Fibrofascitis – An Enigma for the Dentist: A Case Report
Kriti Shrivastava1, Giridhar Naidu2, Manas Gupta3, Neha Singh4
1 Senior Lecturer, Department of Oral Medicine and Radiology, Rishiraj College of Dental Sciences & Research Centre, Bhopal, Madhya Pradesh, India.
2 Reader, Oral Medicine and Radiology, Peoples Dental Academy, Bhopal, Madhya Pradesh, India.
3 Senior Lecturer, Department of Oral Medicine and Radiology, Rishiraj College of Dental Sciences & Research Centre, Bhopal, Madhya Pradesh, India.
4 Senior Lecturer, Department of Oral Medicine and Radiology, Rishiraj College of Dental Sciences & Research Centre, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kriti Shrivastava, Senior Lecturer, Department of Oral Medicine and Radiology, Rishiraj College of Dental Sciences & Research Centre, Bhopal, Madhya Pradesh-462026, India. E-mail- kriti_s2007@yahoo.co.in
Fibromyalgia is a chronic syndrome that causes widespread musculoskeletal pain and stiffness throughout the connective tissues that support and move the bones and joints. Pain and localized tender points occur in the muscles, particularly those that support the neck, spine, shoulders, and hips. Moreover the disorder includes fatigue, depression, sleep disturbances and constipation. A combination of treatments including medications, patient education, physical therapy and counseling are usually recommended. Here, we present a case report of fibromyalgia and the treatment given to the patient, a combination of dental and orthopedic treatment.
Fibromyalgia, Muscles, Musculoskeletal pain, Tender points
Case Report
An 18-year-old female patient reported to the Department of Oral Medicine and Radiology with the chief complaint of pain in right and left neck region and difficulty in mouth opening since one year. The patient was apparently alright one year back when she started feeling slight pain and discomfort on mouth opening. Gradually the pain developed in the right and left lower neck region. Pain was described as constant, dull and non-radiating, typically arising from the neck muscles and at times it was intense and burning in nature. There were no relieving or aggravating factors associated with pain. Patient appeared anxious and also gave a history of disturbed sleep. She was well coordinated with moderate built and all the vitals were within the normal range.
On extra-oral examination face appeared symmetrical [Table/Fig-1] with restricted mouth opening (3cm) and pain on turning head. On palpation tenderness was elicited with respect to left masseter, right and left sternocleidomastoid and trapezius muscles, bilateral clicking of Temporo Mandibular Joint (TMJ) during early mouth opening and tenderness over the cervical areas was noted. On intra-oral examination full complement of teeth were present, no odontogenic abnormality detected, class I occlusal relation with no occlusal discrepancies was observed. On palpation tenderness was noted bilaterally over lateral and medial pterygoids.
Extra-oral view showing no abnormality.

A provisional diagnosis of myofascial pain syndrome associated with cervical spondylosis was given and the following differential diagnosis were considered - impacted third molars, internal disc derangement in the TMJ, TMJ arthritis, otitis media / mastoiditis, eagle’s syndrome /ernest syndrome, fibromyalgia/ fibrofascitis.
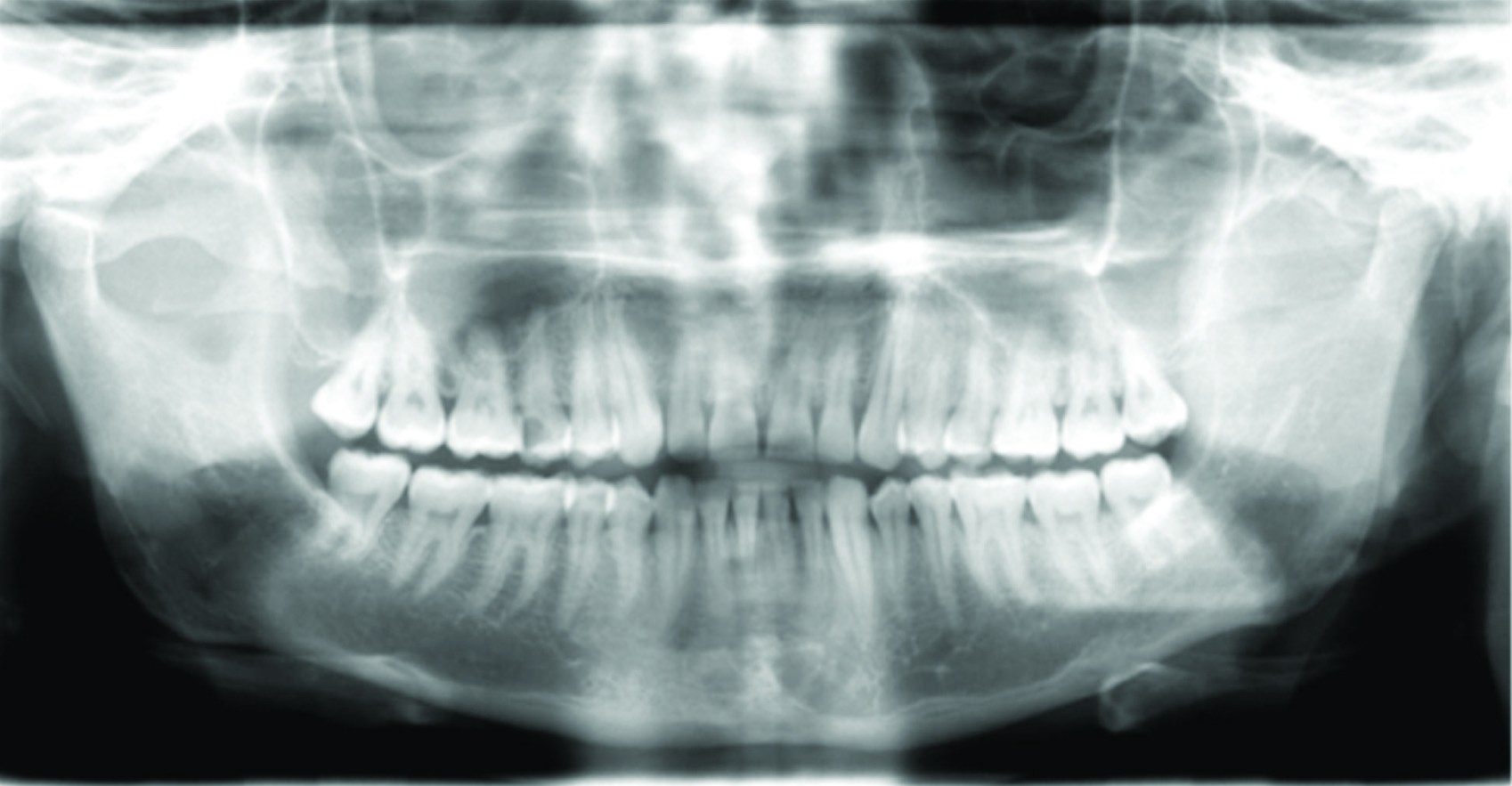
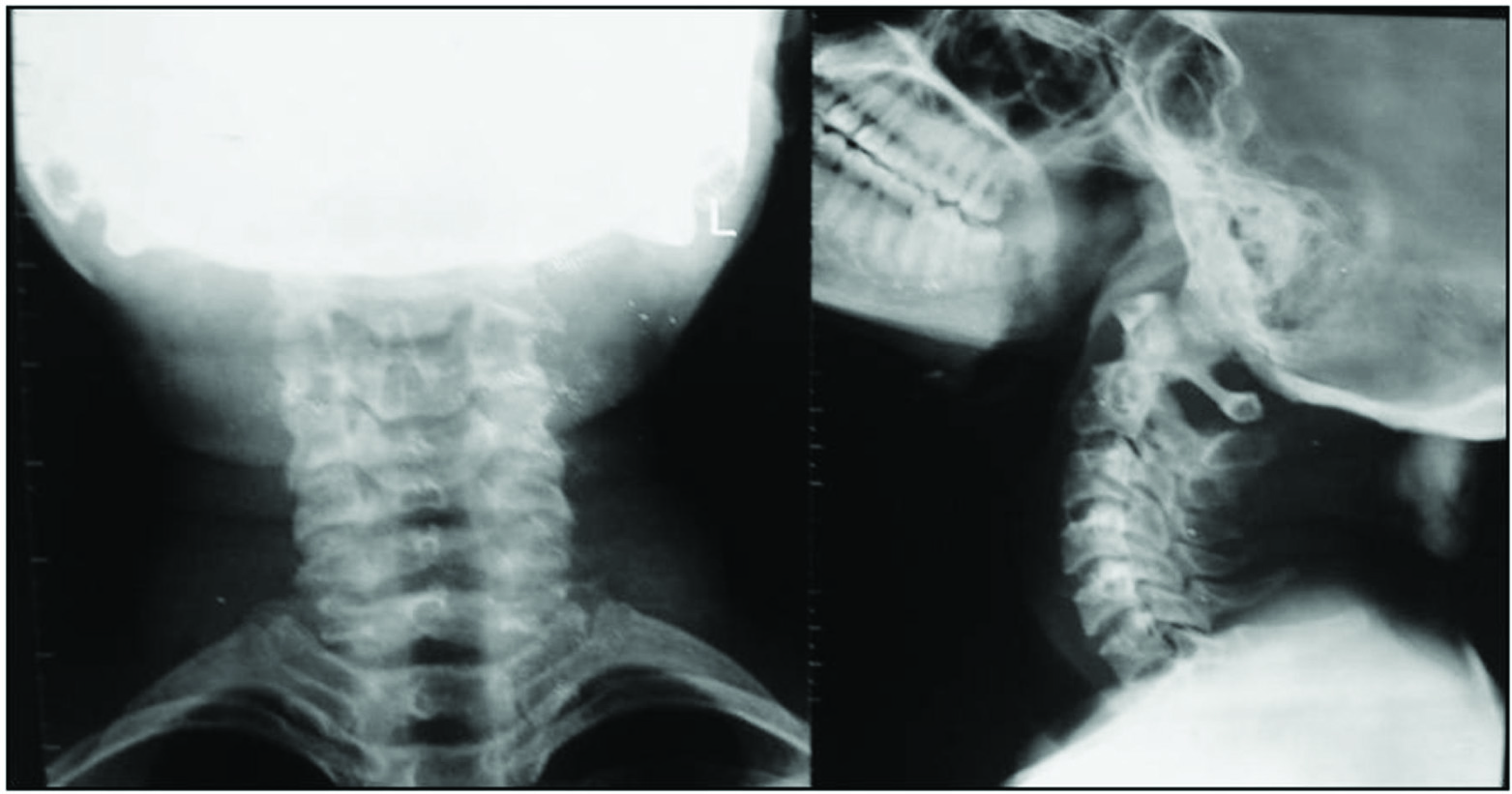
The investigations consisted of radiographs including Panoramic radiograph /OPG [Table/Fig-2], anterioposterior and lateral view of cervical vertebrae [Table/Fig-3] which did not reveal any significant changes. Blood investigations consisted of complete blood picture, C-reactive protein estimation, antistreptolysin O titre – all the parameters were within the normal range. Patient was also referred to Ear Nose Throat Department of People’s General Hospital for opinion where the specialist ruled out otitis media or mastoiditis.
Orthopantomograph(OPG) indicates no odontogenic abnormality.
Anterioposterior and lateral view of cervical vertebrae showing no abnormality.
Anterior repositioning device.

Our initial management consisted of-
Transcutaneous electrical nerve stimulation therapy along with non steroidal anti-inflammatory drugs, skeletal muscle relaxants and anti - anxiolytics for 1 week but the patient response was not satisfactory. To increase patient comfort physiotherapy was started and an anterior repositioning device for 15 days was also given. Patient had relief from pain in the maxillofacial region but neck pain still persisted.
Analysing the persistent pain areas in the neck region an orthopaedic consultation was sought and it was finally diagnosed as a case of FIBROFASCITIS associated with myofascial pain syndrome.
Patient was thus treated in conjunction with the orthopaedicians [Table/Fig-5].
Final management of the patient.
| DENTAL MANAGEMENT | ORTHOPEDIC MANAGEMENT |
|---|
| TENS Therapy | Physiotherapy – massage stretching exercises |
| Anterior repositioning device [Table/Fig-4] | IFT – Interferential Therapy |
| Muscle relaxants, anxiolytics, anti - depressants | Trigger point therapy |
| NSAID’S | Myofascial release |
| Patient Education – soft diet, hot fomentation, mouth opening and closing exercises | Massage |
Discussion
Fibromyalgia syndrome (FM)/Fibrofascitis is a chronic pain syndrome, characterized by generalized pain, tender points, disturbed sleep and pronounced fatigue felt in the musculature [1]. The aetiology of FM is unidentified, however abnormal concentrations of neuropeptides of CNS and alterations of the hypothalamic-pituitary-adrenal axis have been proposed as the causative factor [2]. In numerous studies the involvement of a gene has been indicated in the serotoninergic, dopaminergic, and catecholaminergic systems involved in FM [3]. In FM, allodynia is widespread and not just limited to tender points. Many studies on FM have shown abnormalities of pain sensitivity while using different methods of neurosensory testing [4].
FM is a symptom complex and there is no specific representative or distinguishing feature. The diagnosis is made clinically, with no laboratory or radiological tests available. However in 1990, the American College of Rheumatology (ACR) published diagnostic criteria for FM that included chronic widespread pain (>3 months) and mechanical allodynia in at least 11 of 18 tender points [5]. It occurs more commonly in women, in the ratio of 9:1 [6]. Using different methods to monitor blood flow in the muscles, the researchers concluded that there is a significantly reduced intramuscular perfusion of muscles in patients with fibromyalgia [7,8].
The clinical features consist of: (i) Structural Dysfunction; (ii) Pain increases with function of involved muscles; (iii) Generalized myogenous pain even at rest; (iv) Tender points throughout the various quadrants of the body [9].
Fibromyalgia is a complex condition hence can be difficult to treat. A combination of treatments including medications, patient education, physical therapy and counseling are usually recommended.
Pharmacological Treatment
Various drugs have been tried for the management of FM, these include selective serotonin reuptake inhibitors (SSRIs; fluoxetine) and dual serotonin-nor-epinephrine reuptake inhibitors (SNRIs; milnacipran, duloxetine) have demonstrated moderate effectiveness. Tramadol is the only analgesic shown to be helpful in FM treatment [10,11].
In 2007, the FDA approved Pregabalin as the first drug for the treatment of fibromyalgia [12]. A meta-analysis of the trials with Pregabalin and gabapentine also showed effects on reduction of pain, improved sleep, and quality of life [13].
Non-Pharmacological Treatment [
14]
Physical therapy – Several interventions undertaken suggest that cardiovascular aerobic exercise can be one of the most promising and effective treatments for FM. In addition, pool exercise, aerobic exercise including cycling, dance, and walking in-doors significantly improve FM pain and function.
Cognitive – Behavioural Therapy (CBT): Researches and interventions also indicate that psychological and behavioural therapy in the form of CBT is effective in managing FM pain.
Other treatments – There is some evidence to support the use of acupuncture.
Conclusion
FM is a chronic pain disorder and patients suffer with significant disability and reduced quality of life and may also develop secondary psychological disturbances, such as depression, anger, fear, and anxiety. The diagnosis of this condition as well as its management is a challenge for the physicians worldwide.
Accurate and most effective management of FM requires a multidisciplinary approach. In our patient, relief was achieved by combining the dental and the orthopedic management.
[1]. Staud R, New evidence for central sensitization in patients with fibromyalgiaCurr Rheumatoi Rep 2004 6:259 [Google Scholar]
[2]. Neeck G, Neuroendocrine and hormonal perturbations and relations to the serotonergic system in fibromyalgia patientsScand Rheumatol Suppl 2000 113:8-12. [Google Scholar]
[3]. Buskila D, Developments in the scientific and clinical understanding of fibromyalgiaArthritis Res Ther 2009 11:242 [Google Scholar]
[4]. Neeck G, Pathogenic mechanisms of fibromyalgiaAgeing Res Rev 2002 1:243-55. [Google Scholar]
[5]. Wolfe F, Smythe HA, Yunus MB, The American College of Rheumatology 1990 criteria for the classifi cation of fibromyalgia. Report of the Multicenter Criteria CommitteeArthritis Rheum 1990 33:160-72. [Google Scholar]
[6]. Burckhardt CS, Goldenberg D, Crofford L, Gerwin R, Gowans S, Jackson K, Guideline for the management of fibromyalgia syndrome pain in adults and children, APS Clinical Practice, Guideline Series No 4 2005 Glenview, ILAmerican Pain Society [Google Scholar]
[7]. Delgado EV, Romero JC, Escoda CG, Myofascial pain syndrome associated with trigger points: a literature review. (I): Epidemiology, clinical treatment and etiopathogenyMed Oral Pathol Oral Cir Bucal 2001 1(10):e494-98. [Google Scholar]
[8]. Bennett RM, Emerging concepts in the neurobiology of chronic pain: evidence of abnormal sensory processing in fi bromyalgiaMayo Clin Proc 1999 74:385-98. [Google Scholar]
[9]. Okeson JP, Management Of TMJ disorders And Occlusion 2008 6th edPhiladelphiaMosby Elsevier [Google Scholar]
[10]. Biasi G, Manca S, Manganelli S, Tramadol in the fi bromyalgia syndrome: a controlled clinical trial versus placeboInt J Clin Pharmacol Res 1998 18:13-19. [Google Scholar]
[11]. Goldenberg DL, Pharmacological treatment of fi bromyalgia and other chronic musculoskeletal painBest Pract Res Clin Rheumatol 2007 21:499-511. [Google Scholar]
[12]. Owen RT, Pregabalin: Its efficacy, safety and tolerability profile in fibromyalgia syndromeDrugs Today 2007 43:857-63. [Google Scholar]
[13]. Häuser W, Bernardy K, Üçeyler N, Sommer C, Treatment of fibromyalgia syndrome with gabapentin and pregabalin: a meta-analysis of randomized controlled trialsPain 2009 145:69-81. [Google Scholar]
[14]. Arnold LM, Biology and therapy of fibromyalgia. New therapies in fibromyalgiaArthritis Res Ther 2006 8:212 [Google Scholar]