Gynaecological Perspective of Schwannoma: A Rare Pelvic Tumour
Neranjana Padmanaban1, Priya Subash Chandrabose2, Muthuvel Esakki3, Hephzibah Kirubamani4, Chitra Srinivasan5
1 Senior Resident, Department of Obstetrics and Gynecology, Saveetha Medical College and Hospital, Chennai, India.
2 Assistant Professor, Department of Pathology, Saveetha Medical College and Hospital, Chennai, India.
3 Associate Professor, Department of Pathology, Saveetha Medical College and Hospital, Chennai, India.
4 Professor, Department of Obstetrics and Gynecology, Saveetha Medical College and Hospital, Chennai, India.
5 Professor, Department of Pathology, Saveetha Medical College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hephzibah Kirubamani, 58/2, Paripoorna Vinayagar Koil Street, Mylapore, Chennai – 600 004, India.
E-mail: hepsi1002@yahoo.co.in
Schwannomas are benign tumours that arise from Schwann cells of nerve fibres. They commonly occur in the head, neck, mediastinum and extremities but pelvic occurrence is rare. We report a rare case of retroperitoneal tumour with Gynaec presentation. A 26-year-old parous woman was admitted with abdominal mass, pain abdomen, painful menstruation and painful coitus for one year. Abdominal examination revealed firm mass filling the lower abdomen with restricted mobility. On bimanual examination cervix was hitched against pubic symphysis. Mass felt through anterior and left adnexa not tender, uterus felt close to the mass about 8-10 weeks size, right adnexa free. USG revealed broad ligament fibroid with cystic right ovary. Hence myomectomy was planned, but intraoperatively it was found that the mass was filling the pelvis close to bulky uterus with cystic right ovary. After informed consent while proceeding with hysterectomy, necrotic, yellow colour material came out from the capsule like structure of the mass which was close to lower part of posterior wall of uterus. Mass was removed except which was adherent to deeper structure left behind. Histopathological examination revealed Schwannoma undergoing cystic degeneration. Since Schwannoma was mostly diagnosed incidentally, high degree suspicion is necessary for diagnosis.
Benign, Neurogenic, Pelvis
Case Report
A 26-year-old P3L3 completed family, presented to the OPD with history of pain abdomen and mass abdomen. She had history of painful menstruation, but no history of menorrhagia in her previous menstrual cycles and painful coitus since 6 months. Physical examination was unremarkable.
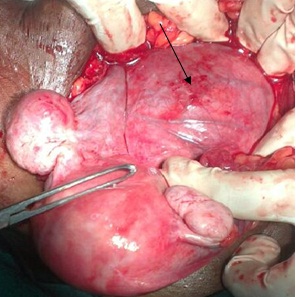
On abdominal examination revealed a firm mass filling the lower abdomen with restricted mobility upto 14-16 weeks size. Bimanual examination showed cervix hitched against pubic symphysis. Mass felt per abdomen through anterior and left adnexa was, not tender, uterus was about 8-10 weeks felt close to the mass, right adnexa free; P/R POD free, rectal mucosa free. Complete haemogram, renal function and urine analysis were normal and ultrasound of her abdomen and pelvis showed a 10cm x 9.8cm hypoechoic, well-defined left adenexal mass with cystic and calcified areas, likely broad ligament fibroid, bilateral ovaries were normal. Thus a provisional diagnosis of Broad ligament fibroid uterus was made and was decided that surgery - Myomectomy was the best choice. Peroperative findings: Uterus was 8-10 weeks was lifted up and close to lower end of uterus close to uterosacral ligament, mass about 10cmx12 cm of varying consistency, mostly hard was filling the pelvis was found, with cystic right ovary & left ovary was normal as seen in [Table/Fig-1].
Intraoperative picture showing the mass (arrow) close to uterus with bilateral ovaries.
After informed consent, decision to do abdominal hysterectomy was done since mass was close to uterus and uterus was enlarged. During abdominal hysterectomy when mobilizing the mass adherent to the uterus, necrotic yellowish material came out from the thick capsule like structure as seen in [Table/Fig-2]. Abdominal hysterectomy with right salpingoophorectomy was done. Rest of the tumour was enucleated intra lesion as in [Table/Fig-3]. During the procedure, there was tearing of external iliac vessel same was sutured by surgeon. Intraoperatively blood loss was heavy and 5units of blood and one FFP were given. Few remnant tumour densely adherent to deeper structures were left behind. Postoperative, right ureteric injury was suspected, ureteric stent was introduced and patient was discharged on 15th day. Histopathology of the tumour revealed Schwannoma undergoing cystic degenerative changes and osseous Metaplasia.
Retroperitoneal tumour with the Necrotic yellowish material. (arrow)

Tumour with uterus after surgical removal.

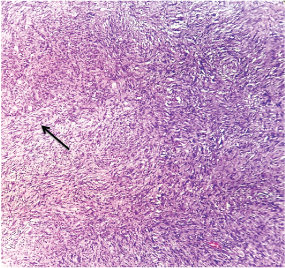
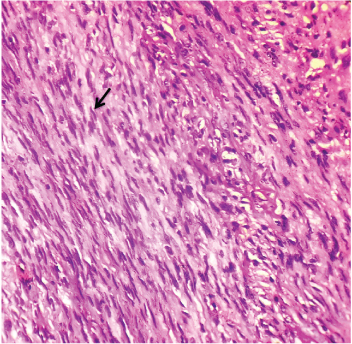
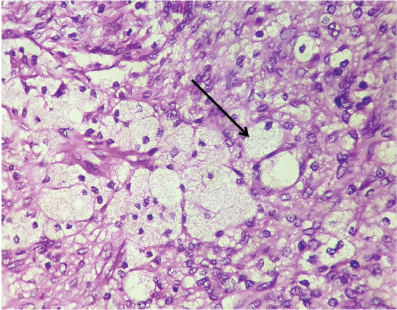
Grossly, there were multiple irregular, pale brown soft tissue masses, with rough external surface, all together measuring 15x10x6cm, smallest mass measured 0.8x0.5cm and largest mass measured 6x3x2cm. Cut surface was pale brown, firm homogenous with focal gray white glistening areas routine processing of the tissue was done, 4μm sections were taken, Haematoxylin and Eosin staining was performed. Microscopically, the tumour was highly cellular; ill circumscribed, composed of spindle-shaped cells variably arranged in intersecting long and short fascicles [Table/Fig-4]. Spindle cells had moderate amounts of eosinophilic cytoplasm and wavy nuclei [Table/Fig-5].
Microscopically, the tumour was highly cellular; ill circumscribed, composed of spindle-shaped cells variably arranged in intersecting long or short fascicles (40X).
Spindle cells had moderate amounts of eosinophilic cytoplasm and wavy nuclei (100X).
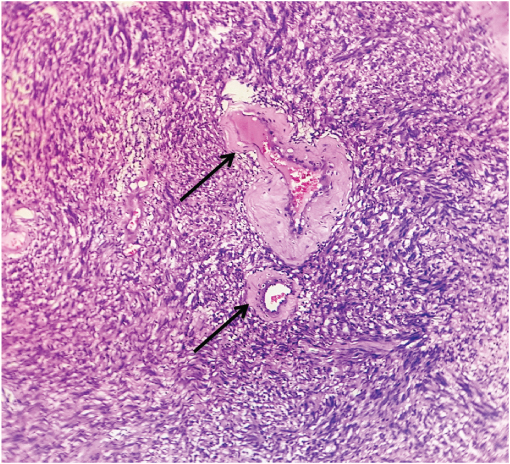
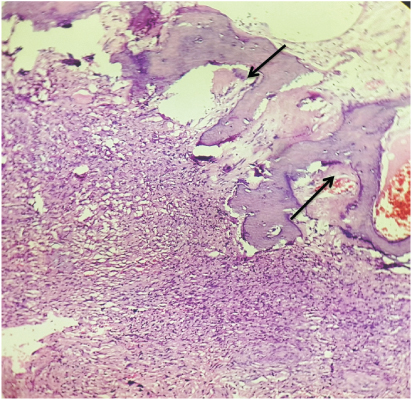
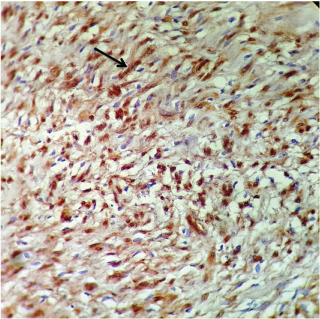
Focally, neoplastic cells exhibited storiform and herringbone growth patterns. The cells had relatively abundant pale to eosinophilic cytoplasm and oval nuclei. Mitotic activity was low (<2mitosis×10HPF). Nuclear pleomorphism and atypical mitoses were not seen. Tumour contained numerous small to medium sized blood vessels with thick hyalinized walls [Table/Fig-6]. Areas of degenerative changes characterized by oedema and abundant foamy histiocytes interspersed among fascicles of tumour cells were noted [Table/Fig-7]. Interestingly, a foci of bone formation composed of bony trabeculae enclosing marrow spaces, was seen [Table/Fig-8]. Immunohistochemical staining for S100 was performed with mouse antibody clone: 4C4.9 S100 (BIO SB). The spindle cells exhibited positivity for S100 [Table/Fig-9]. This case is reported for its rarity, and successful management of this case by multispecialty approach namely Gynaecologist, Surgeon, internal medicine specialist and Urologist.
Tumour contained numerous small to medium sized blood vessels with thick hyalinized walls (40X).
Areas of degenerative changes characterized by oedema, and abundant foamy histiocytes interspersed among fascicles of tumor cells were noted (100X).
Interestingly, a foci of bone formation composed of bony trabeculae enclosing marrow spaces, was seen (40X).
Immunohistochemistal staining for S100 was performed with mouse Antibody Clone: 4C4.9 S100 (Bio SB). The spindle cells exhibited positivity for S100 (100X).
Discussion
Schwannomas (neurilemmomas) are tumours of neurogenic origin arising from nerve sheaths. These tumors develop from a type of cell called a Schwann cell, which gives these tumors their name. Among all schwannomas pelvic occurrence is 1–3% and it is rare [1]. From the sacral nerve or the hypogastric plexus pelvic schwannomas arise [2]. These are usually slow growing tumours and are often detected incidentally. These tumours are usually solid but may undergo necrosis and cystic degeneration [3], usually seen in age groups of 20-50 years, more commonly in males than females [4]. The cause of schwannomas is unknown [5]. They sometimes occur in people with certain disorders including some types of neurofibromatosis (neurofibromatosis type 2 and schwannomatosis). NF is a dominantly inherited tumour prone disorder characterized by development of multiple schwannomas and meningiomas. The disease can be diagnosed when there is pathogenic mutation of NF2 gene [6].
They may arise de novo or may be associated with von Recklinghausen’s disease. If they are a part of von Recklinghausen’s disease there is always a chance to undergo malignant change, but these are most commonly benign. These are found rarely in the pelvis with very few cases, around 20, as reported in the English literature mentioned by Yi K et al., [7]. Present case was slow growing and schwannomas are slow-growing tumours and do not cause many symptoms until they have attained a large size as reported by Jindal et al., [8]. Schwannomas may cause non-specific symptoms such as backache, abdominal or pelvic heaviness, distension and discomfort (Jindal et al., [8]) and the present case had similar symptoms. In our case pelvic schwannoma must have originated from a sacral nerve or the hypogastric plexus similar to the case reported by Takashi Okuyama et al., [9].
In the present case it was misdiagnosed as Broad ligament fibroid same as in the report of Song JY [10] but in his report Schwannoma was misdiagnosed preoperatively in 60 year woman as a malignant adnexal mass. Preoperative diagnosis of pelvic schwannomas is difficult as there are no imaging findings that are specific for schwannomas. In our case USG reported as Broad ligament fibroid which is similar to the case report by Takashi Okuyama et al., in his case preoperative diagnosis was mesenteric tumour [9].
In our case tumour densely adherent to deeper structures was left behind to prevent injury as mentioned by Borghese M et al., [1].
As mentioned by Borghese M et al., schwannoma can be diagnosed only during surgery and definitive diagnosis by histological examination [1]. In our case though patient had few gynaecological symptoms, pelvic Schwannoma definitive diagnosis is done by HPE.
The prognosis of schwannoma after surgical excision is good though recurrence is less but our patient has to be followed up for recurrence since surgical removal is incomplete. Our case was ‘ancient schwannomas’ since it showed cystic degeneration and calcification [11] which was reported initially by Ackerman and Taylor. The differential diagnoses include psoas abscess, retroperitoneal lymph nodes, adnexal mass, fibrosarcoma, liposarcoma and ganglioneuroma. As mentioned by Andonian et al., it is always recommended to use Surgical excision and Histopathological examination to arrive at a confirmatory diagnosis since imaging findings are not specific. Also, percutaneous biopsies are often used which are inaccurate and sometimes misleading [3]. Patients with asymptomatic neurilemmomas occurring in association with NF2 frequently present with more severe neurologic deficits.
Conclusion
In all pelvic mass, one of the differential diagnosis of Pelvic schwannomas is to be thought off. A high index of clinical suspicion is required. Pre-operative imaging was not conclusive, in our case but preoperative and postoperative complications were promptly managed by multispecialty team work.
[1]. Borghese M, Corigliano N, Gabriele R, Antoniozzi A, Izzo L, Barbaro M, Benign schwannoma of pelvic retroperitoneum. Report of a case and review of the literatureG Chir 2002 21(5):232-38. [Google Scholar]
[2]. Aubert J, Debiais F, Irani J, Dore B, Levillain P, Schwannome. et appareil urinaire. A propos Dùne tumeur du nerf obturateur [in French]Prog Urol 1999 9:528-33. [Google Scholar]
[3]. Andonian S, Karakiewicz PI, Herr HW, Presacral cystic schwannoma in a manUrology 2003 62:551 [Google Scholar]
[4]. Wong CS, Chu TYC, Tam KF, Retroperitoneal schwannoma: A common tumour in an uncommon siteHong Kong Medical Journal 2010 16(1):66-68. [Google Scholar]
[5]. Roche PH, Bouvier C, Chinot O, Figarella-Branger D, Genesis and biology of vestibular schwannomasProg Neurol Surg 2008 21:24-31. [Google Scholar]
[6]. Evans DGR, Huson S, Donnai D, Neary W, Blair V, Newton V, A clinical study of type 2 neurofibromatosisQ J Med 1992 84:603-18. [Google Scholar]
[7]. Yi K, Wang YM, Chen J, Laparoscopic resection of an obturator schwannoma: a case reportChin Med J 2010 123:1804-06. [Google Scholar]
[8]. Jindal T, Mukherjee S, Kamal MR, Sharma RK, Ghosh N, Cystic schwannoma of the pelvisAnn R Coll Surg Engl 2013 95(1):e1-e2. [Google Scholar]
[9]. Okuyama T, Tagaya N, Saito K, Takahashi S, Shibusawa H, Laparoscopic resection of a retroperitoneal pelvic schwannomaJSCR 2014 1:1-4. [Google Scholar]
[10]. Song JY, Kim SY, Park EG, Kim CJ, Kim do G, Lee HK, Schwannoma in the retroperitoneumJ Obstet Gynaecol Res 2007 33(3):371-75. [Google Scholar]
[11]. Goh B, Tan Y, Chung Y, Chow PK, Ooi LL, Wong WK, Retroperitoneal schwannomaAm J Surg 2006 192:14-18. [Google Scholar]