Introduction
Delivering dental care to young pediatric dental patients can be very challenging [1]. Children who are present at the dental clinic for minor surgical procedures pose a problem for the dentist. Behavioral management alone is unfortunately not sufficient for these children, who can be more compassionately managed with sedation or general anesthesia. Conscious sedation is widely used in dentistry to help anxious patients undergo dental treatment with minimal stress [2]. Immature children, fearful and anxious children, medically and physically disabled children are commonly indicated for conscious sedation technique (AAPD 2006) [3]. Among various routes oral route is the commonly used route. The perfect premedication in children ought to be adequate, fast, and reliable in onset, have negligible symptoms, quick end, and an atraumatic course of administration [4]. The premedicaments utilized for this study were oral midazolam and ketamine 0.5mg/kg and 5mg/kg respectively.
These drugs such as midazolam and ketamine were not available for oral administration in India hence the syrup was made by adding variety of additives which can be taken orally. Conscious sedation with combination methods increases the adequacy and wellbeing, so N2O-O2 can be joined with other routes and agents. Midazolam is an imidazobenzodiazepine that can be given in the dose of 0.5-0.75mg/kg orally. Midazolam meets all the criteria of a premedication drug, i.e., it has fast onset of activity, absence of significant side effects, no impedance with key signs furthermore more powerful in directing patient conduct, making it a good premedication drug [5,6]. Ketamine is a very much recorded anesthetic and analgesic with a wide margin of safety and keeps up defensive reflexes [7]. However there may be a varied reaction and response in the patients after the administration of a combination of drugs.
Aim
The aim of the study was to evaluate and compare the effectiveness of oral Midazolam – N2O and oral Ketamine – N2O by considering various psychological parameters of the child.
Materials and Methods
Thirty cooperative but apprehensive children in the age group of 3-9 years with in the normal range of weight categorized under American Society of Anesthesiology I and II, with multiple primary carious teeth indicated for extraction were selected from the outpatient Department of Pedodontics, St. Joseph Dental College, Eluru. As this study was designed to compare the effectiveness of two drugs in combination with N2O-O2, patients received oral midazolam 0.5mg/kg with N2O-O2 inhalation in the first appointment and oral ketamine 5mg/kg with N2O-O2 inhalation in the follow up appointment. One to two weeks was minimum time interval between two appointments as primary healing of the extraction socket takes a period of minimum two weeks and the patient is advised not to take any hard diet on that side, and this time interval is sufficient for sedation procedure to be carried out on the contra lateral side. Ethical approval for this study was obtained from the local ethical committee. Full verbal and written explanation of the procedure was provided to parents regarding the sedation, type of medication, its safety and side effects. A written consent was obtained from the parent for participation of the child in the study.
Each patient’s medical and dental history was recorded, followed by a detailed clinical and radiographic examination. Their behavior category was assessed by Frankl’s Behavior Rating Scale [Table/Fig-1] [8].
Frankel Behavioral Rating Scale (1962).
| Category | Frankel Behavioral Rating Scale |
|---|
| Rating 1 | Definitely negative: Child refuse treatment, cries forcefully, fearfully, or display any overt evidence of extreme negativism. |
| Rating 2 | Negative: Reluctant to accept treatment and some evidence of negative attitude (not profound). |
| Rating 3 | Positive: The child accepts treatment but may be cautious. The child is willing to comply with the dentist, but may have some reservations. |
| Rating 4 | Definitely positive: This child has a good rapport with the dentist and is interested in the dental treatment. |
Palatable syrup was made by adding sorbitol 45 g, sucrose 15 g, saccharine 0.2 g, sodium benzoate 0.15 g, citrus extract 2 g, and distilled water to convey it to 100 ml [9]. A 10 ml of diluent was titrated to 10 ml of IV drug to achieve a final dose of 0.5mg of Midazolam per ml and 90 ml of diluent is titrated to 10 ml of IV drug to achieve a final dose of 5mg of ketamine per ml for oral use. And N2O-O2 (Quantiflex MDM Relative Analgesia Machine, Matrix medical Inc., Orchard Park, New York, USA.) sedation unit was used for the procedure.
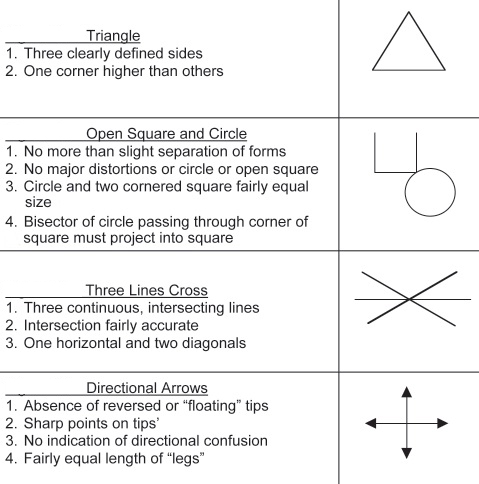
Initially baseline pulse rate, oxygen saturation, respiratory rate and patient’s weight were recorded. The child was shown drawings (Bender Visual Motor Gestalt Test [Table/Fig-2]) and asked to draw the same before the onset of sedation. The scheduled drug oral midazolam in the form of syrup was administered to the patient and the onset of sedation was monitored using Houpt’s Sedation Rating scale [10]. The subjective signs were noted by observing their muscle coordination, look, eye movement, sleep, speech at a regular interval of five minutes after the administration of the drug [11]. After 30 minutes, the picture drawing was (According to Bender Visual Motor Gestalt Test) repeated again. The objective signs and symptoms were noted.
Drawings of Bender Visual Motor Gestalt test.
First, 100% oxygen was delivered for 2 to 3 minutes at an appropriate flow rate. Once the flow rate was achieved, the nitrous oxide was gradually introduced by slowly increasing the concentration at increments of 10% in oxygen to a final dose of 30% in oxygen. Then the objective signs and symptoms were again recorded. According to the site, local anesthesia (2% lidocaine with epinephrine 1:100,000) was given, not exceeding the maximum recommended dosage (4.4mg/kg). Extraction procedure was carried out after five minutes of local anesthetic administration. Hundred percent oxygen was given for three minutes before removal of the nasal mask. As this study was designed to compare the effectiveness of oral midazolam and oral ketamine, the same protocol at first visit was followed but oral ketamine in addition with nitrous oxide and oxygen was used instead of oral midazolam in addition with nitrous oxide and oxygen. All hemodynamic parameters were monitored during the entire course of treatment after sedation and at the end of dental treatment. Before discharge, hemodynamic parameters were recorded and the patient was asked to draw the diagrams as per Bender Test.
Statistical Analysis
All data were tabulated and statistically analyzed using Independent sample t-test to test for its statistical significance.
Results
A total of 30 cooperative but anxious children (3-9 years) were included in the study. On their first visit all patients received 0.5mg/kg oral midazolam with N2O-O2 (Midazolam group) and next visit they received 5mg/kg of oral ketamine with N2O-O2 (Ketamine group) to compare the effectiveness of two drugs. The data were analyzed using t-test and chi-square test.
The pulse rate (beats per minute) and the oxygen saturation (%) scores for both midazolam and ketamine groups immediately after sedation are given in [Table/Fig-3,4] respectively. Both the figures show no significant difference between the midazolam group and ketamine group. The plot of average respiratory rate (in breathes per minute) after sedation for both midazolam and ketamine groups is given in [Table/Fig-5]. The figure shows no significant difference between the two groups.
Comparison of pulse rate between two groups (beats per minute).
| Variable | Group | Mean | SD | t-value | p-value |
|---|
| Base line | Oral midazolam-N2O | 92.3333 | 9.93889 | 0.616 | 0.540 (NS) |
| Oral Ketamine-N2O | 90.7000 | 10.59326 |
| Average value throughout the procedure | Oral midazolam-N2O | 100.2000 | 11.07155 | -0.413 | 0.681 (NS) |
| Oral Ketamine-N2O | 101.5333 | 13.81087 |
| Before discharge/After sedation | Oral midazolam-N2O | 96.3167 | 9.24800 | 0.078 | 0.938 (NS) |
| Oral Ketamine-N2O | 96.1167 | 10.66713 |
NS- Not significant.
Data were analyzed by using t- test.
Comparison of oxygen saturation between two groups (%).
| Variable | Group | Mean | SD | t-value | p-value |
|---|
| Base line | Oral midazolam-N2O | 99.0667 | 1.20153 | 0.654 | 0.516 (NS) |
| Oral Ketamine-N2O | 98.8667 | 1.16658 |
| Average value throughout the procedure | Oral midazolam-N2O | 99.1000 | 0.84486 | -1.027 | 0 .309 (NS) |
| Oral Ketamine-N2O | 99.3000 | 0.65126 |
| Before discharge/After sedation | Oral midazolam-N2O | 99.0833 | 0.74375 | 0.000 | 1.000 (NS) |
| Oral Ketamine-N2O | 99.0833 | 0.70812 |
NS- Not significant.
Data were analyzed by using t- test.
Comparison of respiratory rate between two groups (breaths per minute).
| Variable | Group | Mean | SD | t-value | p-value |
|---|
| Base line | Oral midazolam-N2O | 21.0333 | 2.93003 | -0.633 | 0 .529 (NS) |
| Oral Ketamine-N2O | 21.5333 | 3.18112 |
| Average value throughout the procedure | Oral midazolam-N2O | 23.4667 | 3.31905 | -1.799 | 0.077 (NS) |
| Oral Ketamine-N2O | 24.9000 | 2.83269 |
| Before discharge/After sedation | Oral midazolam-N2O | 22.2667 | 2.46259 | -1.586 | 0.118 (NS) |
| Oral Ketamine-N2O | 23.2333 | 2.25424 |
NS- Not significant.
Data were analyzed by using t- test.
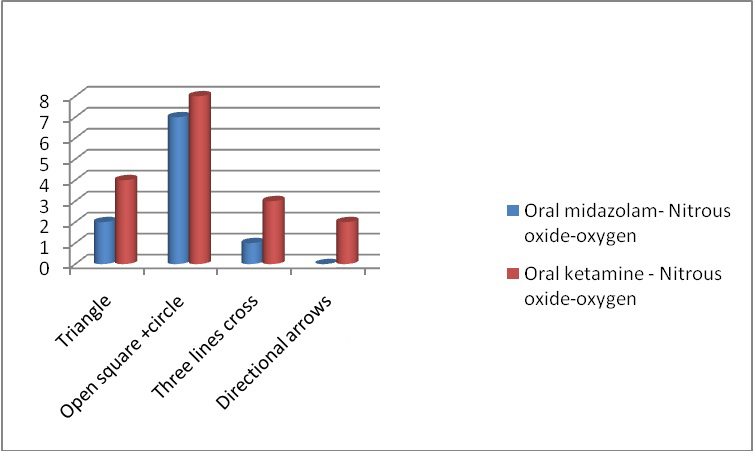
The results of psychomotor test are given in [Table/Fig-6]. Objective signs were noted and tabulated in [Table/Fig-7]. The subjective symptoms are given in [Table/Fig-8]. The results of psychological effects are tabulated and given in [Table/Fig-9]. Comparative data of sensations in the fingers between the two groups is presented in [Table/Fig-10].
Comparative data of psychomotor effects between the two groups.
Comparative data of objective signs between the two groups.
| OBJECTIVE SIGNS | Chi-square value | p-value |
|---|
| Oral midazolam- N2O | Oral ketamine- N2O |
|---|
| After | After | 0.149 | 0.997 (NS) |
| Eyes open | 24 | 26 |
| Smile | 16 | 14 |
| Speaking | 27 | 22 |
| Laughing | 23 | 25 |
| Hands open | 29 | 28 |
| Legs limp | 23 | 22 |
| Abducted feet | 7 | 6 |
NS- Not significant.
Data were analyzed by using Chi-square test.
Comparison of subjective symptoms between the two groups.
| Oral midazolam- N2O | Oral ketamine- N2O | Chi-square | p-value |
|---|
| Feel good | 14 | 11 | 1.781 | 0.879 (NS) |
| Feel Bad | 1 | 3 |
| Feel sleepy | 6 | 7 |
| Feel ok | 4 | 4 |
| Feel Different | 5 | 5 |
| Sensation in lip | 6 | 4 |
NS- Not significant.
Data were analyzed by using Chi-square test.
Comparative data of psychological effects of the two groups.
| HEAD | Oral midazolam- N2O | Oral ketamine- N2O | Chi-square | p-value |
|---|
| Tingly | 8 | 7 | 0.169 | 0.919 (NS) |
| Light | 9 | 6 |
| Ok | 13 | 11 |
| Heavy | 0 | 6 |
NS- Not significant.
Data were analyzed by using Chi-square test.
Comparative data of sensations in the fingers between the two groups.
| FINGERS | Oral midazolam- N2O | Oral ketamine- N2O | Chi-square | p-value |
|---|
| Tingly | 23 | 21 | 0.382 | 0.826 (NS) |
| Warm | 2 | 3 |
| Cold | 0 | 0 |
| Light | 5 | 6 |
NS- Not significant.
Data were analyzed by using Chi-square test.
There was no statistical difference between the two groups with respect to objective signs (p=0.997), subjective symptoms (p=0.879), psychological effect (p=0.919) and sensation in the finger (p=0.826).
Discussion
The pediatric dentist uses a wide variety of techniques to alleviate fears of children and improve their cooperation while getting dental treatment done. But still in some children safe, fast and non-traumatic dental treatment is needed and thus pharmacological management in the form of sedation is recommended. Sedation is commonly indicated for fearful and physical or mentally handicapped children [3]. Among different methods of medication administration, oral premedication was decided for this study as this is more suitable, most safe and easiest method of medication administration. Advantages of oral drug administration are that they are more acceptable, safe, have minimal side effects, minimal equipment and no specialized training [3,12].
Midazolam is administered in the oral measurements of 0.5-0.75 mg/kg and 3-10 mg/kg of ketamine administered orally, has a high margin of safety as the defensive reflexes are normally kept up [13]. Oral midazolam at the dose of 0.5mg/kg has shown to produce good anxiolysis when used as premedication [2]. And reported rare side effects associated with oral midazolam usage for behavior management [14]. Oral ketamine at 5mg/kg provides safe, successful, high-quality sedation for young children undergoing dental extractions under local anesthesia [15]. Hence in the present study 0.5mg/kg of oral midazolam and 5mg/kg oral ketamine dosage was administered to compare their efficacy in dental treatment of children.
In India there is no availability of midazolam and ketamine to administer orally. Hence intravenous preparation has been used orally. However, it has an extremely bitter taste. Hence, intravenous preparations of the above drugs were modified to make them palatable when taken orally by adding a variety of additives. The drugs were administered 45 minutes before the treatment to ensure adequate level of sedation [10].
Theoretically, under most circumstances, the addition of nitrous oxide to a combination of sedative agents results in the reduced need for higher doses of the other agents, attaining the same sedation end point because of the potential effect of nitrous oxide. According to Fniash M, levels of 30% and above N2O provide an adequate level of sedation without the risk of over sedation [16].
Children in the age group of 3-9yrs were selected so as to have the capability to draw at least one figure on the psychomotor evaluation component [17]. The general health of ASA I and II patients is reasonably good and there is minimal likelihood that the physiologic stresses of the dental procedure, or local anesthetics and sedative will precipitate a significant medical complication [18]. Psychomotor impairment is an imperative marker of drug impact and recovery from a drug. Psychomotor effects were evaluated with a modified Bender Visual Motor Gestalt Test [10].
The parameters like pulse, respiratory rate, oxygen saturation (SaO2), level of sedation were recorded just before the administration of sedative and the same were monitored once the sedative has been administered and at the end of the procedure. One study reported that in some children there was increase in blood pressure, pulse and respiratory rate over time, where as in others there was an initial increase in vital signs followed by a decrease [19]. According to another study heart rate and respiratory rate were marginally higher in children who were administered 5mg/kg of oral ketamine contrasted with 0.5mg/kg of oral midazolam [20]. In the present study, respiratory rate was increased after ketamine sedation than midazolam and pulse rate marginally increased after midazolam sedation than with ketamine. However comparing midazolam and ketamine with respect to pulse and respiratory rates, there was statistically no significant difference between the two drugs.
In the present study by comparing oral midazolam- N2O-O2 and oral ketamine - N2O-O2 with respect to oxygen saturation there was statistically no significant difference between the two drugs. Houpt M et al., had evaluated the psychomotor effects of the drugs - used in combination with N2O sedation, and his study reported that N2O have no significant effect on psychomotor performance [10]. In the present study psychomotor effects were evaluated by using Bender Visual Motor Gestalt Test. The children were made to draw diagrams (triangles, open square/circle, three lines cross, and directional arrows) pre and post sedation. On comparison of the psychomotor effects between the two groups oral midazolam - N2O group performed marginally better than oral ketamine –N2O. Oral midazolam at a dose of 0.5 mg/kg produces minimal side effects and successful premedicament and on the other hand, 5mg/kg oral ketamine provides high margin of safety as the protective reflexes are usually maintained [13,21].
Limitation
Limitations of this study were in steady with other comparative studies. A few students were involved in the treatment and assessment and they were not prepared particularly for institutionalization of patient evaluation. Besides, the procedure was supervised by experienced faculty member and data were collected according to AAPD guidelines. Further studies need to be conducted in the light of present situation, to arrive at a definite conclusion.
Conclusion
Oral midazolam – N2O and oral ketamine N2O as sedative regimens were found to be safe and effective and their use greatly reduced the patient anxiety during the therapeutic procedure. Overall the findings in the present study suggested that no significant difference was observed pertaining to pulse rate, oxygen saturation, respiratory rate, psychological effects, objective signs and subjective symptoms. However, psychomotor effect of the midazolam group appeared marginally better than ketamine group.
NS- Not significant.
Data were analyzed by using t- test.
NS- Not significant.
Data were analyzed by using t- test.
NS- Not significant.
Data were analyzed by using t- test.
NS- Not significant.
Data were analyzed by using Chi-square test.
NS- Not significant.
Data were analyzed by using Chi-square test.
NS- Not significant.
Data were analyzed by using Chi-square test.
NS- Not significant.
Data were analyzed by using Chi-square test.
[1]. Lee-Kim SJ, Fadavi S, Punwani I, Koerber A, Nasal versus oral midazolam sedation for pediatric dental patientsJ Dent Child 2004 71:126-30. [Google Scholar]
[2]. Wilson KE, Welburry RR, Girdler NM, A study of the effectiveness of oral midazolam sedation for orthodontic extraction of permanent teeth in children: a prospective, randomized, controlled, crossover trialBr Dent J 2002 192:457-62. [Google Scholar]
[3]. Dock M, Creedon RL, Pharmacological management of patient behavior. In:Mc Donald RE, Avery DRDentistry for the child and adolescent 1983 4th edSt.LouisCV Mosby Co:298 [Google Scholar]
[4]. Sen S, Thakurta RG, Gupta SD, Bhattacharya S, Mukherji S, Preoperative anxiolysis in pediatric population: a comparative study between oral midazolam and oral ketamineAnesth Essays Res 2013 7(2):200-05. [Google Scholar]
[5]. Shabbir A, Bhatt SS, Sundee Hegde K, Saman M, Comparison of oral midazolam and triclofos in conscious sedation of uncooperative childrenJ Clin Pediatr Dent 2011 36(2):189-96. [Google Scholar]
[6]. Gupta R, Sharma K, Dhiman UK, Effect of a combination of oral midazolam and low dose ketamine on anxiety, pain, swelling and comfort during and after surgical extractions of mandibular third molarsIndian J Dent Res 2012 23:295-96. [Google Scholar]
[7]. Sekeric Donmez A, Ates Y, Okten F, Oral ketamine premedication in children (Placebo controlled double blind study)Eur J Anaesthesiol 1996 13:606-11. [Google Scholar]
[8]. Frankl SN, Shiere FR, Fogels HR, Should the parents remain with the child in the dental operatory?J Dent Child 1962 2:150-63. [Google Scholar]
[9]. Al-Zahrani AM, Wyne AH, Sheta SA, Comparison of oral midazolam with a combination of oral midazolam and nitrous oxide-oxygen inhalation in the effectiveness of dental sedation for young childrenJ Indian Soc Pedod Prev Dent 2009 27:9-16. [Google Scholar]
[10]. Houpt M, Limb R, Livingston R, Clinical effects of nitrous oxide conscious sedation in childrenPediatr Dent 2004 26:29-36. [Google Scholar]
[11]. Smith BM, Cutilli BJ, Saunders W, Oral midazolam: pediatric conscious sedationCompend Contin Educ Dent 1998 19(5868):590-92. [Google Scholar]
[12]. Malamad SF, Oral sedation. In: Malamad SF, Quinn CLSedation: a guide to patient management 2003 4th edSt. LouisMosby Year Book:89 [Google Scholar]
[13]. Alfonzo- Echeverri EC, Berg JH, Wild TW, Glass NL, Oral ketamine for pediatric outpatient dental surgery sedationPediatr Dent 1993 15:182-85. [Google Scholar]
[14]. Papineni A, Lourenco-Matharu L, Ashley PF, Safety of oral midazolam use in paediatric dentistry: a reviewInt J Paediatr Dent 2014 24(1):2-13. [Google Scholar]
[15]. Roelofse JA, de V JJJ, Roelofse PGR, A double blind randomized comparison of midazolam alone and midazolam combined with ketamine for sedation of pediatric dental patientsJ Oral Maxillofac Surg 1996 54:838-44. [Google Scholar]
[16]. Fnaish M, Nitrous oxide oxygen inhalation sedation in pediatric dentistryJournal of Research in Medical Sciences (JRMS) 2010 17:38-42. [Google Scholar]
[17]. Houpt MI, Koenigsberg SR, Weiss NJ, Desjardins PJ, Comparison of chloral hydrate with and without promethazine in the sedation of young childrenPediatr Dent 1985 7:41-46. [Google Scholar]
[18]. Jackson LD, Jhonson BS, Conscious sedation for dentistry: risk management and patient selectionDent Clin North Am 2002 46:767-80. [Google Scholar]
[19]. Cote JC, Cohen IT, Suresh S, Rabb M, Rose JB, Weldon C, A comparison of three doses of commercially prepared oral midazolam syrup in childrenAnesth Analg 2002 94:37-43. [Google Scholar]
[20]. Damle SG, Gandhi M, Laheri V, Comparison of oral ketamine and oral midazolam as sedative agents in pediatric dentistryJ Indian Soc Pedod Prev Dent 2008 26:97-101. [Google Scholar]
[21]. Millan Mc, Schopfer S, Sikich RN, Hartley E, Lerman J, Premedication of children with oral midazolamCan J Anaesth 1992 39:545-50. [Google Scholar]