Parathyroid Adenoma Associated with Granulomatous Inflammation: A Curious Cause of Hypercalcaemia
Hena Paul Singh1, Vikram Narang2, Neena Sood3, Harpreet Puri4
1 Senior Resident, Department of Pathology, Dayanand Medical College & Hospital, Ludhiana, India.
2 Assistant Professor, Department of Pathology, Dayanand Medical College & Hospital, Ludhuana, India.
3 Professor & Head, Department of Pathology, Dayanand Medical College & Hospital, Ludhuana, India.
4 Professor, Department of Pathology, Dayanand Medical College & Hospital, Ludhuana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vikram Narang, Assistant Professor, Department of Pathology, DMCH, Ludhiana, Punjab, India.
E-mail: drvikramnarang@yahoo.com
Primary Hyperparathyroidism (PHPT) due to solitary parathyroid adenoma followed by parathyroid hyperplasia and carcinoma are the most frequent cause of hypercalcaemia. The most common granulomatous disorders causing hypercalcaemia are sarcoidosis and tuberculosis. We have reported a case where unexplained granulomas were seen along with parathyroid adenoma.
Hyperparathyroidism, Tuberculosis, Sarcoidosis
Case Report
A 43-year-old female presented with complains of body pains and fatigue of 4 months duration. Her physical examination and routine investigations (complete blood counts, urine routine examination) were normal except for increase Serum Parathyroid hormone (161.4 pg/ml) and increased serum calcium levels (1.55 mmol/L). Ultrasound neck was planned with clinical suspicion of parathyroid adenoma which showed a well-defined space occupying lesion in left lobe of thyroid measuring 23x17mm. Parathyroid scan (20mCi of Tc- 99m sesta MIBI) showed a focal area of increased uptake in relation to lower pole of left lobe of thyroid gland and was suggestive of Left lobe Parathyroid adenoma [Table/Fig-1a]. Chest X ray was normal. No past history or family history of tuberculosis was present. Sarcoidosis was excluded as her ACE levels were also normal.
/b> (a). Parathyroid scan (20mCi of Tc- 99m sesta MIBI) showed a focal area of increased uptake in relation to lower pole of left lobe of thyroid gland and was suggestive of Left lobe Parathyroid adenoma. (b) Granulomas in parathyroid adenoma (arrow) (100X,H&E).
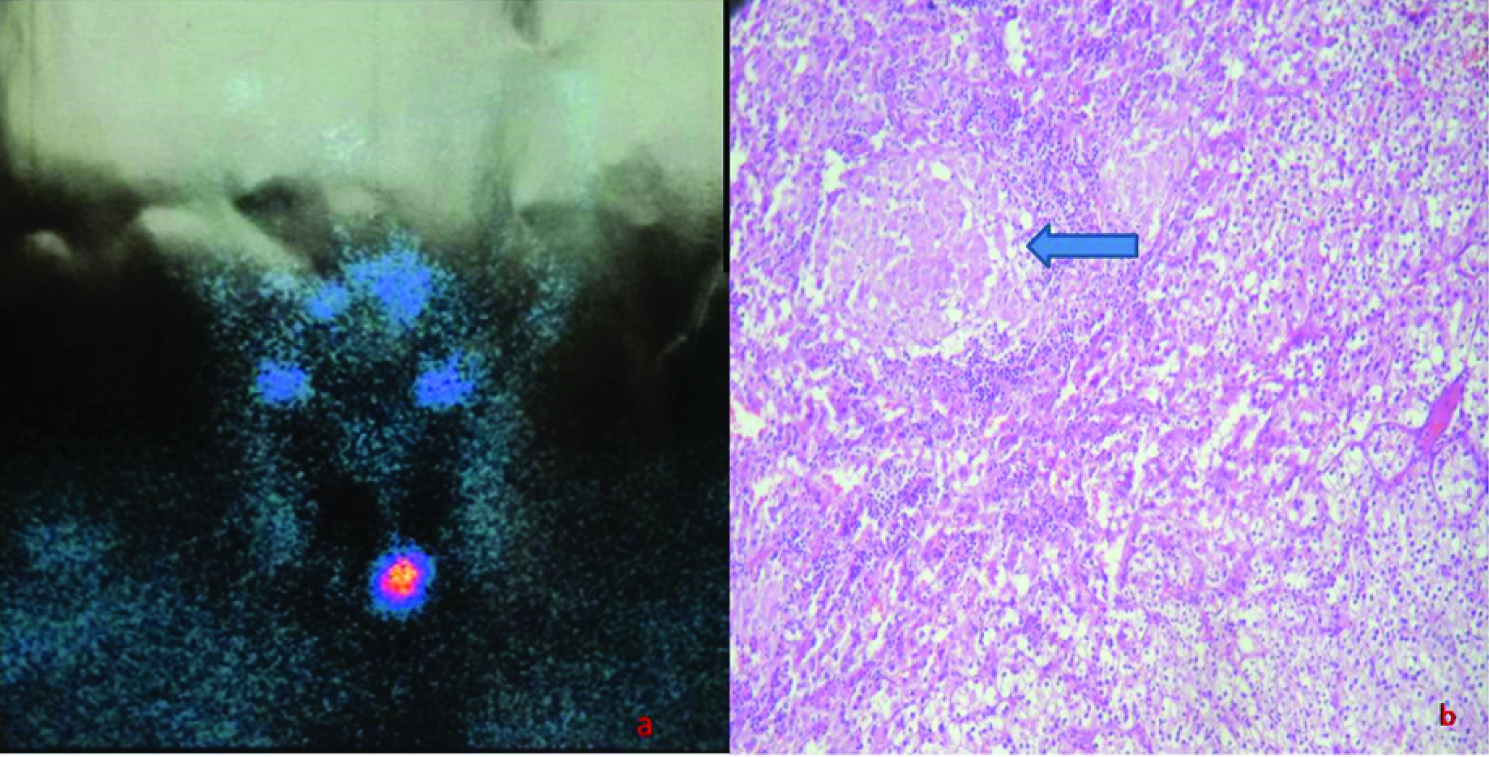
She underwent excision of left parathyroid gland and tissue was subjected to histopathology. Grossly, there was a well encapsulated grey tan soft tissue piece measuring 2.0x2.0x1.0 cm. on cutting lesion had a yellowish brown appearance. Histopathological examination revealed features of parathyroid adenoma along with presence of epitheloid cell granulomas associated with Langhans and foreign body giant cells [Table/Fig-1b]. Zeihl-Neelson stain for Acid fast bacillus was negative.
Discussion
Hypercalcaemia in PHPT is due to activation of osteoclasts, leading to increased bone resorption. It has also been demonstrated to be associated with vitamin D (1,25(OH)2D3) mediated granulomatous disorders, reflecting disordered extrarenal production of 1,25 (OH)2D3 [1–3]. The most common granulomatous disorders causing hypercalcaemia are sarcoidosis and tuberculosis. Other causes include lymphoma, silicone-induced granulomatosis, paraffin-induced granulomatosis, berylliosis, Wegener’s granulomatosis and eosinophilic granuloma. Underlying infectious etiologies may include fungal infections (candidiasis, histoplasmosis, coccidioidomycosis) and leprosy. Although most patients with granulomatous disease-related hypercalcaemia are asymptomatic but symptoms and signs of chronic hypercalcaemia can occur [4–6].
The present case had enough radiological and biochemical evidence of hyperparathyroidism which was the cause of hypercalcaemia in the patient. The fall in calcium and Parathormone levels postoperatively also suggest as parathyroid adenoma being the cause of hypercalcaemia [Table/Fig-2]. This patient had no family history or past history of tuberculosis and the CXR was normal. Also there were no complains of cough or loss of appetite. Thus primary lung tuberculosis was ruled out. This patient had normal ACE levels and as previously discussed normal CXR, so hypercalcaemia due to sarcoidosis was also ruled out. Moreover, her medical history and clinical findings for berylliosis, coccidioidomycosis, and histoplasmosis were all negative.
Comparison of pre and postoperative PTH levels.
| Before operation | After operation | Normal levels |
|---|
| PTH (parathyroid hormone) serum | 161.40pg/ml | 25.30pg/ml | 15.00-65.00pg/ml |
| Serum calcium | 1.55mmol/L | 1.20pg/ml | 1.16-1.32mmol/L |
Anaforoglu et al., and Jacob et al., couldn’t ascertain the reason behind this co-existence of parathyroid adenomas and granulomatous infiltration [1,7]. Jacob et al., preferred to begin anti-tuberculous treatment for their patient. Similarly, we could not ascertain any aetiology of granulomatous inflammation in the index case even with extensive clinical and laboratory work up. The patient was not started on anti-tubercular treatment and was advised to follow-up in the out patient department.
Conclusion
Granulomas within a parathyroid adenoma are a rare. The detailed clinical and pathology workup is necessary to ascertain the exact aetiology, however rarely it might not be possible to find the exact reason of granulomatous response as was in the present case.
[1]. Anaforogl I, Siviloglu C, Livaoglu A, Algun E, Granulomatous infiltration of a parathyroid adenoma presenting as primary hyperparathyroidism in a woman: a case reportJ Med Case Reports 2010 4:400 [Google Scholar]
[2]. Hewison M, Burke F, Evans KN, Lammas DA, Sansom DM, Liu P, Extra- renal 25-hydroxyvitamin D3 - 1±- hydroxylase in human health and diseaseJ of Steroid Biochemistry & molecular biology 2007 103:316-21. [Google Scholar]
[3]. Sadideen HM, Blaker P, Donnell PO, Taylor J, Goldsmith DJ, Tuberculosis complicating tertiary hyperparathyroidism in a patient with end-stage renal disease: a case reportJ Nephrol 2008 21:438-41. [Google Scholar]
[4]. Kar DK, Agarwal G, Mehta B, Agarwal J, Gupta RK, Mishra SK, Tuberculous Granulomatous inflammation associated with adenoma of parathyroid gland manifesting as primary hyperparathyroidismEndocr Pathol 2001 13:355-59. [Google Scholar]
[5]. Taguchi K, Makimoto K, Nagal S, Kitachi M, Izumi T, Yamabe H, Cystic parathyroid adenoma with coexistant sarcoid granulomasArch Otorhinolaryngol 1987 243:392-94. [Google Scholar]
[6]. Robinson RG, Kerwin DM, Tsou E, Parathyriod adenoma with coexistant sarcoid granulomas. A hypercalcaemia patientArch Intern Med 1980 140:1547-48. [Google Scholar]
[7]. Jacob PM, Sukumar GC, Nair A, Thomas S, Parathyroid adenoma with necrotizing granulomatous inflammation presenting as primary hyperparathyroidismEndocr Pathol 2005 16:157-60. [Google Scholar]