Is Reactive Dengue NS1Antigen Test a Warning Call for Hospital Admissions?
Sriram Pothapregada1, Banupriya Kamalakannan2, Mahalakshmy Thulasingam3, Srinivasan Sampath4
1 Associate Professor, Department of Paediatrics, Indira Gandhi Medical College and Research Institute, Puducherry, India.
2 Junior Resident, Department of Paediatrics, Indira Gandhi Medical College and Research Institute, Puducherry, India.
3 Assistant Professor, Department of Community Medicine, Indira Gandhi Medical College and Research Institute, Puducherry, India.
4 Associate Professor, Department of Microbiology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sriram Pothapregada, Plot No 7 and 8, Ground Floor, Logu Nagar, PO: Dhanvantri Nagar, Puducherry-605006, India.
E-mail: psriram_ped@yahoo.co.in
Introduction
Dengue fever is a major public health problem worldwide. The 2011 revised World Health Organization (WHO) guidelines have emphasized on early diagnosis and intervention to reduce the case fatality rate due to dengue fever. Rapid diagnostic tests like NS1 antigen assays have improved the detection of cases in early clinical phase of illness but its role as a predictor of severe dengue infection is not very clear.
Aim
To evaluate the utility of NS1 Ag assay as an early diagnostic marker and predictor of severe dengue infection.
Materials and Methods
All children (0-12 years of age) diagnosed and confirmed with dengue fever at a tertiary care hospital in Puducherry between 01st August 2012 and 31st July 2015 were reviewed retrospectively from hospital case records as per the revised WHO guidelines for dengue fever. The diagnosis was confirmed by NS1antigen-based ELISA test or dengue serology for IgM and IgG antibodies and the data were analysed using SPSS 16.0 statistical software. After collecting all the data, all the variables were summarised by descriptive statistics. Categorical variables were expressed as frequencies and percentages, and then analysed by the χ2 test or fishers exact test, where appropriate. Significance was taken at p-value< 0.05.
Results
Among the 261 confirmed cases of dengue fever non-severe dengue and severe dengue infection was seen in 60.9% and 39.1% respectively. The mean age of presentation was 6.9 years and M:F ratio was 1.2:1. NS1 Ag was positive in 217 cases (83.1%) and among them non-severe dengue and severe dengue was seen in 65.9% and 34.1% cases respectively. A total of 44 cases (16.9%) were negative for NS1 Ag assay and positive for IgM MAC ELISA and among them 16 children (36.4%) had non-severe dengue infection where as 28 children (63.6%) had severe dengue infection. Secondary infection with (MAC-ELISA IgG) was seen in 17 cases (6.5%). NS1Ag assay was predominantly positive in acute phase sera, where as IgM/IgG MAC ELISA was predominantly positive in convalescent phase sera. There were six deaths (2.3%) and the common causes of poor outcome were multiorgan failure, encephalopathy and refractory shock.
Conclusion
NS1 Ag assay is a useful early diagnostic marker for dengue fever but cannot be used as an early predictor of severe dengue infection. The criteria for admission in hospitals of cases of dengue fever should be based on clinical warning signs rather than positive NS1 Antigen test.
Early diagnosis, ELISA, Severe dengue, World health organization
Introduction
Dengue fever is the most rapidly spreading mosquito borne viral disease worldwide with an estimated 30-fold increase in incidence over last five decades with unpredictable clinical evolution and outcome. An estimated 5,00,000 people with severe dengue infection require hospitalization annually and 90% of them are children aged less than 5 years of age. Without proper treatment, the case fatality rate in severe dengue is more than 20% and with timely intervention it can be reduced to less than 1% [1].
Dengue virus is a positive stranded, encapsulated RNA virus 11kb in size and has a single Open Reading Frame (ORF) encoding for a single polypeptide which is further processed into three structural proteins, that is the Capsid (C), Membrane (M), and Envelope (E) proteins, and seven non-structural (NS1) proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, NS5) [1]. There are four serotypes of dengue virus (DEN1-4) and the recovery of infection from one serotype can confer life-long protection against that serotype but not against the other three serotypes. Severe dengue infection usually occurs after a second infection with a different serotype, which is due to immune-mediated antibody-dependent enhancement (ADE) [2,3].
The major diagnostic methods currently available are viral culture, viral RNA detection by reverse transcriptase PCR (RT-PCR) and serological tests such as an immunoglobulin M (IgM) capture enzyme-linked immunosorbent assay (MAC-ELISA) but the diagnosis at an early stage of illness still remains a challenge as these diagnostic assays have their own pitfalls [3]. Viral culture assay is the gold standard for diagnosis of dengue fever but it is a time consuming procedure and cannot be used as a routine diagnostic procedure during early stage of illness [4]. Viral RNA detection by reverse transcriptase PCR (RT-PCR) can be used in the diagnosis of dengue infection during the early stage of illness, but requires highly trained staff, sophisticated equipment and the cost factor involved has limited its application as a routine diagnostic assay. The MAC-ELISA, which is commonly used assay, has a low sensitivity in the first four days of illness [5].
Enzyme-Linked Immunosorbent Assays (ELISA) directed against Non-Structural glycoproteins (NS1 Antigen) have demonstrated very high concentrations in the sera of dengue virus infected patients during the early clinical phase of the disease and represents a new approach to the diagnosis of acute dengue infection [6–10]. The focus has shifted to early diagnosis and treatment to reduce the mortality due to severe dengue infection. With the advent of NS1 antigen assay, there has been unprecedented rise in early diagnosis of dengue fever during the first week of illness especially during epidemics but its role as an early predictor of severe dengue infection is not very clear.
The recent epidemics at Puducherry have seen an increase in number of admissions of cases of dengue fever with reactive NS1 antigen. On one hand it has improved intervention at an early stage of illness and on the other hand it has resulted in overburdening of hospitals with dengue fever cases especially during epidemics.
Aim
The objective of this study was to evaluate the utility of NS1 Ag assay as a diagnostic marker as well as an early predictor of severe dengue infection.
Materials and Methods
After approval by the Institute Ethics committee, case records of all children (0-12 years of age) diagnosed and confirmed with dengue fever at a tertiary care hospital at Puducherry between the 1st of August 2012 and January 31st 2015 were reviewed retrospectively from hospital case records. Data was entered in a structured proforma. The case definition, diagnosis and management used for dengue fever were as per the revised World Health Organization (WHO) guidelines 2011 [1]. The diagnosis was confirmed by NS1antigen-based ELISA test (J Mitra kit, India) or dengue serology for IgM for primary dengue infection and IgG antibodies for secondary dengue infection (Kit from National vector born disease control programme Pondicherry and National institute of virology Pune, India) during the acute phase and convalescent phase of illness. Blood samples were collected from children with provisional diagnosis of dengue fever and were screened by both NS1 Ag assay and MAC-ELISA. The performance of NS1 antigen assay in comparison to MAC-ELISA in acute and early convalescent sera and detection rate was evaluated. All other relevant and other additional investigations were done as per the clinical course of illness.
Statistical Analysis
The SPSS 16.0 statistical software was used for data analysis. After collecting all the data, all the variables were summarized by descriptive statistics. Continuous data, expressed as mean+SD, or median (range) wherever appropriate. Categorical variables were expressed as frequencies and percentages, and then analysed by the χ2 test or fishers exact test, where appropriate. Significance was taken at p-value< 0.05.
Results
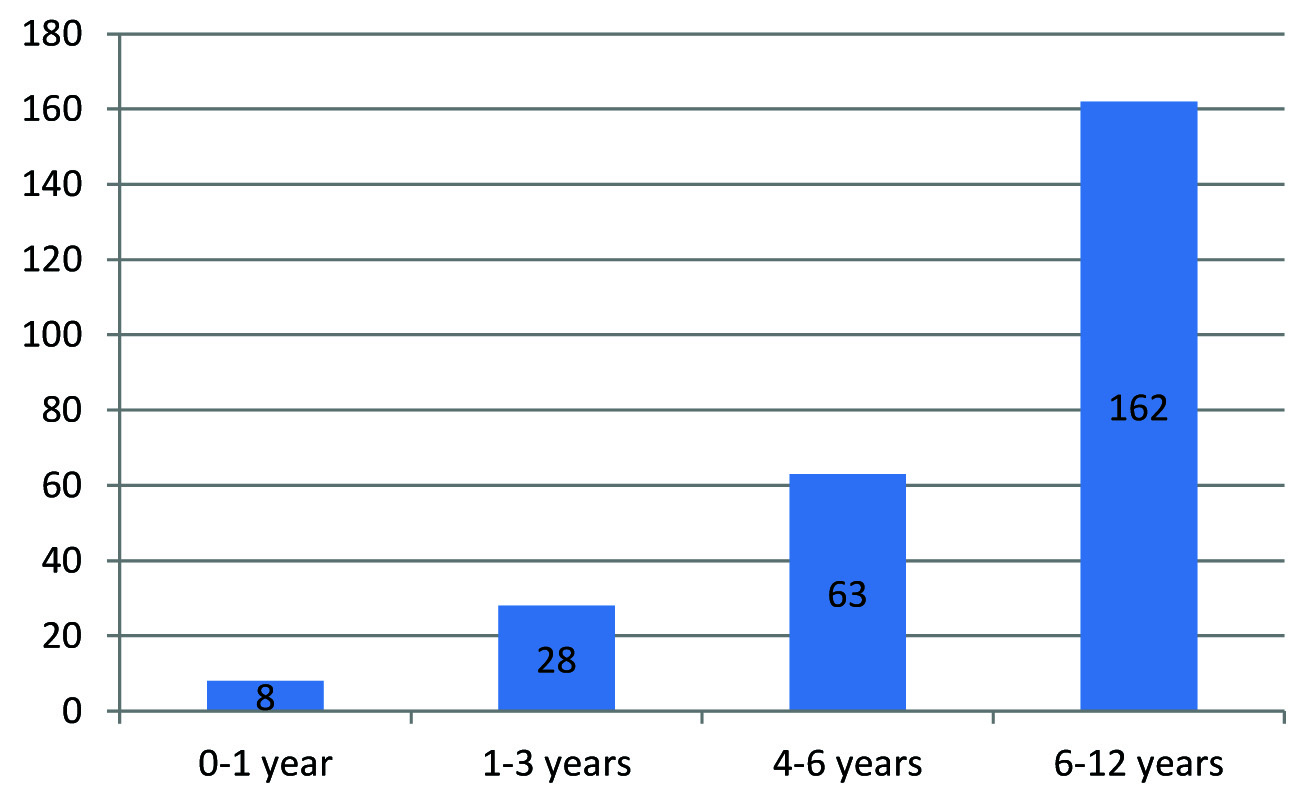
Out of 398 children admitted with dengue fever the diagnosis was confirmed in 261 cases (65.5%). Non-severe dengue infection was seen in 159 cases (60.9%) and severe dengue infection was seen in 102 cases (39.1%). Majority of the cases were from Pondicherry and neighboring states. Mean age of presentation was 6.9 years and 6-12 years was the most common affected age group [Table/Fig-1]. The M: F ratio was 1.2:1.
Age-wise distribution of cases with dengue fever.
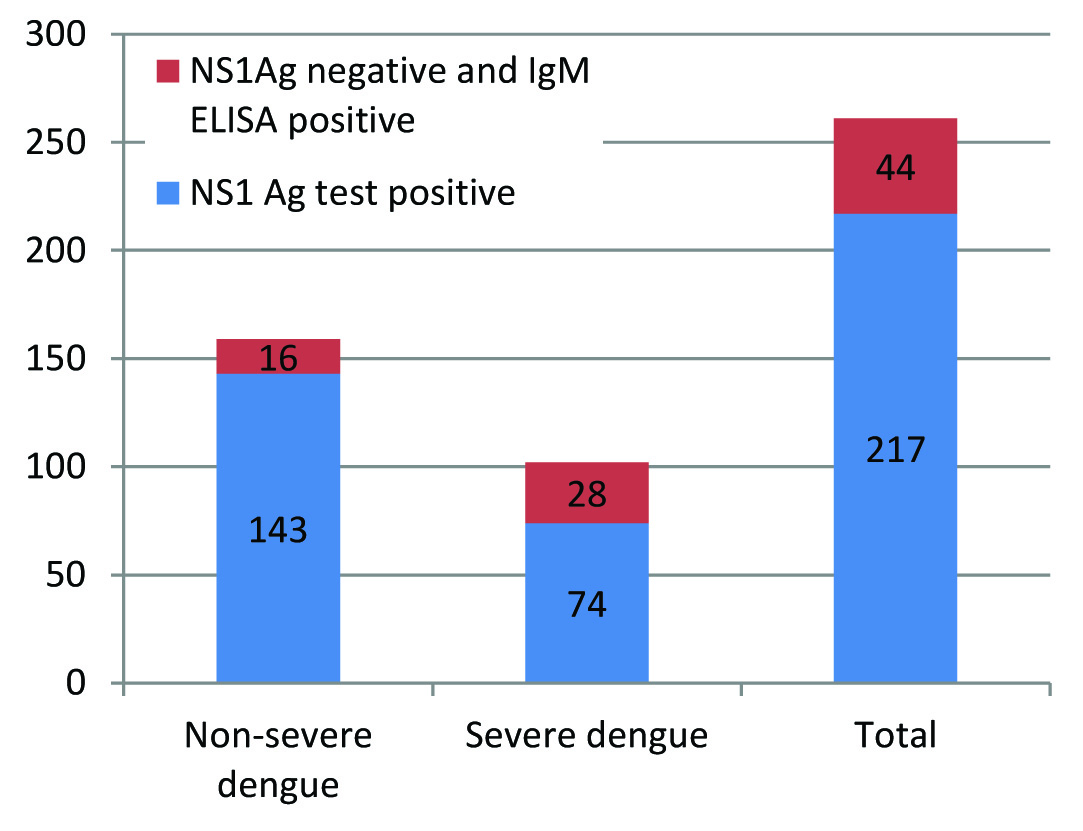
NS1 Ag was positive in 217 (83.1%) cases and among them non-severe dengue and severe dengue was 143 cases (65.9%) and 74 cases (34.1%) respectively [Table/Fig-2]. A total of 44 children (16.9%) were negative for NS1 Ag assay and positive for IgM MAC ELISA and among them 16 children (36.4%) had non-severe dengue infection where as 28 children (63.6%) had severe dengue infection [Table/Fig-2]. A 96 children (36.7%) were positive for both NS1 Ag and IgM MAC ELISA, 17 children were positive for IgG (6.5%) and 13 children (4.9%) were positive for all the three markers. Eleven children with features had clinical features of severe dengue infection with compensated shock and improved with fluid therapy but were neither positive with NS1Ag assay or IgM/IgG ELISA in both acute phase sera nor convalescent phase sera.
Graph shows NS1 Ag test in severe and non-severe dengue infection.
NS1 Ag was predominantly positive in acute phase sera in the first week of illness where as IgM MAC ELISA was predominantly positive in convalescent phase sera and was statistically significant [Table/Fig-3]. IgG MAC ELISA was positive in 4 cases (23.5%) in the acute phase sera and 13 cases (76.5%) in convalescent phase sera. All Children who were positive only for NS1 Ag in the study belonged to acute phase sera and were having non-severe dengue infection.
Comparison of assay results in acute / convalescent sera.
| Blood samples | NS1Ag(+) | NS1Ag-ve & MAC ELISA(+) | Total | p-value |
|---|
| Acute phase sera | 202(93.1) | 4(9.1) | 206(78.9) | <0.001 |
| Convalescent phase sera | 15(6.9) | 40(90.9) | 55(21.1) |
| Total | 217(83.1) | 44(16.9) | 261 | |
Data represented as number (%)
The comparison of NS1Ag assay and IgM MAC ELISA with platelet count is given in [Table/Fig-4]. Platelet count in the range of <20,000/mm3, 20-50,000/mm3 and >50,000/mm3 were seen in 12 (4.6%), 31 (11.9%) and 218 (83.5%) cases respectively. Platelet count>50,000/mm3 was significantly associated with positive NS1Ag assay where as severe thrombocytopaenia (Platelet count<20,000/mm3) was significantly associated with positive IgM ELISA test. The platelet counts were lower among children who were positive for IgM MAC ELISA in comparison to those who were only NS1Ag positive and were statistically significant. Eight children who had platelet count <50,000/mm3 were NS1 Ag negative.
Comparison of NS1 antigen assay and platelet counts.
| Platelet range | NS1Ag +ve | NS1Ag-ve & IgM MAC ELISA +ve | Total | p-value |
|---|
| <10,000/mm3 | 3(1.4) | 4(9.1) | 7(2.7) | <0.001 |
| 10,000-20,000/mm3 | 0(0) | 5(11.4) | 5(1.9) | <0.001 |
| 20,000-50,000/mm3 | 17(7.8) | 14(31.8) | 31(11.9) | <0.001 |
| 50,000-1,00,000/mm3 | 48(22.1) | 10(22.7) | 58(22.2) | <0.001 |
| 1,00,000-1,50,000/mm3 | 105(48.4) | 9(20.5) | 114(43.7) | <0.001 |
| >1,50,000/mm3 | 44(20.3) | 2(4.5) | 46(17.6) | <0.001 |
| Total | 217(83.1) | 44(16.9) | 261(100) | <0.001 |
Data represented as number (%)
Shock was present in 102 cases (39.1%) in children with severe dengue infection and among them significant bleeding was present only in 22 cases (21.6%) and decompensated shock was in 16 cases (15.7%). There was difficulty in classifying them as Dengue haemorrhagic fever as all children did not fulfil the four criteria of fever, thrombocytopaenia, bleeding and plasma leakage. Among the children who were NS1Ag positive 34.1% had features of shock where as among children who were IgM ELISA positive 63.6% had features of shock [Table/Fig-2]. Eleven children presented with features of dengue fever with shock and responded to fluid therapy but were negative for NS1 Ag assay and dengue serology. There were six deaths (2.3%) and among them 5 cases (83.3%) were positive for both NS1Ag and IgM MAC ELISA and four children (66.6%) were positive for IgG MAC ELISA. One child had features of severe dengue infection with multiorgan failure and was NS1Ag test negative but was positive for both IgG and IgM MAC ELISA. The common causes of poor outcome were multiorgan failure, encephalopathy and refractory shock.
Discussion
Dengue fever is a major public health problem with high morbidity and mortality. The revised World Health Organization dengue fever guidelines 2011 have emphasized the need for early diagnosis and treatment to reduce the mortality due to severe dengue infection [1]. The classical methods of confirmation of diagnosis are virus isolation, serotype identification, antibody detection tests (IgM and IgG MAC-ELISA), haemagglutination inhibition or neutralization tests but all these tests are time consuming and do not help in the confirmation of diagnosis at an early stage of illness [2]. The serological diagnosis by IgM/IgG MAC ELISA has been the most common method of confirmation of dengue fever and has sensitivity and specificity of approximately 90% and 98%, respectively but the problem is that it is only detected in the convalescent phase of illness. With the advent of NS1 antigen assay, there has been unprecedented rise in early diagnosis of dengue fever as it develops during the acute phase of illness (0-7 days) and is emerging as a suitable option for dengue diagnosis in the first week of illness with high sensitivity and specificity [3].
In our study the diagnosis of dengue fever was confirmed by NS1 Ag test in 83.1% of cases and among them 93.1% of the cases was detected in the acute phase sera in the first week of illness. IgM MAC ELISA was positive in 16.9% of cases and among them 90.9% of cases was detected in convalescent phase sera. The NS1Ag test was a useful early diagnostic marker for dengue infection in acute phase illness in primary and secondary dengue infection in this study as has been reported with few previous studies [4–6]. The detection of specific IgM by MAC-ELISA is still used as the diagnostic technique but the main disadvantage being it is usually positive during the convalescent phase of illness and as a result a large number of cases go undetected during the acute phase of illness as suggested in the previous studies [7–10]. An NS1 Ag level varies from 0.5-2 μg/ml in acute-phase serum samples, to less than 0.04 μg/ml in convalescent phase serum [11]. The requirement of paired sera, subsequently in convalescent phase, if negative in acute phase also delays diagnosis. There was an increase in sensitivity of detection when both NS1Ag assay and IgM MAC ELISA detection assays were used together in a single sample as reported in previous studies [12–14].
NS1 antigen assay is a useful tool in the diagnosis of dengue infection in the early phase of the disease but it is not clear whether they can be used as an early predictor of the severity of the disease [10,15]. Libraty et al., in their study showed a very high concentration of NS1 antigen during early phase of illness in patients with severe dengue infection and used as an early diagnostic marker for severe dengue infection [16]. However, in our study the predominant mode of presentation in children who were NS1 Ag positive was non-severe dengue infection. The sensitivity of detection of NS1 Ag test in non-severe dengue infection was good. The detection of severe dengue infection by NS1 Ag test and IgM MAC ELISA were 34.1% and 63.6% respectively. NS1 Ag test was not an early predictor of severe dengue infection in this study even though it helped in confirmation of diagnosis at an early stage of illness.
The demerit of NS1 Ag assays are that they are unable to distinguish the serotype of the dengue virus causing infection. Real time and nested RT-PCR is fast becoming the method of choice as it enables rapid detection, serotype identification, as well as viral RNA quantification which are 80-90% sensitive and >95% specific [17]. The DENCO (Dengue and control) study concluded that a positive PCR or positive viral culture, or IgM in paired sera, IgG seroconversion in paired sera or a fourfold IgG titer increase in paired sera in confirmatory for dengue viral infection. The presence of IgM in a single serum sample or IgG in a single serum sample with a haemagglutination inhibition titer of 1280 or higher was considered highly suggestive of dengue viral infection [18]. The addition of an IgM/G component for NS1 testing improves diagnostic sensitivity above NS1 testing alone and probably is the most practical option for the diagnosis of dengue infection [19–22].
In our study, there was an increase in early detection of dengue infection with the help of NS1Ag rapid diagnostic test, but we also witnessed traumatized and panic-struck parents putting unnecessary pressure on the treating paediatricians for hospitalization in children who were NS1 Ag test positive. Hence, the real need of the hour especially for the treating physicians is to recognize the early warning signs in children with dengue fever and it should remain the only indicator for admission rather than positive results in rapid diagnostic tests like NS1 Ag assay. It is also important for the treating physicians to counsel the panic struck parents and educate them regarding home care treatment and identification of symptoms and danger signs and bring the child to immediate medical attention should the need arise especially during epidemics.
Limitation
There are several limitations to the present study. The study is retrospective analysis of dengue fever cases from a single centre and included only those cases which were admitted to the hospital. The diagnosis was confirmed by either NS1Ag test or dengue serology. Virus isolation and serotype identification was not done in the present study. There were cases which behaved like dengue fever but remained undiagnosed due to lack facilities for other confirmatory tests. A larger multicentric prospective study having a larger sample size would be ideal.
Conclusion
NS1 Ag assay is useful, sensitive and specific for the diagnosis of dengue infection, especially during the acute phase when antibodies are not detectable and the dengue serology was negative. Early diagnosis and timely intervention can reduce the mortality due to severe dengue infection. However from our experience it cannot be used as an early predictor of sever dengue infection and the criteria for admission in hospitals of cases of dengue fever should be based only on clinical warning signs rather than NS1 Ag positive reports.
Data represented as number (%)
Data represented as number (%)
[1]. World Health Organization, Regional Office for South-East Asia. Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Hemorrhagic fever, Revised and expanded edition. WHO-SEARO 2011. (SEARO Technical Publication Series No 60) [Google Scholar]
[2]. Guzman MG, Kouri G, Dengue: an updateLancet Infect Dis 2002 2:33-42. [Google Scholar]
[3]. Chakravarthi A, Kumaria R, Batra VV, Verma V, Improved detection of dengue virus serotypes from serum samples-Evaluation of single-tube multiplex RT-PCR with cell cultureDengue Bulletin 2006 30:133-40. [Google Scholar]
[4]. Xu H, Pan YX, Qiu LW, Wang YD, Hao W, He LJ, Serotype 1-specific monoclonal antibody-based antigen capture immunoassay for detection of circulating nonstructural protein NS1: implications for early diagnosis and serotyping of dengue virus infectionsJ Clin Microbiol 2006 44:2872-78. [Google Scholar]
[5]. Thomas L, Najioullah F, Verlaeten O, Martial J, Brichler S, Kaidomar S, Relationship between nonstructural protein 1 detection and plasma viral load in dengue patientsAm J Trop Med Hyg 2010 83:696-99. [Google Scholar]
[6]. Sekaran SD, Lan EC, Mahesawarappa KB, Appanna R, Subramanian G, Evaluation of a dengue NS1 capture ELISA assay for rapid detection of dengueJ Infect Developing Countries 2007 1:182-88. [Google Scholar]
[7]. Shu PY, Huang JH, Current advances in dengue diagnosisClinical and Diagnostic Laboratory immunology 2004 11:642-50. [Google Scholar]
[8]. Alcon S, Talarmin A, Debruyne M, Falconar A, Duebel V, Flammand M, Enzyme linked immunosorbent assay specific to dengue virus type 1 nonstructural protein ns1 reveals circulation of the antigen in the blood during acute phase of the disease in patients experiencing primary or secondary infectionsJ Clin Microbiol 2002 40:376-81. [Google Scholar]
[9]. Dussart P, Labeau B, Lagathu G, Louis P, Nunes MRT, Rodrigues SG, Evaluation of an Enzyme Immunoassay for detection of dengue virus NS1 antigen in human serumClin Vaccine Immunol 2006 13:1185-89. [Google Scholar]
[10]. Datta W, Wattal C, Dengue NS1 antigen detection test: A useful tool in early diagnosis of dengue virus infectionIndian J Med Microbiol 2010 28:107-10. [Google Scholar]
[11]. Bessof K, Delorey M, Sun W, Hunsperger E, Comparison of two commercially available dengue virus (denv) ns1 capture enzyme-linked immunosorbent assays using a single clinical sample for diagnosis of acute denv infectionClin Vaccine Immunol 2008 15:1513-18. [Google Scholar]
[12]. Kumarasamy V, Wahab AHA, Chua SK, Hassan Z, Chem YK, Mohamed M, Evaluation of a commercial dengue NS1 antigen-capture ELISA for laboratory diagnosis of acute dengue virus infectionJ Virol Methods 2007 140:75-9. [Google Scholar]
[13]. Young PR, Hilditch PA, Blectchy C, Halloran W, An antigen capture enzyme-linked immunosorbent assay reveals high levels of dengue virus protein NS1 in the sera of infected patientsJ Clin Microbiol 2000 38:1053-57. [Google Scholar]
[14]. Xu H, Pan YX, Qiu LW, Wang YD, Hao W, He LJ, Serotype 1-specific monoclonal antibody-based antigen capture immunoassay for detection of circulating nonstructural protein NS1: implications for early diagnosis and serotyping of dengue virus infectionsJ Clin Microbiol 2006 44:2872-78. [Google Scholar]
[15]. Henchal EA, McCown JM, Sequin MC, Gentry MK, Brandt WE, Rapid identification of dengue virus isolates by using monoclonal antibodies in an indirect immunoflourescent assayAm J Trop Med Hyg 1983 32:164-69. [Google Scholar]
[16]. Libraty DH, Young PR, Pickering D, Endy TP, Kalayanarooj S, Green S, High circulating levels of the dengue virus nonstructural protein NS1 early in dengue illness correlate with development of dengue haemorrhagic feverJ Infect Dis 2002 186:1165-68. [Google Scholar]
[17]. Kong YK, Chong HT, Tan CT, Devi S, Rapid detection, serotyping and quantification of dengue viruses by TaqMan real-time one-step RT-PCRJ Virol Methods 2006 138:123-30. [Google Scholar]
[18]. Basuki PS, Budiyanto A, Puspitasari D, Husada D, Darmowandowo W, Ismoedijanto Application of revised dengue classification criteria as a severity marker of dengue viral infection in IndonesiaSoutheast Asian J Trop Med Public Health 2010 41:1088-94. [Google Scholar]
[19]. Charkavarthi A, Kumar A, Malik S, Detection of dengue infection by combining the use of an NS1 antigen based assay with antibody detectionSoutheast Asian J Trop Med Public Health 2011 42:297-302. [Google Scholar]
[20]. Ampaiwan C, Wathanee C, Viroj P, Kanchana T, Sarapee L, Sutee Y, The use of Nonstructural protein 1 antigen for the early diagnosis during the febrile stage in patients with dengue infectionJ Paed Infect Dis 2008 27:43-48. [Google Scholar]
[21]. Kittigul L, Pitakarnjanakul P, Sujirarat D, Siripanichgon K, The differences of clinical manifestations and laboratory findings in children and adults with dengue virus infectionJ Clin Virol 2007 39(2):76-81. [Google Scholar]
[22]. Arya SC, Agarwal N, Parikh SC, Agarwal S, Simultaneous Detection of Dengue NS1 Antigen, IgM plus IgG and Platelet Enumeration during an OutbreakSultan Qaboos Univ Med J 2011 11(4):470-76. [Google Scholar]