Lung cancer is one of the most common malignancies with high mortality, 13% of all new cancer cases and 19% of cancer related deaths worldwide are due to lung cancer. A 6.9% of all new cancer cases and 9.3% of all cancer related deaths in India are due to lung cancer. The 5 year survival rate is only 15% in the developed countries and a dismal 5% in the developing countries [1].
There is an alarming increase in the incidence of lung cancers in women and consequently it’s mortality in USA, which has been attributed to rise in smoking trends in US women in 1970s [1].
The majority of the lung cancers among non-smokers occur in women. The possible factors which have been thought to be responsible for this are: infections, hormones, geographic, cultural and genetic differences [2].
Bronchoscopy is a safe and effective means of diagnosing bronchogenic carcinoma with varying diagnostic yield. Various bronchoscopic procedures include bronchial washings, brush cytology, bronchial biopsy, transbronchial needle aspiration (TBNA) & bronchioalveolar lavage (BAL). It has been shown that a combination of various histological & cytological procedures have significantly increased the overall yield of diagnostic bronchoscopy in the management of lung cancers [3].
The size & location of the lesion, sampling technique, physicians’ level of experience, retrieval & processing of specimen being the determinants of variable yield [4]. The British Thoracic Society (BTS) guidelines for diagnostic bronchoscopy recommend the use of combination of various bronchoscopic procedures to increase the yield in lung malignancies [5].
The CB (CB) prepared by embedding the residue in a paraffin block has been mentioned in the literature to harness tissue/cells shed in the pleural fluid, bronchial washings and irrigation of the needles used for fine needle aspiration cytology [6]. Various studies have observed increase in the diagnostic yield using CB of cytological specimen when compared with smear cytology alone [6]. However, there are fewer studies comparing the usefulness of CB of bronchial washings with smear cytology of bronchial washings till date [7]. Hence we decided to compare the diagnostic yield of CB of bronchial washings with the conventional smear cytology obtained during flexible bronchoscopy.
Materials and Methods
The present study is a prospective analytical study. An Institutional Ethics Committee approval was obtained for this study. All patients of suspected bronchogenic carcinoma admitted in the Department of Pulmonary Medicine, Goa Medical College, from August 2011 to September 2013, were included in this study and underwent flexible video-bronchoscopy as per standard BTS protocol [5].
Patients having clinical and radiological features which suggested an underlying lung malignancy were included in this study. Bronchial biopsy, brushings & washings were collected. The bronchial washings obtained in a mucus trap were divided into two aliquots. The aliquots were processed differently, one by preparing smears conventionally and other by preparation of CB. The bronchial washings obtained were centrifuged in a cold-centrifuge at 4000 rpm for 6 min.
Smearing technique: Immediately after centrifuging, the supernatant fluid was drained off. Two to four smears were then prepared immediately. Slides were then fixed in fixative containing 50% ethanol + formalin and sent for pathological examination.
Cell-blocking: The supernatant fluid was decanted. The residual cell pellet which was left was fixed in freshly prepared Bouin’s Solution (Saturated picric acid + glacial acetic acid + formalin) which was followed by processing & embedding the cell pellet in a paraffin block. These were later stained with routine H&E staining.
Method of analysis: CB and smears thus prepared were further processed & examined by two different pathologists from Department of Pathology, Goa Medical College, independently. Results were tabulated and analysed to evaluate the diagnostic efficacy of CB & compared it with conventional smear cytology (CS) of bronchial washings specimen.
Results
A total of 104 cases were included in this study of which 92 were confirmed as malignancy by bronchoscopy. The remaining 12 cases were diagnosed by one of the following tests viz., pleural fluid cytology, cervical lymph node FNAC/excision biopsy or transthoracic needle aspiration of pulmonary or pleural masses under USG or CT scan guidance. The bronchoscopy was normal in all these 12 cases.
The age of the patients ranged from 35 years to 80 years with a mean of 61.7 years; the same being 60.5 years and 60.8 years for males & females respectively. There were 77 males (74%) and 27 were females (25.96%) in the present study. The male:female (M:F) ratio of 3.5:1.
Endobronchial growth was seen in 70 cases, followed by mucosal irregularity in 53 cases & concentric narrowing in 17 cases. Some patients had more than one finding. The diagnostic yield of various bronchoscopic procedures is shown in [Table/Fig-1].
Diagnostic yield for various bronchoscopic procedures.
| BRONCHOSCOPIC PROCEDURES | DIAGNOSTIC YIELD |
|---|
| No. | % |
|---|
| Endobronchial Biopsy (EB) | 60 | 57.69 |
| Bronchial Brushings (BB) | 51 | 49.03 |
| Bronchial Washings – Smears (CS) | 38 | 36.53 |
| Bronchial Washings – CB (CB) | 46 | 44.23 |
The diagnosis was obtained by CB technique in 8 more patients in whom corresponding smears were negative. Diagnosis was exclusively obtained only by CB of bronchial washings in 2 cases meaning all the other three procedures viz., endobronchial biopsy (EB), brush biopsy (BB) and conventional smear (CS) were negative for malignancy in these two cases. The cumulative diagnostic yield when all these 4 bronchoscopic sampling techniques were considered was 88.46%.
The flexible brochoscopy has been taken as the gold standard test in order to calculate the sensitivity, specificity, positive predictive value, negative predictive value, percentage of false positive rates and percentage of false negative rates.
The sensitivity of endobronchial biopsy (EB), brush biopsy (BB), conventional smear (CS) and CB was 65.22, 55.43, 41.3 and 50 percent respectively [Table/Fig-2,3,4 and 5].
Comparison of endobronchial biopsy with cumulative yield of bronchoscopy (gold standard).
| Test | FOB proven cyto/histology | Total |
|---|
| Positive (No) | Negative (No) |
|---|
| Endobronchial Biopsy | Positive (No) | 60 | 0 | 60 |
| Negative (No) | 32 | 12 | 44 |
| Total | 92 | 12 | 104 |
Comparison of brush biopsy with cumulative yield of bronchoscopy.
| Test | FOB proven cyto/histology | Total |
|---|
| Positive (No) | Negative (No) |
|---|
| Endobronchial Brush Biopsy | Positive (No) | 51 | 0 | 51 |
| Negative (No) | 41 | 12 | 53 |
| Total | 92 | 12 | 104 |
Comparison of conventional smear with cumulative yield of bronchoscopy.
| Test | FOB proven cyto/histology | Total |
|---|
| Positive (No) | Negative (No) |
|---|
| Conventional smear | Positive (No) | 38 | 0 | 38 |
| Negative (No) | 54 | 12 | 66 |
| Total | 92 | 12 | 104 |
Comparison of CB with cumulative yield of bronchoscopy.
| Test | FOB proven cyto/histology | Total |
|---|
| Positive (No) | Negative (No) |
|---|
| CB | Positive (No) | 46 | 0 | 46 |
| Negative (No) | 46 | 12 | 58 |
| Total | 92 | 12 | 104 |
The specificity of endobronchial biopsy (EB), brush biopsy (BB), conventional smear (CS) and CB (CB) was 100 percent [Table/Fig-2,3,4 and 5]. The positive predictive value of endobronchial biopsy (EB), brush biopsy (BB), conventional smear (CS) and CB (CB) was 100%. The negative predictive value of endobronchial biopsy (EB), brush biopsy (BB), conventional smear (CS) and CB (CB) was 27.27, 22.64, 18.18 and 20.7 respectively. The percentage of false positive rates was nil for all the four procedures. The % of false negative rates for endobronchial biopsy (EB), brush biopsy (BB), conventional smear (CS) and CB (CB) was 34.78, 44.57, 58.7 and 50 percent respectively [Table/Fig-2,3,4 and 5].
Squamous cell carcinoma was the commonest histological subtype in the present study. There were 41 cases (39.42%) of squamous cell carcinoma while 18 cases (17.3%) of adenocarcinoma were identified. Unclassified/ Poorly differentiated carcinoma was noted in 38 cases (36.53%) followed by small cell carcinoma in 7 cases (6.73%)
The diagnostic yield was highest (77.14%), with a forceps biopsy when an endobronchial growth was present, whereas the yield on account of bronchial brushings & washings (conventional smears) were almost the same in this group i.e. 42.85% and 41.42% respectively [Table/Fig-6].
Comparing the yield of various techniques in presence or absence of endo-bronchial growth.
| PROCEDURE | ENDOBRONCHIAL GROWTH (n=70) | NO ENDOBRONCHIAL GROWTH (n=34) |
|---|
| No. | % | No. | % |
|---|
| Biopsy | 54 | 77.14 | 6 | 17.64 |
| Brushings | 30 | 42.85 | 21 | 61.76 |
| Washings- CS | 29 | 41.42 | 9 | 26.47 |
| Washings- CB | 38 | 54.28 | 8 | 23.52 |
However in the same group, when the washings were processed by CB technique, the diagnostic yield was 54.28% which was significantly higher when compared with the yield when the smears were prepared by conventional smears of bronchial washings (41.42%).
When no intrabronchial growth was seen during bronchoscopy and the bronchoscopic findings were mucosal irregularity, concentric narrowing or normal bronchoscopy, the various diagnostic procedures were evaluated.
There was no statistical difference in the diagnostic yield between conventional smears and CB technique (chi square= 0.212, p>0.05). This was observed irrespective of whether an intra-bronchial growth was present or not.
The diagnostic yield obtained by washings-smear and CB were comparable when no endobronchial growth was seen. Interestingly, it was observed that in this group, highest diagnosis was obtained with bronchial brushings with a diagnostic yield of 61.76%.
The yields of bronchial washings-CB & bronchial washings-smears were then compared in combination to bronchial biopsy. It was noted that when bronchial washings-CB (CB) was combined with bronchial biopsy, the yield increased in both the groups.
In the presence of an endo-bronchial lesion, the diagnostic yield of endobronchial biopsy (EB) was shown to improve from 77.14% to 88.57% by supplementing CB of bronchial washings whereas washings- conventional smears increased the yield from 77.14% to 80% only in the same group [Table/Fig-7].
Comparing the results of CB & smears with biopsy.
| PROCEDURE | ENDOBRONCHIAL GROWTH (n=70) | NO ENDOBRONCHIAL GROWTH (n=34) |
|---|
| No. | % | No. | % |
|---|
| Biopsy | 54 | 77.14 | 6 | 17.64 |
| Biopsy + BW- CS | 56 | 80.00 | 10 | 29.41 |
| Biopsy + BW- CB | 62 | 88.57 | 9 | 26.47 |
When there was no growth noted intra-bronchially, the combined yield of forceps biopsy with washings- smear and CB were 29.41% & 26.47% respectively.
Discussion
The yield of our study was comparable to the other studies with high yield despite the non-availability of fluoroscopy in our department. It should be emphasised that efforts were made to develop an excellent liaison with the Department of Pathology to ensure optimal processing of specimen obtained by bronchoscopy and efficient reporting of results.
Also, the routine use of CB of bronchial washings in addition to the CS served as a diagnostic aid in supplementing diagnosis of forceps biopsy and brush cytology. All the samples were processed on site and then transported to pathology department for further processing. Selection of patients of suspected bronchogenic carcinoma for bronchoscopy also had an impact on the overall yield in these patients.
Since the introduction of the CB technique by Bahrenburg nearly a century ago, it has been used routinely for processing fluids [8]. In 1928, Zemansky concluded that the CB method was superior to the conventional smear (CS) technique [9]. CB preparations of bronchial washings play an important role in recovery of cellular material for further histopathological study. Studies have shown improvement in the diagnostic yield by CB preparations when compared with smear cytology [6]. Various methods for preparing paraffin embedded CB from fine needle aspiration cytology have been reported [10,11]. These methods mainly include direct transfer of all centrifuged cellular material wrapped in lens paper [12] or embedding in plasma [13,14] or agar [15] and then processing as a routine histological specimen.
Musso C et al., has described an easy one step method of CB preparation after fine needle aspiration. The results demonstrated that the amount and quality of material obtained in the cotton wool tip is similar to that in the traditional CB obtained from the pellet after centrifugation of aspirated fluid [16].
Wide range of histologic fixatives have been used for CB, primarily buffered formalin, neutral buffered formaldehyde solution, 10% buffered formalin, Bouin solution, picric acid fixative, carnoy fixative and ethanol [10,17,18]. CB techniques can be of value to anatomic pathologists when analysing cytology specimens by enabling microscopic evaluation that can mimic histology. Calabretto et al., and Flint et al., demonstrated increase in diagnostic yield when CB of bronchial washings was combined with smears [6,19]. Collin et al., in his study concluded that there is an improvement in the diagnostic yield when CB of bronchial washings was used along with conventional smears of bronchial washings [20].
The present study compares favourably with the other similar studies in the literature viz. Calabretto et al., Flint et al., Collins et al., [Table/Fig-8] [6,19,20]. In the present study we have observed that CB of bronchial washings enhanced the overall yield of bronchoscopy as compared to conventional smears of bronchial washings. The increase in the yield of CB of bronchial washings was 9% when compared to conventional smears. Also it was observed that using a combination of forceps biopsy (EB), brush cytology (BB), washings-smears (CS) and CB (CB) increased the diagnostic yield of bronchoscopy in lung malignancies. Though the quantitative yield on account of CB technique was not statistically significant, the use of CB of bronchial washings was found to be cost-effective and helped in complementing diagnosis in addition to conventional smears of bronchial washings. CB can also be useful in the evaluation of cytoarchitecture and micro-biopsies, as well as for performing special stains and immunohistochemistry, which is not possible with conventional smears.
Yield of CB in various studies.
| Sr.No. | Authors nameyear | Type ofFluid | Outcome of the study |
|---|
| 1. | Flint et al., [19]/1993 | Bronchialwashings | Increase in yield by 9% whencombined with smears. |
| 2. | Calabretto et al., [6] /1996 | Bronchialwashings | Increase in yield by 6.6% whencombined with smears. |
| 3. | Collins et al., [20] /2012 | Bronchialwashings | Improvement of yield with CB. |
| 4. | Present study | Bronchialwashings | Increase in yield of CB by 9%when compared with smears. |
Conclusion
Cell-Block method is easy to perform and no expertise is required to handle the specimen. This processes the minute amounts of cellular material and eases the diagnosis of tumour when reviewed along with cytological smears. In limited resource settings, CB preparation is a simple method that increases diagnostic yield, is cost-effective & hence can be routinely used.
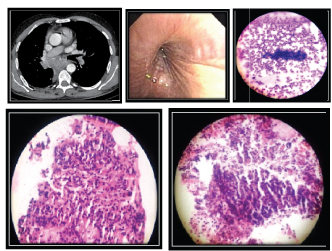
Case 1
Case 1 shows a left hilar mass which showed a presence of an endobronchial growth on bronchoscopy. Diagnosis was confirmed with forceps biopsy showing small cell. [Table/Fig-9] shows visible cell pellet after centrifuging bronchial washings which were used to prepare smears and CB. CB of bronchial washings was positive for malignancy in this case where corresponding bronchial washings smear was negative for malignancy.
(a) CECT- Thorax showing left Hilar mass. (b) Bronchoscopy showing presence of an endobronchial growth. (c) Visible cell pellet after centrifuging washings (d) Biopsy positive for Small cell Carcinoma (e) Bronchial washings cellblock positive for Small cell carcinoma (f) Bronchial washings smear negative for Malignancy
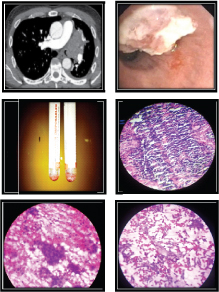
Case 2
Case 2 shows a right Hilar mass which showed concentric narrowing of right main bronchus with no intra-bronchial growth on bronchoscopy. Diagnosis was confirmed with brush cytology showing squamous cell carcinoma. CB of bronchial washings as well as corresponding smears was positive for malignancy in this case [Table/Fig-10].
(a) CECT- Thorax showing Right Hilar mass (b) Concentric narrowing of right bronchus (c) Brush cytology positive for SCC (d) Bronchial washings cellblock positive for SCC (e) Bronchial washings smear positive for Sq cell Ca