Scrub Typhus Presenting with Bilateral Lateral Rectus Palsy in A Female
Tony Ete1, Jaya Mishra2, Bhupen Barman3, Sumantro Mondal4, Rondeep Kumar Nath Sivam5
1 Senior Resident, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
2 Associate Professor, Department of Pathology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
3 Assistant Professor, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
4 Post Doctoral Trainee, Department of Rheumatology, Institute of Post Graduate Medical Education and Research, Kolkata, West Bengal, India.
5 Senior Resident, Department of Cardiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tony Ete, Senior Resident, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India. E-mail : tonyete14@gmail.com
Scrub typhus, a rickettsial disease is endemic in several parts of India usually presenting with acute symptoms. Fever, maculopapular rash, eschar, history of tick exposure and supportive diagnostic tests usually leads to diagnosis. Scrub typhus should be included in the differential diagnosis in occasions when a patient presents with fever with or without eschar and isolated cranial nerve palsy. Here we are reporting a case of Scrub typhus who presented with fever and altered sensorium of short duration, eschar formation and bilateral lateral rectus palsy. Patient was treated with doxycycline with complete reversal of neurodeficit.
Eschar, Orientia tsutsugamushi, Rickettsial disease
Case Report
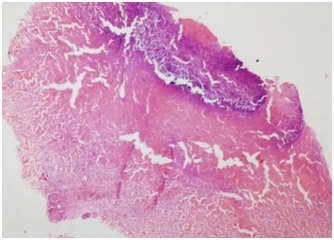
A 22-year-old female, living in a village in northeast India presented with, high grade, continuous fever for five days, associated with headache and myalgia. Fever was followed by irrelevant talks and alteration in sensorium. There was no history of seizure or vomiting. She also developed yellowish discolouration of sclera. There was no past or contact history of tuberculosis. On examination, patient was febrile and had altered sensorium. Pulse rate was 100/minute, regular, BP-110/70 mm Hg, respiratory rate-24/minute. The patient had a dark, hyperpigmented, raised, patch in left infra-axillary region suggestive of an eschar [Table/Fig-1]. Respiratory system, cardiovascular system and per abdominal examination were non contributory. On neurological examination, higher mental function was impaired in the form of disorientation and clouding of consciousness. Plantar reflex was flexor bilaterally. Cranial nerve examination revealed bilateral lateral rectus palsy [Table/Fig-2]. Investigations showed Hb-9.3 gm%, total leucocyte count-6000/cumm, platelets-1.9 lacs/cumm, PCV-28%, ESR-70mm/h. Peripheral blood smear showed normocytic normochromic anaemia with relative lymphocytosis. Malaria parasite slide and dual antigen were negative. Liver function test revealed total bilirubin-3.2mg/dl, direct bilirubin-1.5 mg/dl, SGOT-169 U/l, SGPT-91 U/l, albumin-2.4 gm/dl, globulin-4.9 gm/dl. Blood for HbsAg, anti HCV, HIV-1 and HIV-2 antibody were negative. Dengue NS-1 antigen and IgM, IgG anti-dengue antibody by ELISA were also negative. Urea-22 mg/dl, creatinine-0.5 mg/dl. Widal test was negative. Chest X-ray was normal. Sonography of abdomen revealed mild hepatosplenomegaly with minimal right sided pleural effusion. Cerebrospinal fluid study showed cell count-3/cumm predominantly lymphocytes, glucose 54mg/dl, protein-117 mg/dl, Adenosine Deaminase (ADA) below 10 U/l. MRI of brain with contrast was normal. Considering patient’s area of living, clinical presentation of fever and skin lesion, blood test to confirm scrub typhus (IgM) was sent which came out to be positive on immunofluorescence assay. Skin biopsy showed extensive dermal necrosis with small vessels of the upper and lower dermis showing necrotizing vasculitis with perivascular lymphocytic and neutrophilic infiltrate. There was extravasation of red blood cells and evidence of luminal thrombosis and also there were zones of infarction [Table/Fig-3]. Features were in favour of typical eschar (Doxycycline to be considered after confirmation of diagnosis). She responded on third day with improvement in sensorium however she developed diplopia and her lateral rectus palsy persisted. The patient was given a full course of doxycycline along with azithromycin with occular movement exercises and discharged with an advice to follow up in outpatient department.
Eschar (Left infra axillary region).

showing right lateral rectus palsy and left lateral rectus palsy.

HPE of skin biopsy from the eschar showing extensive dermal necrosis with small vessels of the upper and lower dermis showing necrotizing vasculitis with perivascular lymphocytic and neutrophilic infiltrate.
Discussion
Scrub typhus is a tropical febrile illness with multisystem involvement caused by Orientia tsutsugamushi which is transmitted to humans by an arthropod vector of the Trombiculidae family. The organism is an obligate intracellular gram negative organism. It is prevalent in some parts of India including North eastern region [1].
It is usually characterized by fever, myalgia, headache, rash, eschar formation and meningoencephalitis. Incubation period in human hosts range from 5 to 20 days. Neurological involvement in the form of meningoencephalitis has been described quite often. However, focal neurological deficit in the form of isolated cranial nerve palsy is very uncommon. Historically, scrub typhus occurred among allied military personnel causing mortality and resulting in burden in Second World War [2]. The disease usually begins with the inoculation of the organism following the bite of the mite. Multiplication of this organism at the site of bite results in the formation of an eschar which is considered as the pathognomonic clinical finding. The painless chigger bite can occur on any part of the body. It usually begins as a small papule which enlarges, undergoes central necrosis and acquires a blackened crust to form an eschar [3]. A classic triad of fever, rash and history of tick exposure is often present. In India, around 50 % cases of scrub typhus report tick exposure. The weil felix test has been considered as diagnostic tool when used and interpreted in the correct clinical context [4]. The gold standard for diagnosis is immunofluorescence assays [5]. The common organ system complications seen in scrub typhus are hepatitis, acalculous cholecystitis, pancreatitis, acute renal failure, acute respiratory distress syndrome, hilar lymphadenopathy, pleural effusion, meningoencephalitis, seizures, vasculitic cerebral infarct, cardiac rhythm abnormalities, myocarditis [6]. The main pathologic change in scrub typhus is focal or disseminated vasculitis caused by the destruction of endothelial cells and perivascular infiltration of leucocytes [7]. Generalised vasculitis leads to fatal complications like pneumonia, shock, meningitis, encephalitis in severe cases. Neurological involvement in scrub typhus is attributed to inflammation and vascular leakage of intracranial blood vessels. CSF examination is usually consistent with aseptic meningitis. Neurological involvement in scrub typhus may present in the form encephalomyelitis with prominent focal neurologic signs [8]. Cranial nerve involvement in scrub typhus is very uncommon. Cranial nerve involvement in the form of bilateral facial nerve palsy has been reported [9]. Scrub typhus with involvement of eighth cranial nerve with sensorineural hearing loss has also been described [10]. Rickettsial fever with isolated third nerve palsy has been reported [11]. Involvement of abducens nerve in scrub typhus is very uncommon [12]. Neuro imaging studies are often normal in these settings. The isolated cranial nerve palsies are attributed to the micro infarction due to vascular involvement of vasa narvorum and also stretching of the vessels due to dilated ventricles. Here we are reporting a case of scrub typhus presented with eschar with bilateral abducens nerve palsy with normal imaging features that was initially treated with doxycycline and later on with azithromycin. Patient responded well to treatment and her clinical condition improved without any permanent sequelae.
Conclusion
Rickettsial fevers are endemic in some states of India and its diagnosis also requires a high index of suspicion as its initial clinical features resembles many diseases. However, focal neurologic signs with classic clinical features like fever, maculopapular rash in an endemic area should alert the physician to consider scrub typhus as one of the possible differentials.
[1]. Mahajan SK, Kashyap R, Kanga A, Sharma V, Prasher BS, Pal LS, Relevance of Weil-Felix test in diagnosis of scrub typhus in IndiaJ Assoc Physicians India 2006 54:619-21. [Google Scholar]
[2]. Elsom KA, Beebe GW, Sayen JJ, Scheie HG, Gammon GD, Wood FC, Scrub typhus: a follow-up studyAnn Intern Med 1961 55:785-95. [Google Scholar]
[3]. Watt G, Parola P, Scrub typhus and tropical rickettsiosesCurr Opin Infect Dis 2003 16(5):429-36.Review [Google Scholar]
[4]. Kularatne SA, Gawarammana IB, Validity of the Weil-Felix test in the diagnosis of acute rickettsial infections in Sri LankaTrans R Soc Trop Med Hyg 2009 103(4):423-24. [Google Scholar]
[5]. Parola P, Fenollar F, Badiaga S, Brouqui P, Raoult D, First documentation of Rickettsia conorii infection (strain Indian tick typhus) in a TravelerEmerg Infect Dis 2001 7(5):909-10. [Google Scholar]
[6]. Bhardwaj B, Panda P, Revannasiddaiah S, Bhardwaj H, Abducens nerve palsy in a patient with scrub typhus: a case reportTrop Biomed 2013 30(4):706-09. [Google Scholar]
[7]. Pai H, Sohn S, Seong Y, Kee S, Chang WH, Choe KW, Central nervous system involvement in patients with scrub typhusClin Infect Dis 1997 24(3):436-40. [Google Scholar]
[8]. Kim DE, Lee SH, Park KI, Chang KH, Roh JK, Scrub typhus encephalomyelitis with prominent focal neurologic signsArch Neurol 2000 57(12):1770-72. [Google Scholar]
[9]. Lin WR, Chen TC, Lin CY, Lu PL, Chen YH, Bilateral simultaneous facial palsy following scrub typhus meningitis: a case report and literature reviewKaohsiung J Med Sci 2011 27(12):573-76. [Google Scholar]
[10]. Kang JI, Kim DM, Lee J, Acute sensorineural hearing loss and severe otalgia due to scrub typhusBMC Infect Dis 2009 9:173 [Google Scholar]
[11]. Rajadhyaksha A, Phatak S, Nolkha N, Pathan Y, Sonawale A, Rickettsial fever presenting with isolated third nerve palsyJ Assoc Physicians India 2013 61(2):144-45. [Google Scholar]
[12]. Lee YH, Yun YJ, Jeong SH, Isolated abducens nerve palsy in a patient with scrub typhusJ AAPOS 2010 14(5):460-61. [Google Scholar]