A Case of Pleuroparenchymal Metastasis: Rare Aetiology
Subramanian Suriyan1, Radhika Sharma2, Meenakshi Narasimhan3, Aruna Shanmuganathan4, Adhithyan Rajendran5
1 Associate Professor, Department of Respiratory Medicine, Chettinad Hospital and Research Institute, Chennai, India.
2 Post Graduate, Department of Respiratory Medicine, Chettinad Hospital & Research Institute, Chennai, India.
3 Professor & HOD, Department of Respiratory Medicine Chettinad Hospital & Research Institute, Chennai, India.
4 Professor, Department of Respiratory Medicine, Chettinad Hospital & Research Institute, Chennai, India.
5 Assistant Professor, Department of Radiology, Chettinad Hospital & Research Institute, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subramanian Suriyan, 80 Third Street, TTK Nagar, Irumbuliyur, West Tambaram, Chennai-600045, Chennai, India.
E-mail: drssmani@gmail.com
A phyllodes tumour is a malignancy of both mesenchymal and epithelial origin affecting the breast. The malignant course of this breast tumour causing lung metastasis is rare. Here we report a treated case of borderline phyllodes tumour that presented with pleuroparenchymal metastasis. Our case highlights the possibility of recurrence of borderline phyllodes tumour as pleuroparenchymal metastasis even after a long disease free interval.
Immunohistochemistry, Phyllodes tumour, Recurrence
Case Report
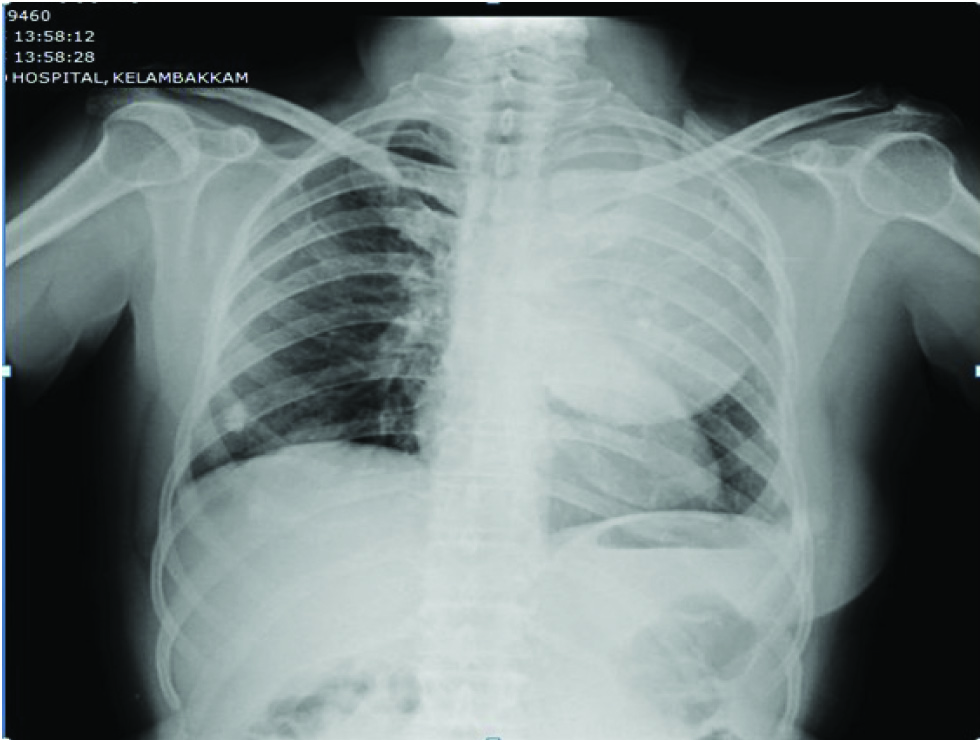
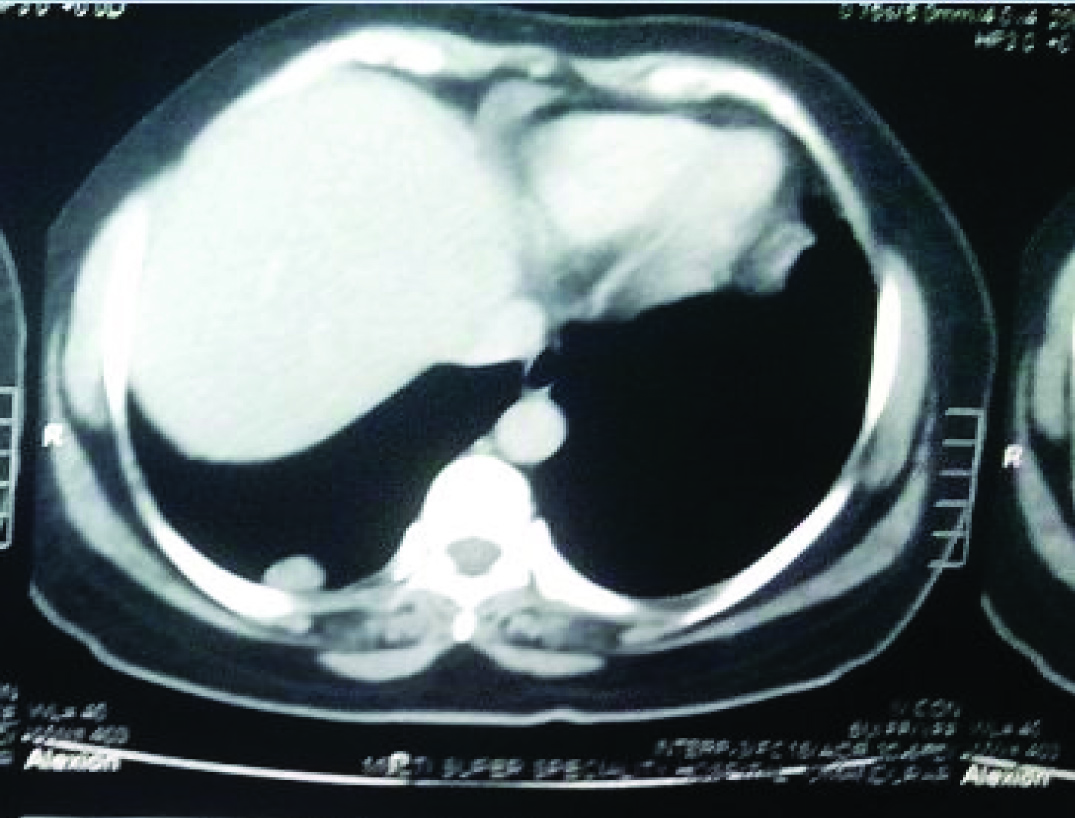
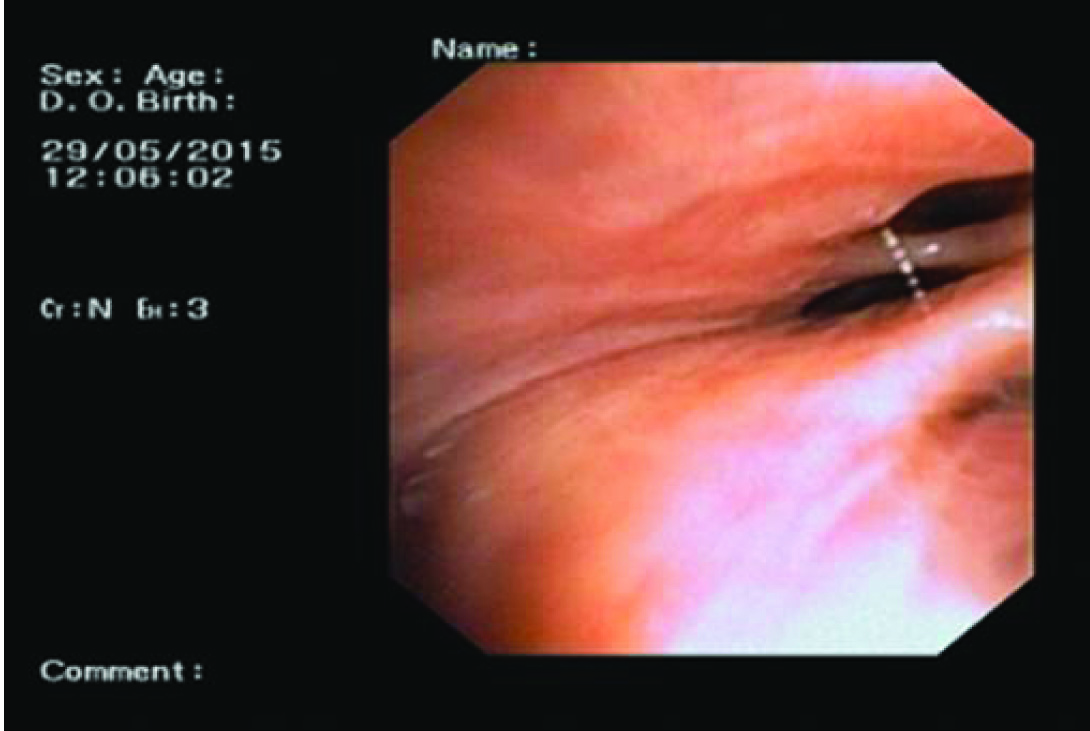
A 58-year-old post menopausal woman presented with complaints of dull aching pain in the posterior aspect of the chest wall for three months. Patient had past history of borderline phyllodes tumour of breast diagnosed on July 2009 and had undergone right mastectomy followed by chemotherapy and radiotherapy for which she was on follow-up till August 2013. Whole body bone scintigraphy done in August 2013 showed no evidence of bony metastasis. Patient was lost to follow up since then and was asymptomatic till three months before she reported to us. Chest X-ray [Table/Fig-1] revealed a well-defined homogenous opacity involving the left upper and mid zone. A small nodular opacity was noted in the right lower zone with absence of breast shadow. Computed Tomography thorax done revealed a large pleural based soft tissue density lesion extending from apicoposterior segment of the left upper lobe to superior basal segment of the left lower lobe [Table/Fig-2,3]. A nodule was also noted in the right lower lobe measuring 1.2 cm × 2.4 cm in the posterior basal segment of right lower lobe [Table/Fig-4]. Bronchoscopy revealed sluggish left vocal cord movements, distorted architecture of carina, and narrowed left upper lobe bronchus along with flattened and stretched bronchus of the lingular segment. The upper lobe bronchus could not be negotiated beyond the narrowing [Table/Fig-5,6]. All the above findings suggested the possibility of external compression of left upper lobe bronchus. Bronchoalveolar lavage sent for analysis revealed no evidence for malignancy or infection. Computed Tomography guided biopsy of the left sided mass lesion showed spindle cells with atypia in sheets and bundles on a myxoid stroma, delicate to broad collagen bundles with few dilated congested capillaries [Table/Fig-7]. No lung parenchyma was seen. Further immunohistochemistry staining was positive for vimentin, negative for ER (Estrogen Receptor), PR (progesterone receptor) & TTF (Thyroid transcription Factor). The Haematoxylin & Eosin staining, immunohistochemistry features were in favour of metastatic tumour. Clinical breast examination and mammography were normal. With the history of treated phyllodes tumour and confirmation by histopathological examination and immunohistochemistry we conclude that the mass present in the left side and the nodule of the right lower lobe as metastasis of the breast phyllodes tumour. After explaining the diagnosis and prognosis to the patient and their relatives, patient was started on chemotherapy under oncology care. Patient received six cycles of Paclitaxel, Epirubicin and cyclophosphamide with only partial response. Patient developed cardiac dysfunction, probably as a side effect of Epirubicin. So chemotherapy was withheld and patient is on symptomatic therapy at present.
CXR-PA view Lt. sided homogenous opacity in upper and middle zone with Nodular opacity in Rt. Lower zone.
CT-Thorax Lung window showing pleural based soft tissue density occupying the apicoposterior segment of the left upper lobe.
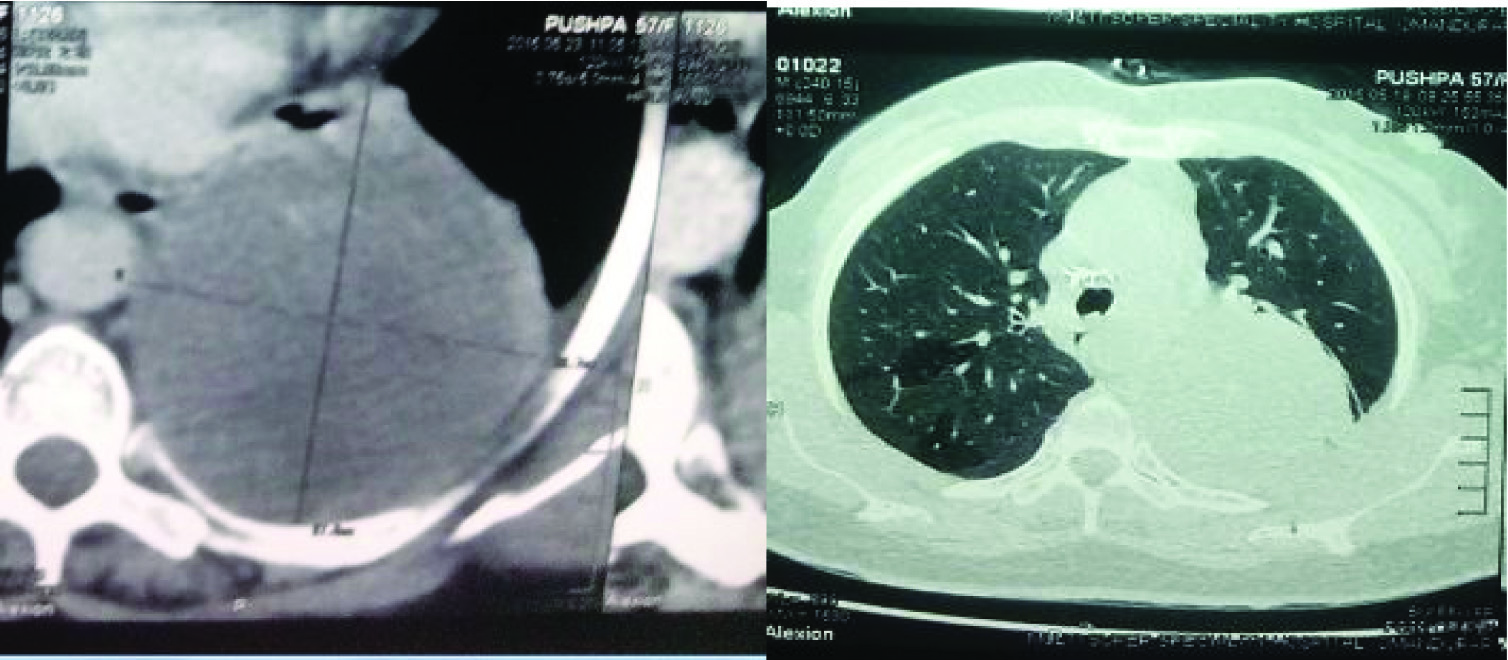
Nodule in right lower lobe measuring 1.2 × 2.4 cm in the posterior basal segment.
FOB showing narrowed left upper lobe bronchus.
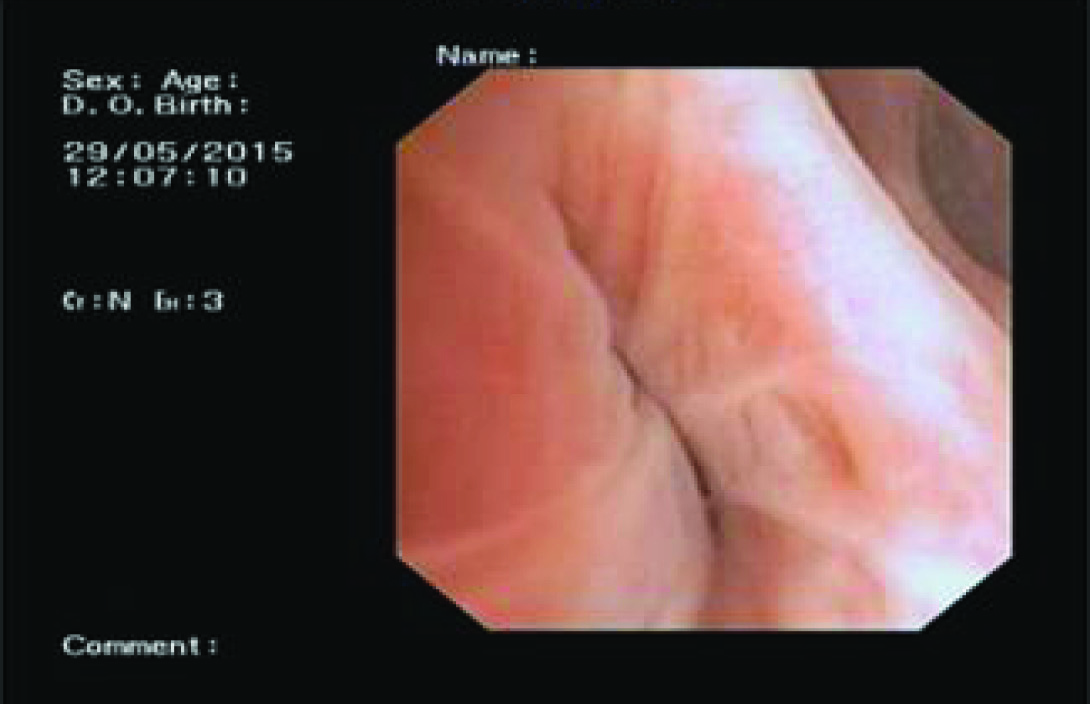
FOB showing stretched bronchus of the lingular segment.
Spindle cells with atypia in sheets and bundles on a myxoid stroma, delicate to broad collagen bundles with few dilated congested capillaries

Consent has been obtained from the patient regarding the publication of this case report.
Discussion
Phyllodes tumour is a rare entity of breast tumour accounting for less than 1% of all breast cancers [1]. This tumour may pursue a benign or malignant course where metastasis is possible in the latter. The common sites of metastases are the lung, pleura and bones [2,3]. Phyllodes tumour can be classified into benign, borderline and malignant categories based on histology [4]. Only the borderline and malignant variant metastasizes. An 8% of borderline [5] and 20%of malignant tumours will metastasize [6]. Common sites of metastasis are lung (66%) [7], pleura and bone. Ours is a case of borderline phyllodes with metastases to lung and pleura. Similar to our case Solberg et al., have reported a case of pulmonary metastasis of phyllodes tumour of breast after 14 months of mastectomy [8]. Ganti et al., have also reported a case of solitary pulmonary metastasis in the left chest seven years after a right-sided mastectomy for malignant phyllodes tumour [9]. Fujii et al., also reported a case of pulmonary metastasis 18 years after mastectomy [10]. Alfa-Wali et al., has reported huge visceral pulmonary metastases from phyllodes tumour of breast with a large left costophrenic mass on CT which revealed the features of phyllodes as in our case [11]. Unlike the above case reports our case had a huge pleural-based mass in the left side as well as another parenchymal nodule in the right lower lobe. However, there have been some reports of pleural involvement in literature. Bucaloiu et al., have reported pleural metastasis in the case of recurrent phyllodes tumour [12]. Filosso et al., has reported a similar case of giant pleural metastasis of malignant phyllodes tumour [13]. The other unusual finding noted in our case was the presence of left vocal cord palsy in bronchoscopy, which is very rare and not yet reported in the literature to the best of our knowledge.
Metastatic phyllodes tumour has very few treatment options. Phyllodes tumour in metastatic setting has limited role of surgery, radiotherapy and chemotherapy or combined treatment. Our patient underwent six cycles chemotherapy with only minimal improvement. However, in some selected patients, palliative surgery may be considered to provide a better quality of life to the patient.
Conclusion
Based on our case and above-mentioned reports, we suggest with the presence of pleuroparenchymal metastatic lesions with occult primary, the possibility of phyllodes tumour of the breast should be considered. We also recommend a long-term regular follow-up of patients diagnosed with borderline/malignant phyllodes even after surgical excision and adequate chemo radiotherapy.
[1]. Mangi AA, Smith BL, Gadd MA, Tanabe KK, Ott MJ, Souba WW, Surgical management of phyllodes tumoursArchives of surgery (Chicago, Ill: 1960) 1999 134(5):487-92. [Google Scholar]
[2]. Hawkins RE, Schofield JB, Fisher C, Wiltshaw E, McKinna JA, The clinical and histologic criteria that predict metastases from cystosarcoma phyllodesCancer 1992 69(1):141-47. [Google Scholar]
[3]. Cohn-Cedermark G, Rutqvist LE, Rosendahl I, Silfversward C, Prognostic factors in cystosarcoma phyllodes. A clinicopathologic study of 77 patientsCancer 1991 68(9):2017-22. [Google Scholar]
[4]. Moffat CJ, Pinder SE, Dixon AR, Elston CW, Blamey RW, Ellis IO, Phyllodes tumours of the breast: a clinicopathological review of thirty-two casesHistopathology 1995 27(3):205-18. [Google Scholar]
[5]. Wei J, Tan YT, Cai YC, Yuan ZY, Yang D, Wang SS, Predictive factors for the local recurrence and distant metastasis of phyllodes tumours of the breast: a retrospective analysis of 192 cases at a single centerChin J Cancer 2014 33(10):492-500. [Google Scholar]
[6]. Parker SJ, Harries SA, Phyllodes tumoursPostgrad Med J 2001 77(909):428-35. [Google Scholar]
[7]. Takahashi M, Murata K, Mori M, Kawaguchi N, Furukawa A, Kushima R, Giant metastatic cystosarcoma phyllodes to the lung: CT and MR findingsRadiation medicine 1992 10(5):210-13. [Google Scholar]
[8]. Solberg OG, Blom GP, Stavem K, A patient with pulmonary metastasis of phyllodes tumour of the breast 2005 125(21):2956-57. [Google Scholar]
[9]. Ganti S, Svennevik E, Ali FS, Anikin V, Successful resection of giant solitary pulmonary metastasis from a phyllodes tumourAnn Thorac Surg 2007 84(5):1750-52. [Google Scholar]
[10]. Fujii T, Yajima R, Yamaki E, Kohsaka T, Yamaguchi S, Tsutsumi S, Pulmonary metastasis from breast cancer with an 18-year disease-free interval: implication of the role of surgeryInt Surg 2012 97(4):281-84. [Google Scholar]
[11]. Alfa-Wali M, Luckraz H, Gibbs AR, Butchart EG, A rare case of a large visceral pleural metastatic phyllodes tumourRespiratory Medicine CME 2008 1(1):59-60. [Google Scholar]
[12]. Bucaloiu ID, Murphy T, Brown R, Siegelmann-Danieli N, Cystic-appearing pleural metastasis in a patient with recurrent phyllodes tumourThe Breast Journal 2005 11(6):482 [Google Scholar]
[13]. Filosso PL, Turello D, Pernazza F, Ruffini E, Oliaro A, Radical surgical resection of a giant pleural metastasis of a malignant phyllodes tumour of the breastJ Thorac Cardiovasc Surg 2005 130(6):1707-08. [Google Scholar]