Behavioural Variant Frontotemporal Dementia with Bilateral Insular Hypometabolism: A Case Report
Ananya Mahapatra1, Mamta Sood2, Roshan Bhad3, Manjari Tripathi4
1 Senior Resident, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
2 Associate Professor, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
3 Senior Resident, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
4 Professor, Department of Neurology, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ananya Mahapatra, Department of Psychiatry, 4th Floor, Teaching Block, All India Institute of Medical Sciences, Ansari Nagar, East, New Delhi-110029, India.
E-mail: nnyaa09@gmail.com
Fronto-Temporal Dementia (FTD) is a cluster of syndromes, characterized by progressive deterioration of cognition, language and/or behavioural changes associated with degeneration of the frontal and temporal lobes. A 53-year-old man was admitted with a history of gradually progressive behavioural disturbances, disinhibition, unprovoked anger outbursts, apathy, disorganised behaviour and impaired self-care. A clinical diagnosis of Fronto temporal Dementia (behavioural variant) was made. Extensive investigations found no abnormality except in FDG-PET scan of the brain which revealed hypo metabolism in bilateral anterior insular region. Insula is an important brain area implicated in emotional awareness and behaviour control. Hypo metabolism in insular region in the absence of any structural neuroimaging findings, in a case of behavioural variant of Fronto-temporal dementia suggest that, it might be one of the earliest neurobiological changes occurring in this disorder.
FTD, Neuroimaging, Role of insula
Case Report
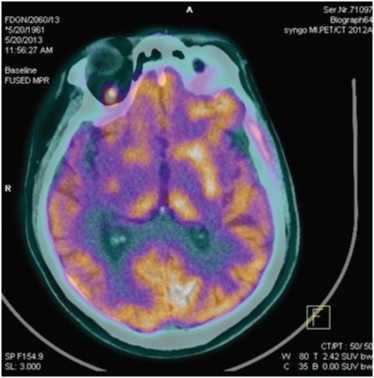
A right handed 53-year-old man presented with 6 years of continuous and gradually progressive illness, initially characterised by decreased interest in household activities, inability to do household chores, decreased interaction, reduced speech output, followed by multiple instances of wandering out of the house aimlessly. He attempted to set himself on fire twice, but would not give any reason for doing so. He would mostly appear apathetic. His self-care was impaired and appetite reduced. He was intermittently violent and aggressive without any provocation. He also would often disrobe himself in front of people. He was found repeating a particular phrase many times, or carrying out stereotypical tapping movements repeatedly. There was no history of seizures, head injury with loss of consciousness, altered sensorium, high grade fever or weight-loss. During a previous admission, patient had been extensively investigated. Routine blood investigations, non-contrast CT brain and CSF examination for cells, sugar, and protein were within normal limit. Patient was brought to our centre following excessive physical aggression and disinhibited behaviour and subsequently admitted. General physical examination did not reveal any abnormality. Patient was apathetic, muttering to self, physically aggressive and uncooperative for interview. Perseveration of particular phrases and stereotyped movements of hands were observed. Patient would pick a comb and repeatedly comb his hair, or try to grab a pen and attempt to write, during interview suggestive of utilization behaviour. He would not show any interest to communicate with the interviewer. During the ward stay, he would frequently disrobe himself in front of others, show unprovoked physical aggression against family members and required physical restraint on multiple occasions. He was not cooperative for a formal neuropsychological assessment. Haemogram, ESR, liver function tests, serum urea/creatinine, C-reactive protein, thyroid function tests, serum folate and serum vitamin B12 levels were within normal range. He screened negative for the viral markers (HIV, HBV and HCV). VDRL was non-reactive. Anti-TPO antibodies were negative. Electroencephalogram and MRI brain (without contrast) were normal. FDG-PET scan of the brain revealed hypo metabolism in the anterior insular region bilaterally [Table/Fig-1].
FDG-PET scan of brain (axial slice at the level of hippocampus and insula) demonstrating bilateral insular hypometabolism.
A provisional diagnosis of behavioural (frontal) variant of fronto-temporal dementia was considered based on his clinical picture. Patient was started on Tab Quetiapine 50 mg, increased up to 300 mg, which reduced his aggression, but did not improve rest of his symptoms. Patient maintained the same over the next 11 months with no improvement in apathy, disorganisation and behavioural symptoms.
Discussion
Fronto-Temporal Dementia (FTD) is a heterogeneous cluster of syndromes, characterized by progressive decline in cognition, behaviour and/ or language associated with degeneration of the frontal and temporal lobes [1]. The behavioural variant of FTD (bvFTD) presents with early disinhibition, apathy, perseverative and stereotyped behaviours and hyper orality. Orbitofrontal and anterior insular cortex have been implicated in the neurobiology of personality and behaviour changes which are characteristically reported in bvFTD [2]. Hypo metabolism in frontal areas, in the absence of structural changes have been reported in bvFTD, but insular hypo metabolism alone in the absence of structural changes in the frontal or temporal regions of patients manifesting with such a clinical picture have not yet been reported. The insula is recently being implicated as a key area involved in emotional awareness and behaviour control. This case highlights the presence of clinical features of bvFTD with only bilateral insular hypo metabolism, without any structural changes.
Present case clinically presented with features of early (within 3 years of onset of illness) disinhibition, apathy, loss of empathy, and perseverative/stereotyped behaviour. From these clinical features it can be conceptualised as a case of “probable” behavioural variant of fronto-temporal dementia, according to the International consensus criteria of 2011 [3]. Only FDG-PET revealed hypo metabolism in anterior insular region bilaterally but no changes were detected on structural neuroimaging. Although atrophy of anterior insular region in structural MRI has been reported in bvFTD [4], insular hypo metabolism in the absence of structural or hypo metabolic changes in frontal cortex has not yet been reported. Behavioural variant of FTD has on rare instances, been found to present with atrophy of the anterior temporal lobe without predominant involvement of the frontal regions [5]. Hypo metabolism on FDG-PET has been detected in frontal brain regions in patients with bvFTD early in the disease process [6]. Jeong et al., analysed FDG-PET findings of 29 cases of FTD and detected hypo metabolism in extensive prefrontal areas, cingulate gyri, anterior temporal regions and bilateral insula [7]. Another study reported hypo metabolism of the frontal lobes, the caudate nuclei, and insula bilaterally when compared to healthy controls [8]. Patients with bvFTD have shown profound deficits in emotions and interpersonal warmth, both specifically linked to right fronto- insular and temporal degeneration [9]. The anterior insular region contains areas which forms strategic links in the speech–language, autonomic, and social–emotional networks [10]. Hence, it could be a potentially important area implicated in the neurobiology of bvFTD. Since structural findings appear later in the course of illness, hypometabolism of insular region, may have been the earliest neurobiological change, observed in this patient. Insula in increasingly being implicated in neural circuits involved with emotional awareness and control; this hypometabolism may reflect the potential aetiology for his behavioural symptoms. However further research is needed to validate these findings.
Conclusion
The insular region is hypothesised to play a potentially important role in human emotional awareness and behavioural guidance networks. With emerging literature, it is also being implicated in the neurobiology of fronto-temporal dementia. Our case presented with the clinical picture of behavioural variant of fronto-temporal dementia, and bilateral insular hypo metabolism as the only neuroimaging finding. The role of insula in mediating the behavioural manifestations of FTD, in the absence of frontal pathology, needs to be explored further to elucidate the neurobiological underpinnings in fronto-temporal dementia.
Consent
Written informed consent was obtained from the patient’s legal guardians for publication of this case report and any accompanying images. A case report is not required Institutional Review Board (IRB) in our institution.
[1]. Rabinovici GD, Miller BL, Frontotemporal Lobar DegenerationCNS Drugs 2010 24(5):375-98. [Google Scholar]
[2]. Riedl L, Mackenzie LR, Förstl H, Kurz A, Diehl-Schmid J, Frontotemporal lobar degeneration: current perspectivesNeuropsychiatr Dis Treat 2014 10(2):297-310. [Google Scholar]
[3]. Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementiaBrain 2011 134(9):2456-77. [Google Scholar]
[4]. Seeley WW, Crawford R, Rascovsky K, Kramer JH, Weiner M, Miller BL, Frontal paralimbic network atrophy in very mild behavioural variant frontotemporal dementiaArch Neurol 2008 65(2):249-55. [Google Scholar]
[5]. Shimizu H, Hokoishi K, Fukuhara R, Komori K, Ikeda M, Two cases of frontotemporal dementia with predominant temporal lobe atrophyPsychogeriatrics 2009 9(4):204-07. [Google Scholar]
[6]. Zhou J, Greicius MD, Gennatas ED, Growdon ME, Jang JY, Rabinovici GD. Divergent network connectivity changes in behavioural variant frontotemporal dementia and Alzheimer’s diseaseBrain 2010 133(5):1352-67. [Google Scholar]
[7]. Jeong Y, Cho SS, Park JM, Kang SJ, Lee JS, Kang E, 18F-FDGPETfindings in frontotemporal dementia: an SPM analysis of 29 patientsJ Nucl Med 2005 46(2):233-39. [Google Scholar]
[8]. Diehl-Schmid J, Grimmer T, Dredge A, Bornschein S, Riemenschneider M, Förstl H, Decline of cerebral glucose metabolism in frontotemporal dementia: a longitudinal 18F-FDG-PET-studyNeurobiol Aging 2007 28(1):42-50. [Google Scholar]
[9]. Agosta F, Canu E, Sarro L, Comi G, Filippi M, Neuroimaging findings in frontotemporal lobar degeneration spectrum of disordersCortex 2012 48(4):389-413. [Google Scholar]
[10]. Seeley WW, Anterior insula degeneration in frontotemporal dementiaBrain Struct Funct 2010 214(5-6):465-75. [Google Scholar]