Vagal Schwannoma: A Rare Parapharyngeal Tumour
Panduranga M Kamath1, Deviprasad Dosemane2, Suja S Sreedharan3, Nazeem A Majeed4, Vijendra S Shenoy5
1 Professor, Department of ENT, Kasturba Medical College, Mangalore, Manipal University, India.
2 Associate Professor, Department of ENT, Kasturba Medical College, Mangalore, Manipal University, India.
3 Professor, Department of ENT, Kasturba Medical College, Mangalore, Manipal University, India.
4 Assistant Professor, Department of ENT, Kannur Medical College, Anjarakkandy, India.
5 Associate Professor, Department of ENT, Kasturba Medical College, Mangalore, Manipal University, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deviprasad Dosemane, House No. A-14, KMC (RNE) staff quarters, Light House Hill road, Mangalore- 575003, India. E-mail : dr.deviprasad@yahoo.co.in
Among the parapharyngeal tumours, salivary gland tumours are the commonest, followed by schwannomas, which are slow growing benign tumours. Half of the parapharyngeal schwannomas originate from the vagus. Complete surgical excision is the treatment of choice. We hereby present two cases of parapharyngeal schwannomas, one which had presented as an intraoral mass and the other as a swelling in the neck. The first case, a 57-year-old female patient complained of a slowly increasing swelling in the left side of the throat since 3 months, associated with pain and dysphagia. In the Contrast Enhanced CT scan of the neck, a well-defined cystic lesion with central enhancing solid components (4cm X 4.5cm X 3cm) was seen in the left parapharyngeal region. The second case, a 39-year-old male patient complained of a painless, gradually increasing swelling below the lobule of the right ear since one month. Examination revealed a solitary, nontender, firm and mobile swelling of 2cm X 2cm below the lobule of the right ear. In Contrast Enhanced CT scan of the neck, an enhancing lesion was seen involving the right parapharyngeal space, post-styloid compartment. Both the patients underwent trans-cervical surgical excision. Vagal nerve schwannoma is rare. The majority of the cases present with a slow growing neck swelling without neurological deficit. Complete surgical excision of the tumour is important to prevent recurrence.
Parapharyngeal space, Vagus nerve
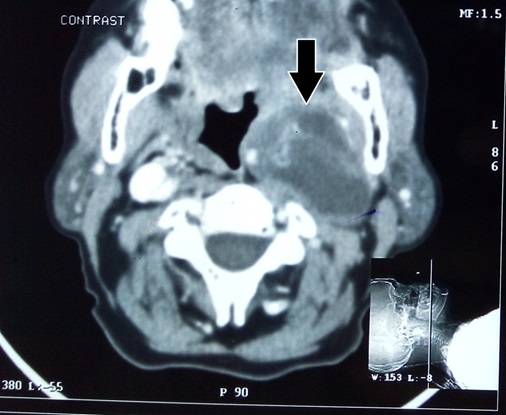
Case Report 1
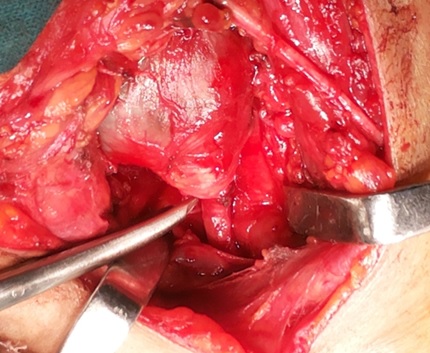
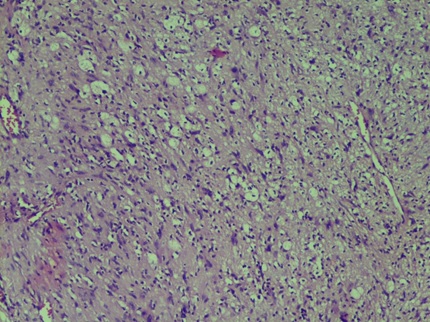
A 57-year-old lady complained of a swelling inside the throat, on the left side for last three months, which was slowly progressing in size. During the same period she had giddiness, which occurred only on deglutition. She had associated pain and difficulty on swallowing. She was treated for pulmonary tuberculosis 15 years back. She was a hypertensive on treatment. Examination revealed a bulge in the left tonsillar fossa pushing the tonsil medially. The overlying mucosa was normal. There was no palpable swelling in the neck. Contrast Enhanced CT scan of the neck showed a well-defined cystic lesion with central enhancing solid components (4 cm x 4.5 cm x 3 cm) in the left parapharyngeal space and carotid space [Table/Fig-1]. The lesion was displacing the carotid vessel medially and the jugular vessel laterally. The parapharyngeal mass was trans-cervically excised. Intraoperatively, a well encapsulated mass of 4 cm x 3 cm x 2 cm was seen occupying the left parapharyngeal region, extending upto the skull base [Table/Fig-2]. The mass was pushing the external carotid artery medially and the internal carotid artery inferiorly. It was seen to be arising from the vagus nerve and was inseparable from it. The hypoglossal nerve was seen to be coursing over the mass. Postoperatively, the patient developed palsy of the left vocal cord and left hypoglossal nerve. Histopathology showed an encapsulated tumour comprising of proliferating spindle cells in a palisading pattern. The nuclei were wavy and spindle shaped with occasional pleomorphic nucleoli [Table/Fig-3]. The features were consistent with schwannoma. Patient is on regular follow-up for last 8 months and the voice has improved as the right vocal cord is compensating for the phonatory gap.
Contrast Enhanced CT scan (axial section) showing the left parapharyngeal mass (arrow).
Intraoperative view of the left parapharyngeal mass (scissor tip is pointing at the vagus nerve, where the tumour is arising).
Photomicrograph showing encapsulated tumour comprising of proliferating spindle cells in a palisading pattern.
Case Report 2
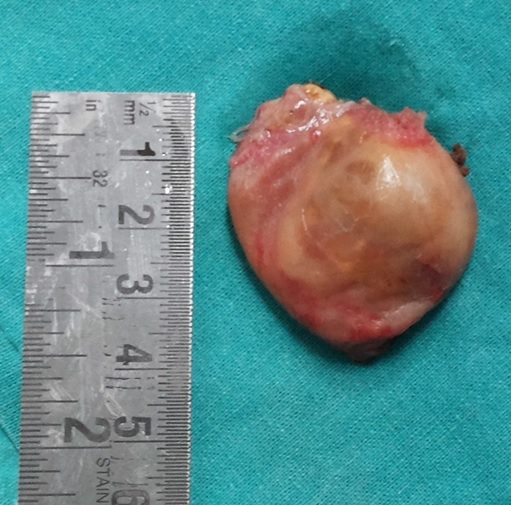
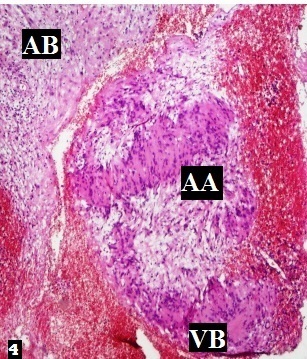
A man aged 39-year-old reported with a swelling below the lobule of the right ear since one month. The swelling had no pain and was gradually increasing in size. Examination revealed a solitary swelling of 2 cm x 2 cm in size below the lobule of the right ear. The swelling was non tender, firm in consistency and mobile. There was no visible swelling within the oral cavity and oropharynx. CT scan of the neck demonstrated an enhancing lesion in the post styloid compartment of the right parapharyngeal region, adjacent to the right carotid bifurcation [Table/Fig-4]. The patient underwent surgical excision of the tumour through the trans-cervical route. Intraoperatively, a well encapsulated mass of 3 cm x 3 cm x 2 cm [Table/Fig-5] was seen superolateral to the carotid bifurcation, attached to and arising from the vagus nerve. Postoperatively, there was paralysis of right vocal cord, marginal mandibular and hypoglossal nerves. Histopathological evaluation showed an encapsulated tumour with spindle cells. Antoni A (AA) and Antoni B (AB) areas were seen with Verocay bodies (VB) [Table/Fig-6]. The features were consistent with a schwannoma. Patient is on regular follow-up for last 7 months and the voice has improved as the left vocal cord is compensating for the phonatory gap.
Contrast Enhanced CT scan (axial section) showing the right parapharyngeal mass (arrow).

Postoperative view of the specimen of right parapharyngeal mass.
Photomicrograph showing encapsulated tumour comprising of spindle cells. AA=Antoni A area, AB=Antoni B area and VB=Verocay bodies.
Discussion
Tumours of parapharyngeal space are rare. Of all the head and neck tumours, they account for only 0.5%. The common parapharyngeal tumours are minor salivary gland tumours, schwannomas and paragangliomas. Schwannomas are usually seen in the following sites-face, scalp, intracranial cavity, orbit, nasal and oral cavity, mastoid, parapharyngeal region and larynx [1]. Parapharyngeal schwannoma was first reported in 1933 by Figi [2]. It is considered to arise from either schwann cells or fibroblasts. Parapharyngeal schwannomas arise from the tenth cranial nerve or cervical sympathetic trunk. Most of the parapharyngeal tumours are benign and slow growing [3]. They usually occur between 2nd and 6th decade. There is no sex predilection for vagal schwannomas [4]. The clinical presentation depends on the anatomic site of the tumour in head and neck. The superior ganglion of the vagus is located within the jugular foramen whereas the inferior ganglion is located at the extra-cranial opening of the foramen. The schwannomas arising from superior ganglion will end up having intracranial extension and those arising from the inferior ganglion will have extracranial extension [5]. Based on this hypothesis, our patients would have the tumour originating from the inferior ganglion of the vagal nerve. Usually the mass is painless. This finding is consistent with our patients. The swelling is freely mobile but attachment to a large nerve may restrict the movements. Benign and malignant tumours may be differentiated by FNAC but in the diagnosis of neural tumours, it has low accuracy [6]. Some schwannomas may be very vascular, so contrast enhanced CT should be done in these cases. Schwannomas of cervical sympathetic nerve displace both carotid and jugular vessels, without separating them [7], whereas carotid arteries are usually separated from the internal jugular vein in vagus nerve schwannomas. Complete surgical excision is the treatment for vagus nerve schwannoma [8]. Transcervical, transcondylar; cervical, trans-mastoid or infra-temporal fossa approach can be used for tumours confined to the neck (with no intracranial extension). For tumour involving the jugular foramen, subcapsular extirpation via enlarged jugular foramen is employed. In our patients, transcervical approach was used despite of the tumour involving the right jugular foramen and parapharyngeal space. To prevent recurrence, the tumour should be excised with its capsule. Hoarseness was reported in most of the patients, while vocal cord paralysis happened in 85% of patients after tumour resection [8]. In our cases, the patients developed right vocal cord palsy and hypoglossal nerve palsy postoperatively.
Conclusion
Schwannoma of vagus nerve is rare. Most of the patients present with a slowly progressive neck swelling and show no neurological deficit. Contrast enhanced CT scan is usually adequate for an appropriate diagnosis but MRI is the gold standard investigation. Complete surgical excision of the tumour is important to prevent recurrence. Vocal paralysis is the most common postoperative complication.
[1]. Girish G, Shrinivas S, Vanaki R, Puranik S, Schwannoma of Parapharyngeal SpaceJ Maxillofac Oral Surg 2010 9(2):182-85. [Google Scholar]
[2]. Neville BW, Damm DD, Allen CM, Bouqot JE, Oral and maxillofacial pathology 2002 2nd ednPhiladelphiaW. B. Saunders:456-57. [Google Scholar]
[3]. Chang SC, Schi YM, Neurilemmoma of the vagus nerve. A case report and brief literature reviewLaryngoscope 1984 94(7):946-49. [Google Scholar]
[4]. Gilmer-Hill HS, Kline DG, Neurogenic tumours of the cervical vagus nerve: report of four cases and review of the literatureNeurosurg 2000 46(6):1498-503. [Google Scholar]
[5]. Chiun KC, Tang IP, Prepageran N, Jayalakshmi P, An extensive cervical vagal nerve schwannoma: a case reportMed J of Malaysia 2012 67(3):342-44. [Google Scholar]
[6]. Garg MK, Garg U, Aggrawal D, Rana P, “Schwannoma of Neck”Journal of Mahatma Gandhi Institute of Medical Sciences 2013 18(1):74-77. [Google Scholar]
[7]. Saito DM, Glastonbury CM, El-Sayed IH, Eisele DW, Parapharyngeal space schwannomas: preoperative imaging determination of the nerve of originArch Otolaryngol Head Neck Surg 2007 133(7):662-67. [Google Scholar]
[8]. Khafif A, Segev Y, Kaplan DM, Gil Z, Fliss DM, Surgical management of parapharyngeal space tumours: a 10-year reviewOtolaryngol Head Neck Surg 2005 132(3):401-06. [Google Scholar]