Combined Arterial and Venous Thrombosis in Ulcerative Colitis- A Rare Vascular Manifestation
Harpreet Singh1, Pranav Ish2, Richa Dewan3, S Anuradha4, Sumeet Singla5
1 Senior Resident, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
2 Post Graduate Resident, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
3 Director Professor, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
4 Professor, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
5 Assistant Professor, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pranav Ish, B1, 1st Floor, Green Park Extension, New Delhi -110016, India.
E-mail: pranavish2512@gmail.com
Combined arterial and venous thrombosis in patients with ulcerative colitis is a rare extra vascular manifestation, which motivated the current report. Increased coagulability is a recognised feature of ulcerative colitis with frequency increasing during flares. We report the case of a 42-year-old lady who was a diagnosed case of ulcerative colitis, currently in remission. She presented with swelling followed by discolouration of left lower limb which later was diagnosed as deep venous thrombosis combined with femoral and popliteal artery thrombosis. This led to wet gangrene of the limb, sepsis, septic shock and death despite aggressive management with heparin infusion, ionotropes, and parenteral antibiotics therapy.
Remission, Thromboembolic complications, Wet gangrene
Case Report
A 42-year-old lady, resident of Delhi presented to medicine emergency with complaints of Swelling in left lower limb for 2 days. She was a follow up case of ulcerative colitis, initially on mesalamine, now in remission not on any medication. There was no history of fever, diarrhea or blood in stools, decreased urine output, breathlessness, chest pain, prolonged immobilization, air travel, oral contraceptive pill intake, trauma, stroke or recurrent miscarriages. On examination, patient was conscious and oriented to time, place and person. Patient had pulse rate – 98/minute in all 4 limbs, Blood Pressure – 92/60 mm of Hg in right brachial artery. Left leg was swollen and tender below the calf and the distal pulses were feeble.
Central Nervous System examination revealed that the patient was conscious, oriented in time, place and person. There was no sensory or motor deficit. All reflexes within normal limit. Bilateral plantar reflex were normal. Cardiovascular, per abdomen and respiratory system were grossly normal. The blood investigations of the patient are shown in [Table/Fig-1].
| Investigation | Day 1 | Day 2 |
|---|
| Haemoglobin | 10.8 grams% | 10.6 |
| Total leucocyte count | 30000cells/mm3 | 42600 |
| Platelet count | 1.8/mm3 | 2.0 |
| Serum Urea/creatinine | 63/2.2 mg/dl | 62/2.1 |
| Serum sodium/potassium | 142/3.9 meq/l | 144/4.1 |
| T.bilirubin/Direct.bilirubin | 1.9/1.3 mg/dl | |
| AST/ALT | 35/36 IU | |
| ALP | 162 IU | |
| Total protein/S erum albumin | 10/4.5 grams/dl | |
| Calcium/phosphate | 9/4.2 mg % | |
| Prothrombin Time | 13/13 | |
| APTT(INR) | 1.0 | 1.8 |
AST-Aspartate Transaminase, ALT-Alanine Transaminase, ALP-Alkaline Phosphatase, APTT-Activated Partial Thromboplastin Time, INR- International Normalized Ratio
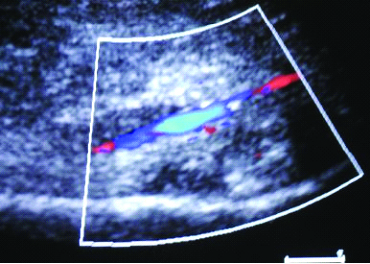
USG doppler in emergency was suggestive of left lower limb Deep Venous Thrombosis (DVT) involving the common femoral and superficial femoral veins on left side. No changes suggestive of pulmonary embolism were present on ECG. A provisional diagnosis of Ulcerative colitis (in remission) with left lower limb DVT with sepsis with hypotension with acute kidney injury was made and patient was started on intravenous ceftriaxone 1 gram 12 hourly, injection noradrenalin infusion 0.8 mg/hr and subcutaneous enoxaparin 60 IU 12 hourly. However, the next day morning (within 12 hours of presentation) the patient developed severe pain in left lower limb with mild blackish discolouration of the distal limb. [Table/Fig-2] Urgent USG arterial doppler was done and it was suggestive of no flow in anterior tibial and popliteal artery. There was a heterogenous hypoechoic content in femoral vein with no colour flow and compressibility suggestive of acute deep Vein Thrombosis [Table/Fig-3] with cellulitis.
Clinical photograph of the patient showing edema and discolouration of the left lower limb.

Colour doppler sonography showing echogenic content in the left femoral vein.
Patient was planned for a CT angiography the same day which was suggestive of eccentric filling defect in infra renal part of aorta just above the common iliac arteries bifurcation. [Table/Fig-4]. An urgent cardiology and Cardio Thoracic Vascular Surgery department referral was taken. However in view of sepsis and hypotension, patient was advised conservative management with heparin, inotropes and antibiotics and wait for line of demarcation, Surgical referral for amputation was sought once the CTVS declared the limb unsalvageable. Patient was started on injection heparin infusion at the rate of 800 units/hour. The blackish discolouration of the left lower limb spread to the thigh. Patient was given injection vancomycin 1 gram 12 hourly and injection dopamine infusion starting at 2 microgram/kg/min was added, however, the patient succumbed to her illness on 3rd day of her hospital stay. Informed consent was taken from the husband of the consent for reporting this as a case report on the request of anonymity.
CT angiography- suggestive of eccentric filling defect in lateral wall of infra renal descending aorta with minimal extension into left common iliac vein.

Discussion
Thromboembolic complications are 3 times more likely in patients with Inflammatory Bowel Disease (IBD) than controls and the relative risk exceeds 15 times during flares [1]. The exact pathogenesis being still unknown, IBD have been implicated in occurrence and pathogenesis of increased both arterial and venous thrombosis [2]. Recent literature has even shown cerebral vasculitis to be associated with IBD [3]. Peripheral arterial and venous thrombosis is known, but the occurrence of both together, especially in patients who are in remission of IBD, is uncommon. Ultrasonography with Doppler can help in screening patients with such complications. However, CT-angiography remains the investigation of choice to confirm the diagnosis as it is a rapid and easily available test.
Once diagnosed, treatment of such patients also remains a matter of concern as there is very high morbidity and mortality associated if timely therapy is not started. Even though not indicated prophylactically, heparin use is justified in proven IBD with thrombosis. Duration of such anticoagulation is also not defined as the pathogenesis is not well established.
A European cohort study estimated that the 5-year risk of recurrence was 33% after discontinuing anticoagulant therapy. Also, IBD was associated with a 2.5-fold higher risk of recurrence with a first unprovoked VTE. This data suggest that IBD is a continuing risk factor for recurrent VTE and, therefore, support indefinite anticoagulant therapy in patients with IBD who have VTE [4]. However, the risk-benefit ratio needs to be assessed. Canadian society of gastroenterology has recently recommended use of anticoagulation for prophylaxis of thrombosis in hospitalized patients for flare or surgery and for proven thrombotic events [5]. However, randomized control trials are needed to increase the strength of this recommendation.
Inflammatory activity, repeated hospitalization, surgery, pregnancy, disease type (e.g., fistulising disease, extensive colonic involvement) and treatment (mainly steroids) along with initiation of the coagulation system, down regulation of natural anticoagulant mechanisms, impairment of fibrinolysis, increased platelet count and reactivity and dysfunction of the endothelium have been implicated in the occurrence of thrombotic events in such patients [6]. Recent literature mentions few isolated case reports of thrombosis in stable patients of IBD in remission. A case of venous thrombosis in a child in remission was recently reported [7]. Clinicians must be aware of such potential consequences and should take adequate prophylactic measures in patients who are hospitalised, are submitted to surgery or are undergoing treatment.
Conclusion
There are isolated case reports of combined arterial and venous thrombosis in ulcerative colitis in remission. There is a need for larger case series to formulate guidelines for role of prophylactic anticoagulation in IBD.
Also, a high index of suspicion should be kept in mind when treating ulcerative colitis for such complications as timely diagnosis and prompt treatment determines both morbidity and mortality of the patients.
AST-Aspartate Transaminase, ALT-Alanine Transaminase, ALP-Alkaline Phosphatase, APTT-Activated Partial Thromboplastin Time, INR- International Normalized Ratio
[1]. Ashrafi MR, Hosseini F, Alizadeh H, Sani MN, Pseudotumor Cerebri in a Case of Ulcerative Colitis with Sagittal Sinus ThrombosisIran J Pediatr 2013 23(1):109-12. [Google Scholar]
[2]. Zezos P, Kouklakis G, Saibil F, Inflammatory bowel disease and thromboembolismWorld J Gastroenterol 2014 20(38):13863-78. [Google Scholar]
[3]. Raj N, Arkebauer M, Waters B, Dickinson B, A Case of Cerebral Vasculitis Associated with Ulcerative ColitisCase Rep Rheumatol 2015 2015:598273 [Google Scholar]
[4]. Jain S, Bhatt P, Muralikrishna GK, Malhotra P, Kumari S, Varma S, Extensive arterial and venous thrombosis in a patient with ulcerative colitis- A Case ReportMed Gen Med 2005 7(2):10 [Google Scholar]
[5]. Bernstein CN, Bitton A, Chan AK, Griffiths AM, Leontiadis GI, Consensus Statements on the Risk, Prevention, and Treatment of Venous Thromboembolism in Inflammatory Bowel Disease: Canadian Association of GastroenterologyGastroenterology 2014 146:835-48. [Google Scholar]
[6]. Magro F, Soares JB, Fernandes D, Venous thrombosis and prothrombotic factors in inflammatory bowel diseaseWorld J Gastroenterol 2014 20(17):4857-72. [Google Scholar]
[7]. Gysemans W, Van Geet C, Janssens E, Alliet P, Venous thrombosis in a child with ulcerative colitis in remission: a case reportActa Gastroenterol Belg 2014 77(1):71-74. [Google Scholar]