A Rare Case of Angiofibroma Arising from Inferior Turbinate in a Female
Gautam Bir Singh1, Shilpi Agarwal2, Rubeena Arora3, Pankaj Doloi4, Deepak Kumar5
1 Professor, Department of ENT & Head-Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
2 Professor, Department of Pathology, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
3 Senior Resident, Department of ENT & Head-Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
4 Senior Resident, Department of ENT & Head-Neck Surgery, Lady Hardinge Medical College & Associated Hospitals, New Delhi, India.
5 Ex-Junior Resident/LHMC, Department of ENT & Head-Neck Surgery, ESI Hospital, Rohini, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gautam Bir Singh, House No:1433/Sector:15, Faridabad-121007 [NCR], Haryana, India.
E-mail: gbsnit@yahoo.co.in
A rare case of extranasopharyngeal angiofibroma arising from the inferior turbinate in a young female of 28 years is presented. The case is discussed in light of scant contemporary literature on the cited subject. This clinical record highlights the distinct clinical nature of Extranasopharyngeal angiofibroma (ENA) and importance of Immunohistochemistry in diagnosis of such lesions. With this case we report a rare clinical entity which presented in an extremely rare manner.
Extranasopharyngeal angiofibroma, Females
Case Report
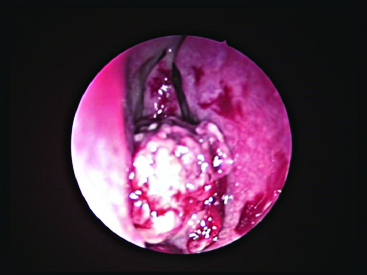
A 28-year-old female reported to the ENT outpatient department of our institution with the chief complaints of epistaxis and nasal obstruction in the right nasal cavity for the past 3 years and 6 months respectively. The frequency of episodes of epistaxis, though in form of mild spotting had increased to 6 episodes in the last one year. On examination a pinkish lesion was seen in the right nasal cavity [Table/Fig-1]. On probe test: the lesion was seen arising from the right inferior turbinate and was non tender but bled on touch. Clinically Nasal Polyp (including fungal), Papilloma, Haemangioma and Malignancy were kept as differentials for the said lesion. A Contrast Enhancement Computed Tomography Scan of the nose and paranasal sinuses was done which showed a 2.5 X 2.1 X 2.6 cm size enhancing lesion in the right nasal cavity, arising from the inferior turbinate with no bony erosion [Table/Fig-2]. As the lesion was small in size and at an accessible location, complete endoscopic excision was done. Mild postoperative bleeding was observed which was controlled by electrocautery. It would also be important to note that as our patient’s background features were not compatible with angiofibroma, she was not referred for angiography or embolization prior to surgery.
Ulceroproliferative lesion originating from right inferior turbinate.
A CECT scan showing an enhancing lesion in the right nasal cavity, arising from the inferior turbinate with no bony erosion.

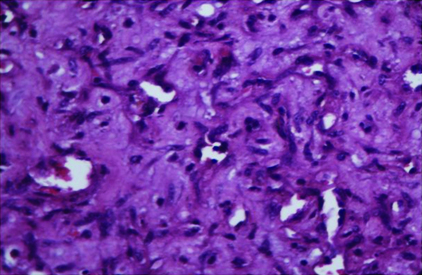
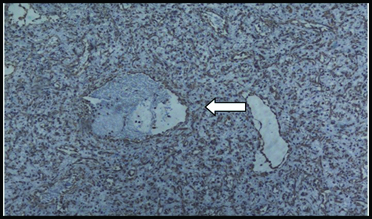
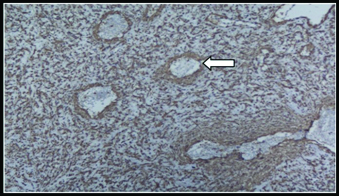
Histopatholgy revealed: Thin walled blood vessels surrounded by fibrous stroma. The blood vessels were lined by a single layer of endothelial cells and incomplete muscular walls [Table/Fig-3]. The following histopathological differential diagnoses were made: Capillary haemangioma, Haemangiopericytoma, Solitary fibrous tumour and Angiofibroma. To confirm the diagnosis immunohistochemistry was done. Immunohistochemistry (IHC) showed vimentin positive stromal cells, SMA positive in cells around vascular spaces and CD34 positivity in vascular endothelial cells [Table/Fig-4,5 and 6] consistent with angiofibroma. Thus a final diagnosis of Extranasopharyngeal Angiofibroma (ENA) of the inferior turbinate was made. The case is in regular follow-up with us for the past one year with no recurrence or any untoward incident to report.
400X. H&E: Variable sized vascular spaces in fibrous stroma.
100X. Vimentin positive in stromal cells (arrow).
100X. CD34 positive in vascular endothelial cells (variable sized vascular spaces) with interspersed stromal cells (arrow).
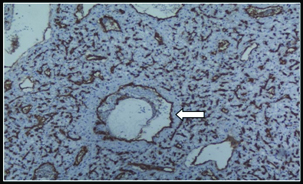
100X-SMA: Circumferential incomplete staining around vascular spaces (arrow).
Discussion
Angiofibromas are rare vascular tumours which originate predominantly in the nasopharynx and occur typically in male adolescents [1,2]. ENA is a distinct clinical entity, different from nasopharyngeal angiofibroma (NA). Further, ENA in extranasopharyngeal sites such as nasal cavity and paranasal sinuses have been sporadically reported in the literature [1–3]. Some salient distinguishing features of ENA are: it is seen in adults (mean age: 22-28 years), whereas angiofibroma is seen in an adolescent male (mean age:15 years) [1,2]. Moreover, it has been frequently reported in females (25% cases) unlike NA [1,2,4,5]. Not much is known about its aetiology, however developmental, genetic and hormonal theories have been proposed [3,4,6,7]. It usually presents with bleeding but it is not as profuse as NA. A Computed Tomography Scan is sufficient to make a diagnosis as it clearly delineates the tumour [5,8]. Magnetic Resonance Imaging & arteriography are also valuable diagnostic investigations; however the exclusion of hypervascularity with arteriography does not exclude extranasopharyngeal angiofibroma [4]. Surgical excision is the primary modality of treatment for these lesions [1–4]. It would also be important to note that recurrence though common for NA has never been reported for ENA [1,2,8].
Histopathologically: The commonest site of origin of ENA is maxillary sinus and they have less vascular component and more fibrosis as compared to NA [1,2,5]. It would be prudent to note that in accordance with “Evidence Based Medicine” immunohistochemistry (IHC) clinches the diagnosis [3]. Though a haemangioma can be distinguished from ENA by marked lobulation and decreased stromal fibrosis, it is difficult to differentiate it from hemangiopericytoma. An immunohistochemical analysis of this lesion shows positive staining for vimentin and negative staining for CD34 and smooth muscle alpha actin [7]. Angiofibromas have positive staining for vimentin, CD34 and alpha-actin [3]. Moreover, a significantly high CD34 expression in angiofibroma distinguishes it from cavernous haemangioma also.
In context of this case it would be prudent to note Extranasapharyngeal angiofibroma arising from the inferior turbinate is a rarity. In a massive internet search using pubmed/medline services we could find only 14 cases arising from the inferior turbinate [3–5] Out of these only four have been reported in females. To the best of our knowledge this is the second case of ENA arising from the inferior turbinate in a young female in reproductive age group (previous two such cases of have been reported in menopausal females) [3,4]. Interestingly, IHC evidence has not been given for the earlier reported case in the young female [4]. In addition, such cases lead us to refute the hormonal theory of angiofibroma that suggests: it is a testosterone-dependent tumour seen mostly in adolescent males and high estrogen levels protect females against this tumour [8]. Further, the primary localization of ENA in inferior turbinate is difficult to explain on the basis of “fascia Basalis” theory by Brunner [9], as it is absent in inferior turbinate. We thus believe that these tumours may be a developmental anomaly: vascular tissue is retained as an ectopic nidus in developing periosteum of inferior turbinate [8,10].
Conclusion
In summary, this exceptional atypical cause of epistaxis (inferior turbinate ENA) in a young female merits mention on account of:
Rarity of the lesion and its underreporting in the medical literature
Immunohistochemistry validation of inferior turbinate ENA in a young female hitherto unreported in the medical literature
Highlighting the ambiguity in the aetiopathogenesis of angiofibroma.
[1]. Szymanska A, Scymanska M, Morshed K, Czekajska-Chehab E, Szczerbo-Trojanowska M, Extranasopharyngeal angiofibroma: clinical and radiological presentationEur arch Otolaryngol 2013 270:655-60. [Google Scholar]
[2]. Windfuhr JP, Remmert S, Extranasopharyngeal angiofibroma: etiology, incidence and managementActa Otolaryngol 2004 124:880-89. [Google Scholar]
[3]. Peric A, Sotirovic J, Cerovic S, Zivic L, Immunohistochemistry in diagnosis of extranasopharyngeal angiofibroma originating from nasal cavity: case presentation and review of literatureActa medica 2013 56(4):133-41. [Google Scholar]
[4]. Salimov A, Ozer S, A Rare Location of Angiofibroma in the InferiorTurbinate in Young WomanInt Arch of otorhinolaryngol 2015 19:187-90. [Google Scholar]
[5]. Nomura K, Shimomura A, Awatuguchi T, Marakami K, Kobayashi T, A case of angiofibroma originating from nasal turbinateAuris Nasus Larynx 2006 33:191-93. [Google Scholar]
[6]. Alvi A, Myssiorek D, Fuchs A, Extranasopharyngeal angiofibromaJ Otolaryngol 1996 25:346-48. [Google Scholar]
[7]. Yokoi H, Arakawa A, Kuribayashi Inoshita A, Haruyama T, Ikeda K, An immunohistochemical study of sinonasal hemangiopericytomaAuris nasus Larynx 2011 38:743-46. [Google Scholar]
[8]. Akbas Y, Anadolu Y, Extranasopharyngeal angiofibroma of the head and neck in womenAm J of otolaryngol 2003 24:413-16. [Google Scholar]
[9]. Brunner H, Nasopharyngeal fibromaAnn Otol 1942 51:30-65. [Google Scholar]
[10]. Schiff M, Pathology of juvenile nasopharyngeal angiofibroma-a lesion of adolescent malesCancer 1959 7:15-28. [Google Scholar]