Non Aggressive Mandibular Osteoblastoma– A Rare Maxillofacial Entity
Rajat G. Panigrahi1, Sanat K. Bhuyan2, Abhishek R. Pati3, Smita R. Priyadarshini4, Snigdha Sagar5
1 Associate Professor, Department of Oral Medicine and Radiology, Institute of Dental Science, Siksha O Anusandhan University, Bhubaneswar, Odisha, India.
2 Professor and Head of Department, Department of Oral Medicine and Radiology, Institute of Dental Science, Siksha O Anusandhan University, Bhubaneswar, Odisha, India.
3 Assistant Professor, Department of Oral Medicine and Radiology, Institute of Dental Science, Siksha O Anusandhan University, Bhubaneswar, Odisha, India.
4 Assistant Professor, Department of Oral Medicine and Radiology, Institute of Dental Science, Siksha O Anusandhan University, Bhubaneswar, Odisha, India.
5 Post Graduate, Department of Oral Medicine and Radiology, Institute of Dental Science, Siksha O Anusandhan University, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajat G. Panigrahi, N- 5 / 24, IRC Village, Bhubaneswar, Odisha - 751015, India. E-mail : adrrajat@gmail.com
Benign osteoblastoma is a very rare, bone tumour occurring in the facial region. These lesions are most frequently seen in long bones. They are characterised by proliferation of compact or cancellous bone. The lesion is usually asymptomatic until it causes significant facial asymmetry or displacement of the teeth if present in the alveolar region. The clinical appearance of osteoblastoma is very similar to peripheral ossifying fibroma or any fibro-osseous lesion. The tumour is characterised by bone formation along with the presence of numerous osteoblasts. This case report describes the presence of a bony hard mass in the right side of mandible of a 27-year-old female patient with the chief complaint of a painless growth since past 10 years. The growth slowly increased in size displacing the teeth associated with it. The patient also complained of difficulty in speech and mastication.
Alveolus, Bone tumour, Mandible, Teeth displacement
Case Report
A 27-year-old female patient reported to the Department of Oral Medicine and Radiology, with the chief complaint of a growth in right lower back teeth region since 10 years. Nothing is suggestive of the family’s and dental history and medical history. History of present illness revealed that the patient noticed a growth since 10 years in right lower back teeth region, which had been growing to attain the present size. Teeth associated with the growth inclined buccally causing malocclusion on the right side. On intraoral inspection, single localised growth was present in the right lower jaw measuring roughly about 2cm x 4cm in its greatest dimension, irregular in shape and lobulated surface, overlying mucosa was not errythmatous with well defined margins. The growth extended from the mesial aspect of 42 anteriorly to medial aspect of 46 posteriorly [Table/Fig-1,2].
Intra oral picture shows the labial aspect of the lesion with displacement of 44,45 and 46.
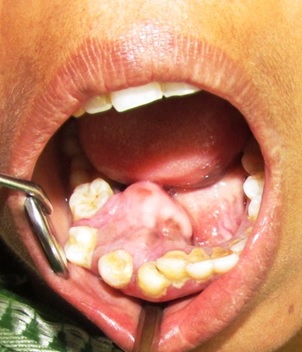
Intra oral picture shows the lingual aspect of the tumour extending from the alveolar region with lobulated surface.

On intra oral palpation the inpectory findings of site, size, shape and extensions were confirmed. The growth was non tender, firm and hard in consistency with lobulated surface, edges were well defined, surrounding structures were normal, it did not yield to pressure, mucosa over the growth was normal inconsistency, base was sessile, non compressible, non reducible. Grade I mobility irt 44 45 & 46 was present.
Based on the clinical findings a provisional diagnosis of benign bony neoplasm was given. The differential diagnosis included Peripheral ossifying fibroma, Peripheral ameloblastoma, tori and osteoma.
Intra Oral Periapical radiograph revealed a radiopaque mass present in the alveolar region extending till the coronal aspect of the premolars and complete loss of lamina dura in rel to 45 and partial loss of lamina dura in relation to 44 and 46 [Table/Fig-3].
IOPA shows a radioapaque mass with displacement of the 43, 44, and 45.

The Mandibular Occlusal radiograph revealed radiopaque radiolucent lesion in the lingual aspect of mandible displacing teeth in buccal aspect in relation to 43 44 45 [Table/Fig-4].
Occlusal Radiograph of mandible shows radiopaque mass originating from the alveolar region and extending to the lingual aspect with the displacement of the teeth in rel to 43 44 45.

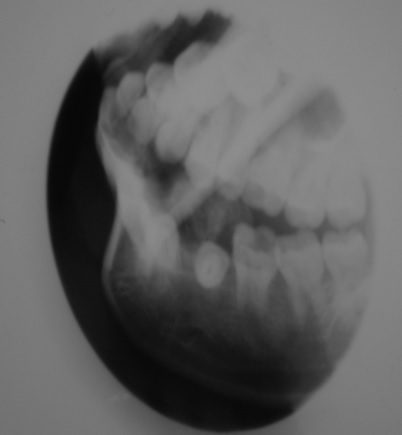
The Orthopantamograph and Lateral Oblique radiograph revealed a radiopaque radiolucent lesion in the right side measuring 2cm x 4cm of ill defined margins displacing the teeth from its original position at 43 44 45 [Table/Fig-5,6].
OPG shows a radio opaque mass in the right mandibular region in rel to 43 44 45.

Lateral oblique shows a radiopacity in the right mandibular region in rel to 43 44 45.
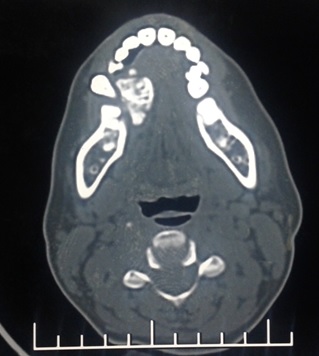
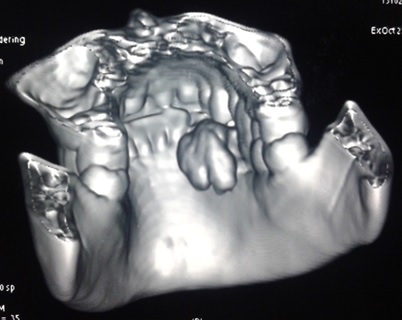
CT face with 3D Reconstruction revealed a hyper dense bony outgrowth about 22 x 14 mm in size arising from right hemimandible at right lower first and second premolar on lingual aspect with small pedicle [Table/Fig-7,8].
CT shows a well defined hyper dense mass with displacement of adjacent teeth.
3 Dimensional CT shows a well defined lobulated mass in the lingual aspect in the right mandibular region.
The insicional biopsy was done was under local anaesthesia. The histopathology report revealed numerous irregular bony trabeculae lined by osteoblasts; the connective tissue contains few dilated capillaries engorged with RBC. Irregular bony trabeculae also contained embedded osteocytes in the lacunae. Few areas also showed lamellar pattern of bony arrangement. Histopathological diagnosis revealed features suggestive of benign osteoblastoma [Table/Fig-9,10,11 and 12].
Incisional Biopsy specimen

The H&E stained section (4X) shows irregular bony trabeculae lined by osteoblasts. The loose connective tissue contains few dilated capillaries.
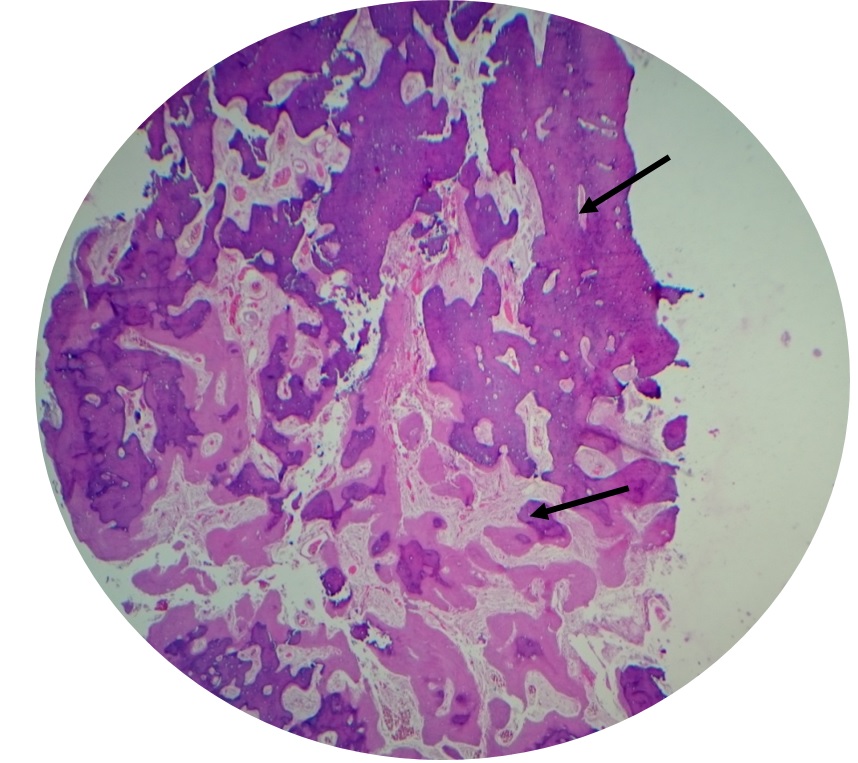
The H&E stained section (10X) shows presence of osteocytes. The bony trabeculae shows increased osteoblastic and osteoclastic activity. It also shows dialated capillaries.
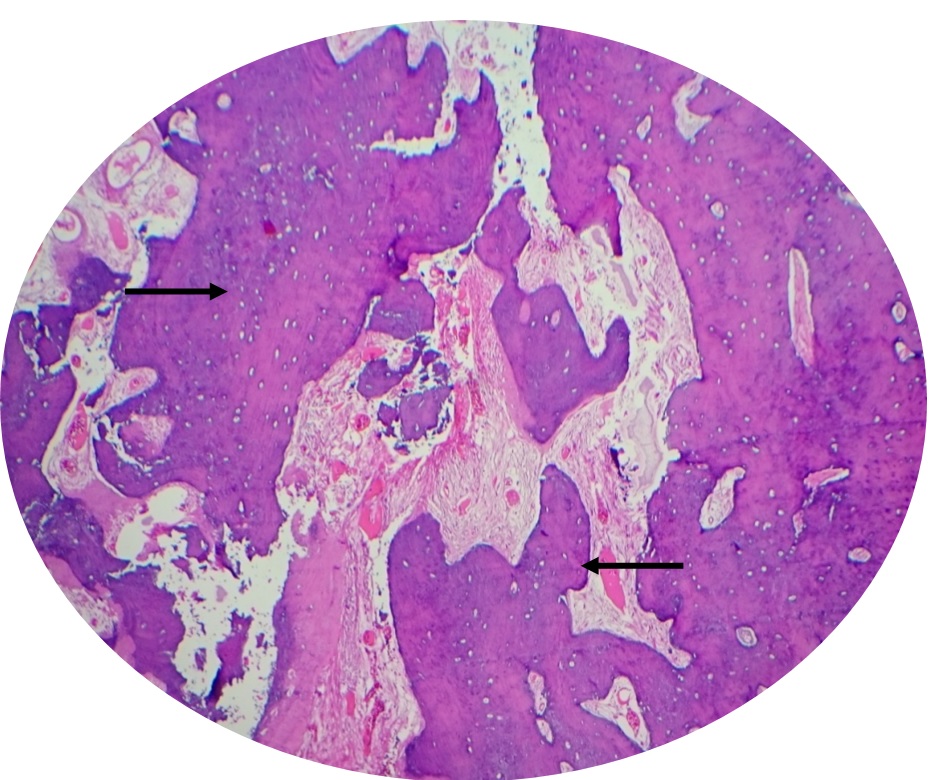
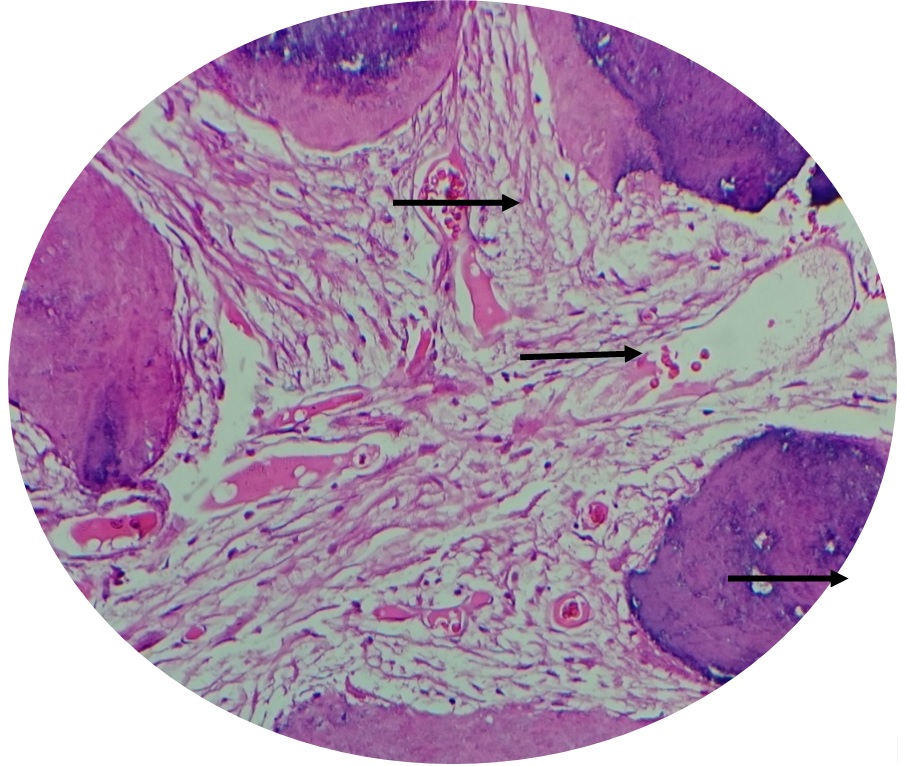
The H&E stained section (40X) shows loose fibrillar connective tissue with blood vessels engorged with RBCs. Irregular bony trabeculae also contains embedded osteocytes in the lacunae. Few areas also showing lamellar pattern of bony arrangement.
Based on the clinical diagnosis and investigative findings a final diagnosis of benign osteoblastoma was given. Patient was referred to the Department of Oral and Maxillofacial Surgery for further further treatment of the tumour. The patient was then explained in detail about the surgery and consent was taken. Traphezoidal mucoperiosteal flap on buccal aspect was raised. Marginal mandibulectomy was done extending from 41 region to 46 region. Overlying lingual mucosa was excised along with the tumour. The bony defect was allowed for secondary healing. The suturing was done with 3.0 vicryl sutures.
Medications: Amoxicillin 1gm I.V BD, Metronidazole I.V TID, Diclofenac I.M BD was administered for 5 days. Chlorhexidine mouth wash was prescribed for maintaining the oral hygiene. Patient was recalled after 3 months of surgery and an orthopantamograph was taken to evaluate the presence of any radiographic evidence to ascertain the presence of the lesion. The patient was then referred to the Department of Prosthodontia for oral rehabilitation [Table/Fig-13,14,15 and 16].
Intraoperative picture showing resection of the growth.

Specimen shows complete removal of the lesion along with the involved teeth.

Post surgical follow up picture of the mandible.

Post surgical OPG shows an edentulous area in relation to 42 43 44 45 46.

Discussion
Osteoblastoma is a rare entity arising from osteoblasts. The mandible is affected more often than the maxilla and mostly in the body of mandible. Mostly it is diagnosed in the second and third decades of life and the prevalence is higher in males with a 2:1 ratio [1]. It is a, solitary, benign bone neoplasm which accounts for approximately 1% of all bone neoplasms and 3.5% of benign bone neoplasms [2].
It more frequently affects the spine, long bones, metacarpals, metatarsals and facial bones including the jaws. Radiographically it appears as a radiolucent lesion that can be ill or well defined. There are two main clinicopatholocigal entities: Benign form which grows slowly over many years and has a well defined sclerotic margin, is fairly well vascularised with a mild inflammatory response. Another is the aggressive form which exhibits locally aggressive behaviour with a propensity to recur and has typical histopathological features, often making differentiation from low grade osteosarcoma difficult. Foci of patchy, cloud like radiopacities may be seen within the lesion [3].
Jaffe and Mayer in 1932 discovered the lesion and named it as osteoblastic osteoid tissue forming tumour. Other synonyms associated were giant osteogenic fibroma and giant osteoid osteoma. In 1956 it was separately termed as Osteoblastoma by Jaffe and Lichenstein. The name is also adopted by the World Health Organisation Classification of bone tumours and the Armed Forces Institute of Pathology [4].
Aetiologies associated are trauma, inflammation, abnormal local response of tissue injury and local alteration in bone physiology [5].
It appears as a well circumscribed, solitary lesion which measures 2cm or more and may be as large as 12 cm [6]. The teeth maybe tender or mobile if the supporting bone is involved [7].
Al Alvares Capelozza et al., reported a somewhat similar case about an eight-year-old male patient with a growth in the mandibular anterior region since one year. The lesion measured 1cm x 1cm with a missing tooth irt 41. The swelling extended from 41 region to 43 region. Routine radiographic examination examinations revealed mixed radiographic lesion. The lesion was then surgically removed. Histopathology confirmed the diagnosis as Benign Osteoblastoma [8].
In this present case the 27-year-old female patient exhibited a huge intraoral swelling extending from the anterior mandibular region till 46 region, the swelling has been slowly growing in size since last 10 years and is associated with pain since last one year. Computer Tomography with 3D reconstruction showed a lingual extension of the lesion. The significance of this case is in the duration of the lesion, the extension of the lesion with associated pain, displacement of the teeth from the occlusion posed difficulty in mastication and frequent ulceration on the overlying mucosa due to trauma while chewing.
The present case clearly signifies the difficulties faced by the patient in a long standing osteoblastoma. This not only posses problems in the aesthetics of the patient but also seriously interferes in the function.
Conclusion
The clinical appearance of the tumour in this case is very distinct. All routine radiographic examinations were carried out before finally being correlated with histopathology to confirm the diagnosis as osteoblastoma. A careful evaluation of the clinical, radiographic and histopathologic features is essential to determine the treatment protocol, prognosis and follow up of the patient. Complete surgical excision is recommended so as to eliminate the risk of reoccurrence of osteoblastoma.
[1]. Kulkarni MM, Aggressive Osteoblastoma of the mandible: A case reportInt J Contemp Dent 2011 2:135-38. [Google Scholar]
[2]. Bo LIN, Osteoblastoma of the Maxilla and Mandible: A Report of 2 Cases and Literature ReviewChin J Dent Res 2012 15:153-58. [Google Scholar]
[3]. Rawal YB, Gnathic Osteoblastoma: Clinicopathologic Review of seven cases with long term followupOral Oncol 2006 42:123-30. [Google Scholar]
[4]. Manjunatha BS, Osteoblastoma of the jaws: report of a case and review of literatureClin Pract 2011 1:118 [Google Scholar]
[5]. Chen JY, Osteoblastoma (Agressove Form) of the mandible-Report of a caseCases Journal TAOMFR 2012 4:1 [Google Scholar]
[6]. Ivkovic T, Vuèkovic N, Gajanin R, Karalic M, Stojiljkovic B, Panjkovic M, Benign osteoblastoma of the mandibleArch Oncol 2000 8:73-74. [Google Scholar]
[7]. Ozturk M, Osteoblastoma of the Mandible with root resorption: A case reportQuintessence Int 2003 34:135-38. [Google Scholar]
[8]. Alvares Capelozza AL, Osteoblastoma of the mandible: systematic review of litereature and report of a caseDentomaxillofac Radiol 2005 34:1-8. [Google Scholar]