Complex musculoskeletal wound due to high energy poses a challenge to the treating surgeons regarding wound healing, coverage and reconstruction. These open musculoskeletal injuries produce significant soft tissue defects resulting in delayed wound healing. Despite the advances in treatment to expedite wound healing by several types of treatment regimen including different types of dressings, hyperbaric oxygen therapy, several types of antiseptic agents, skin grafts or local flaps, treatment to these soft tissue injuries present dilemma to the surgeon [1]. The concept of using negative pressure to create a suction force, enabling the drainage of surgical wounds in order to promote wound healing, is well documented in the literature [2–9]. The application of negative pressure removes excess fluid thus promote better capillary circulation and hyperaemia, decreases bacterial load and risk of bacterial colonization and had mechanical effect in drawing wound edges closer.
The study was conducted with the aim to evaluate the effectiveness of vacuum assisted closure therapy for soft tissue injury in open musculoskeletal trauma.
Materials and Methods
This study was conducted on 20 patients presented with soft tissue injury in open musculoskeletal trauma between March 2013 to May 2014. The present study was conducted after obtaining the permission from ethical committee of the institute. The patient included in the study was those who had compound fracture of long bones with soft tissue loss or defect. All patients with open wound that require coverage were included in the study. However, patients with comorbid conditions like diabetes, peripheral vascular disease or chronic osteomyelitis were excluded in this study.
Routine haematological investigation including complete blood count, ESR, blood sugar, HIV, HBsAg was done. Routine radiological investigations were done for the underlying fracture. Aggressive local debridement was done before applying VAC therapy. All necrotic tissues were removed and haemostasis was achieved prior to application of the VAC.
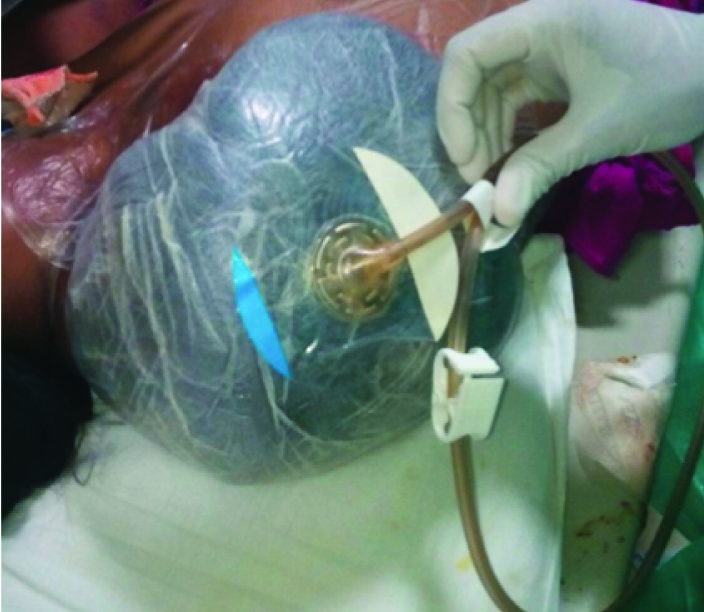
Sterile open – pore foams containing polyurethane ether foam generally of 400-600μm was used as a dressing. An adhesive drape was then applied over the wound area with an additional 2-4cm border of healthy skin to provide an intact seal. Special care was taken to ensure wound was covered in all directions with an air tight seal. Then a hole was created in the film and a self-adhesive evacuation tube was attached over the hole. VAC machine delivers a controlled uniformly placed intermittent negative pressure of -125 mm Hg (7 minute cycle with 5 minute on, 2 minute off). Dressings were changed after every 4 to 5 days. At every dressing the presence of infection, presence or absence of granulation tissue, erythema, and amount of drainage were noted. Routine bacterial cultures and sensitivity testing were done at every dressing. Antimicrobial protocols were followed depending upon the culture and sensitivity report. The vacuum device was used until granulation tissue formed with little or no oedema or drainage, after that secondary procedure like skin grafting and secondary procedure were done [Table/Fig-1,2,3,4,5 and 6].
Wound size of of 94.6 cm2 over the right shoulder.

VAC applied over the wound.
Wound showing healthy granulation tissue with reduced wound size to 80.0 cm2 during dressing.

Large wound size of 92.4 cm2 over anterolateral aspect of distal thigh, knee and leg.

Vac applied over the wound.

Final picture of wound after split skin grafting.

Results
There were 14 males and 6 female patients included in the study. The average patient age was 36.15 years (range 18 to 62 years) [Table/Fig-7]. The average length of follow up was 12 months. Majority of patients with open injury presents due to road traffic accident (70%), followed by patient who had fall from height (30%). Out of 20 patients presented with open injury, 8 patient (40%) had Gustilo Anderson grade 3a, 10 patients (50%) had grade 3b, and 2 patient (10%) had grade 2 injury. Three wounds were infected at the start of VAC therapy. However, all patients were cleared of bacterial infection by the end of VAC therapy.
The frequency of VAC dressing change was done every 4-5 days. Intermittent negative pressure was applied in all patients except in 1 patient. In 1 patient continuous negative pressure was applied. There was no need of repeat surgical debridement in 18 patients during the course of VAC therapy. However in 2 patients, repeat surgical debridement was done due to presence of infection. VAC therapy over the wound was administered for an average of 20.4 days ±6.72 days (range 14 to 42 days) [Table/Fig-7,8].
Characteristics of therapy.
| Characteristics | Findings |
|---|
| Age (yrs) | 36.15±13.27 |
| Sex (M:F) | 14:6 |
| Duration of thearpy (Days) | 20.4±6.72 |
| No of pack of dressing | 4.35±1.424 |
Showing total number of dressing and duration during VAC therapy.
| S.No. | Age(in years) | Gender | Length ofTreatment(in days) | Numberof VACdressingused | Final Outcome |
|---|
| 1 | 25 | M | 18 | 4 | Split skin graft |
| 2 | 35 | M | 20 | 5 | Split skin graft |
| 3 | 28 | F | 22 | 4 | Secondary closure |
| 4 | 42 | F | 14 | 3 | Split skin graft |
| 5 | 22 | M | 32 | 7 | Split skin graft |
| 6 | 26 | M | 16 | 3 | Split skin graft |
| 7 | 18 | F | 18 | 4 | Split skin graft |
| 8 | 44 | M | 25 | 5 | Split skin graft |
| 9 | 29 | M | 14 | 3 | Secondary closure |
| 10 | 54 | M | 16 | 4 | Split skin graft |
| 11 | 48 | F | 42 | 9 | Split skin graft |
| 12 | 23 | M | 18 | 4 | Split skin graft |
| 13 | 30 | F | 16 | 3 | Split skin graft |
| 14 | 46 | M | 17 | 4 | Secondary closure |
| 15 | 48 | M | 26 | 5 | Split skin graft |
| 16 | 24 | F | 22 | 4 | Split skin graft |
| 17 | 23 | M | 18 | 4 | Split skin graft |
| 18 | 38 | M | 20 | 4 | Split skin graft |
| 19 | 62 | M | 16 | 4 | Wound debridement and then split skin graft |
| 20 | 58 | M | 18 | 4 | Wound debridement and then split skin graft |
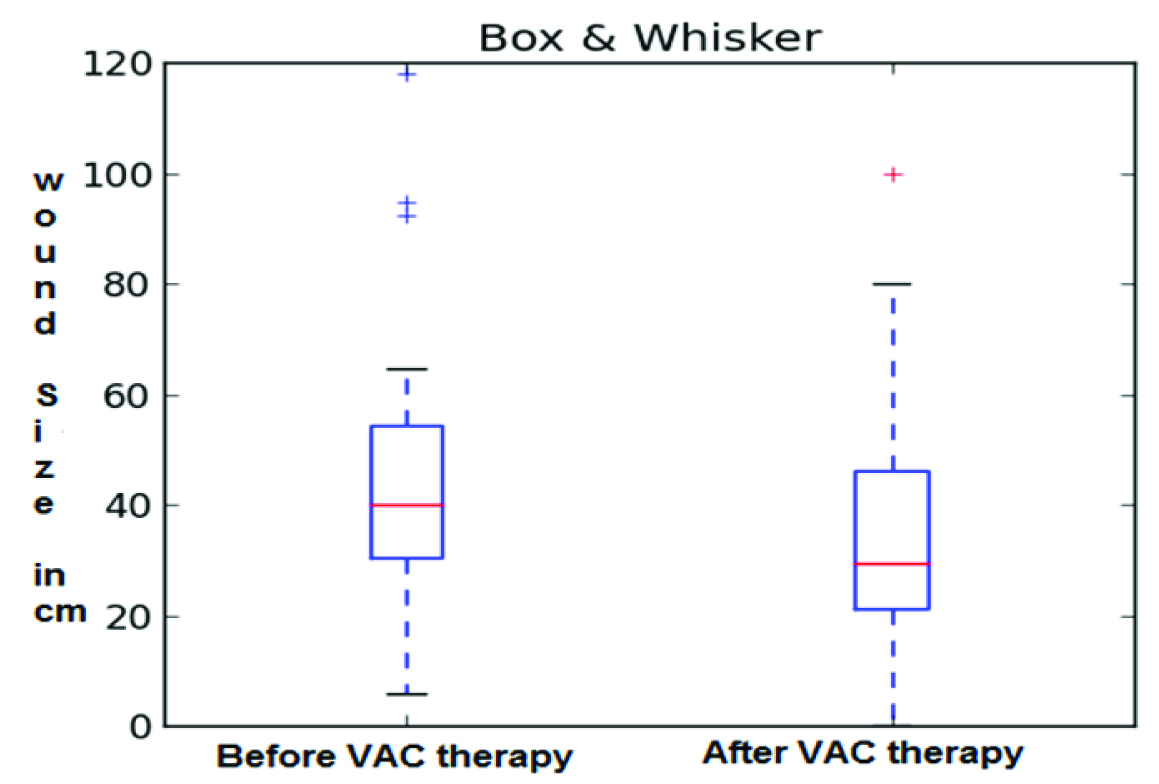
The patient wound area at the time of initial presentation ranged from 5.8 to 118.0 cm2, the average area being 46.8cm2. After VAC therapy, the wound area ranged from 3.2 to 100.0cm2, the average area being 38.0cm2. There was decrease in wound size attained by VAC therapy ranged from 2.6 to 24.4cm2, with an average reduction of 10.55cm2. In 18 patients, wound size was decreased in area and later split skin grafting was done. In patient in whom, repeat debridement done after VAC therapy, there was increase in wound area, but later on split skin grafting was done in both cases [Table/Fig-9,10 and 11].
Showing change in surface area of the wound.
| S. No | Wound size at theinitiation of vactherapy (in cm2) | Wound size at thecessation of VACtherapy (in cm2) | Decrease in woundsize attained by VACtherapy (in cm2) |
|---|
| 1 | 30.8 | 20.2 | 10.6 |
| 2 | 38.4 | 26.1 | 12.3 |
| 3 | 64.6 | 50.4 | 14.2 |
| 4 | 32.6 | 22.8 | 9.8 |
| 5 | 27.8 | 22.0 | 5.8 |
| 6 | 92.4 | 68.0 | 24.4 |
| 7 | 5.8 | 3.2 | 2.6 |
| 8 | 22.8 | 14.6 | 8.2 |
| 9 | 94.6 | 80.0 | 14.6 |
| 10 | 6.2 | 3.6 | 2.6 |
| 11 | 54.4 | 36.4 | 18.0 |
| 12 | 118.0 | 100.0 | 18.0 |
| 13 | 54.3 | 68.3 | –14.0 |
| 14 | 36.0 | 28.2 | 7.8 |
| 15 | 30.4 | 20.0 | 10.4 |
| 16 | 48.5 | 61.1 | –12.6 |
| 17 | 40.3 | 32.4 | 7.9 |
| 18 | 56.0 | 41.8 | 14.2 |
| 19 | 42.1 | 32.7 | 9.4 |
| 20 | 40.0 | 29.3 | 10.7 |
| Therapy | At theinitiation ofVAC therapy | At thecessation ofVAC therapy | MeanDecrease inwound sizeattained byVAC therapy | p-value(Paired t-test) |
|---|
| Wound sizeMean ± SD (in cm2) | 46.8±32.28 | 38.055±27.42 | 10.55±2.69 | 0.000413Highly significant |
Showing impact of therapy.
Bacterial cultures were obtained at the initial debridement and before applying the VAC therapy. Bacterial cultures are also taken from the wound during subsequent dressing. The culture specimen reported positive culture for all 20 cases, out of which in 17 samples are positive for staphylococcus aureus, 2 samples were positive for Pseudomonas aeruginosa and 1 sample was positive for Klebsiella. All patient achieved infection control with no sign of infection or active discharge after VAC therapy.
Discussion
The most important issue dealing with open musculoskeletal injury is to restore the outline and healing of the soft tissue as soon as possible. To expedite the wound healing various kind of treatment had been developed for example, topical applications, and antiseptic agents, hyperbaric oxygen, skin grafts or local flaps. Vacuum Assisted Closure (VAC) is a relatively new method of treatment in management of open musculoskeletal wound. The use of VAC to promote wound healing was first documented by Fleischman et al., [9]. The US Food and Drug Administration (FDA) approved the use of VAC for the treatment of non-healing wounds in 1995. Morykwas and Argental et al., suggest negative pressure increases blood flow as evidenced by hyperaemia [2]. They found that the peak blood flow at 125 mm Hg of vacuum setting. Later on their hypothesis was supported by various authors [3–8]. Banwell et al., found immediate application of the VAC following open injury or debridement to produce good results [10].
The exact mechanism by which VAC promote wound healing is still not known, but various hypothesis have been proposed in the literature. The application of negative pressure removes the excess fluids which are known to obstruct the microcirculation and decreases oxygen supply and clearance of locally accumulated toxins. The removal of this excess fluid promotes better capillary circulation and hyperaemia [7]. Morykwas et al., had found that wound with negative pressure application had lower number of organisms per gram of tissue than wound not treated with negative pressure [2]. Thus, he suggested that VAC decreases the bacterial load and the risk of bacterial colonization. In the present study three wounds were infected at the start of VAC therapy. However, all patients were cleared of bacterial infection by the end of VAC therapy.
Urschel et al., proposed that the negative pressure had mechanical effect on the wound bed [11]. The negative pressure causes the contact wound dressing to collapse; the force of this collapse is transferred on to the wound edges; which draws them close together. In the present study there was decrease in wound size attained by VAC therapy ranged from 2.6 to 24.4 cm2, with an average reduction of 11.2 cm2. Similar results were achieved by other authors also. McCallon et al., reported an average decrease in wound surface area of 28.4% (SD 24.3) using topical negative pressure [12]. Joseph et al., reported a significant reduction in wound volume of 78%in the TNP group compared with 30% in the gauze group within 6 weeks (p=0.038) [13].
Alternatively, during the application of negative pressure, tiny pieces of tissue had been shown to be drawn into a foam contact dressing causing micro deformity and mechanical stress, which is thought to stimulate angiogenesis and tissue growth [7].
The main limitation of VAC system is its higher cost of purchase or hire of a VAC unit. However, VAC reduced treatment duration and early wound healing thus reducing the cost [14].
High energy open fractures has higher incidence of loss of soft tissue and infection and required urgent irrigation and debridement. Wound healing was considered as the primary and most clinically relevant in management of these open injuries. Standard wound dressing required prolonged period, repeated debridement, more trauma to granulation tissue and had poor patient compliance. The whole procedure of VAC application converts an open wound into a controlled and temporarily closed compartment with negative pressure uniformly applied over it. Thus VAC therapy provides a sterile, controlled environment that combines the benefit of both open and closed treatment and wound healing take place under moist, clean and sterile conditions [13,15,16].
Limitations
The main limitation of our series is small number of patients, lack of control group, and absence of functional outcome scores.
Conclusion
The proposed technique of vacuum assisted closure therapy using negative pressure is effective in treating soft tissue injuries in open musculoskeletal trauma which after debridement, may present with exposed tendon, fascia or bone. VAC therapy provides a sterile, controlled environment that can lessen the duration of wound healing and decreases the number of secondary procedures for soft tissue coverage and can be used as alternative method in treating soft tissue injuries in open musculoskeletal trauma with better patient compliance.