Red Eye and Red Face Following Defibrilation
Pinar Doğan1, Sinan İnci2, Bihter Şentürk3, Fatih Mehmet Uçar4, Ümit Güray5
1 Faculty, Department of Cardiology, Aksaray State hospital, Aksaray-Turkey.
2 Faculty, Department of Cardiology, Aksaray State hospital, Aksaray-Turkey.
3 Faculty, Department of Cardiology, Yuksek Ihtisas Education and Research Hospital, Ankara, Turkey.
4 Faculty, Department of Cardiology, Yuksek Ihtisas Education and Research Hospital, Ankara, Turkey.
5 Faculty, Departmentof Cardiology, Yuksek Ihtisas Education and Research Hospital, Ankara, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sinan Inci, Aksaray State Hospital Zafer Mah, Nevsehir Cad No:117, Aksaray/Merkez, Turkey.
E-mail: doktorsinaninci@gmail.com
Electrocardiography, Facial petechial, Subconjunctival haemorrhage
Bilateral subconjunctival haemorrhage and facial petechia are common clinical finding, characteristically present in numerous disease especially systemic diseases; in the setting of infection or trauma; or in patients who are otherwise healthy. To our knowledge this feature has previously been described in one patient after cardioversion [1]. But in this case we wish to draw attention to this finding observed on a patient suffering defibrillation.
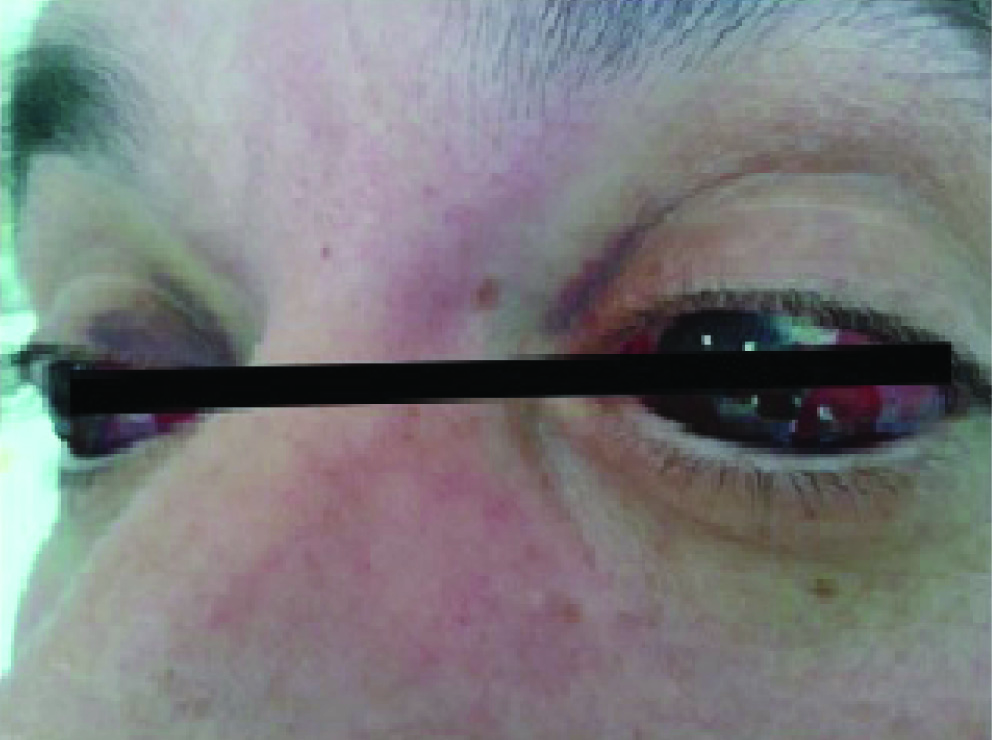
A 45-year-old man was admitted to our hospital with chest pain. His 12-lead electrocardiography (ECG) revealed acute inferior myocardial infarction and he was immediately transferred to catheterization laboratory. After coronary angiography, mid right coronary lesion was found to be culprit and percutaneous coronary intervention including coronary stent implantation was performed. A 7000 IU dose of IV heparin, 600 mg clopidogrel, 300 mg acetyl salicylic aside were given before coronary intervention. Ten hours later his symptoms recurred with associated electrocardiographic findings. Before re-transferring to cardiac catheterization laboratory, ventricular fibrillation occurred that was treated with 300 joule direct current defibrillation energy. Sinus rhythm was obtained. However, immediately after defibrillation, haemoptysis and nasal haemorrhage occurred. Also, within several hours after defibrillation multiple petechiae and a diffuse prominent edema on the face were noted [Table/Fig-1a&b]. Subconjunctival haemorrhage was also observed [Table/Fig-2]. At time of defibrillation platelet count, prothrombin time, and partial thromboplastin time were all within normal limits. There were no signs of associated coagulation disorders or capillary and platelet defects. Two-dimensional echocardiography has revealed acute right ventricular dilatation with moderate degree tricuspid regurgitation. Pulmonary artery systolic pressure was within normal limits which suggested right ventricular infarction. The rash started to fade spontaneously within 24 hours, and had disappeared completely after 4 days without treatment. Spontaneous regression of subconjunctival haemorrhage occurred in more prolonged time.
Diffuse prominent oedema and multiple petechiae.

Subconjunctival haemorrhage.
Rheumatological, dermatological, infectious, traumatic factors, local or systemic vascular diseases, bleeding disorders can cause facial petechiae and subconjunctival haemorrhage. Causes of subconjunctival haemorrhage are trauma, local acute inflammation of the conjunctiva, local or systemic vascular disorders or acute febrile systemic infections. None of the aforementioned pathological mechanisms was present in this case. Miscellaneous benign causes of facial petechiae and subconjuctiaval haemorrhage such as forceful coughing, vomiting, giving birth, after seizures, retch reflex triggered by endoscopy probe have also been reported in the literature [2–4]. Alcalay et al., suggested the name “mask phenomenon” to describe this condition [2]. The most likely explanation of this condition is a Valsalva maneuver that raised the intrathoracic or abdominal pressure and resulted in a rupture of the capillaries in the skin and in the territory of subconjuctiva. The most likely pathogenetic mechanism in this patient appears to be a sudden and severe rise of venous blood pressure due to raised intra-thoracic pressure in the already congested territory of the superior vena cava because of acute right ventricular failure.
[1]. Wackym PA, Ware JM, Gray GF, Subconjunctival haemorrhage, periorbital ecchymoses, and facial petechiae following cardioversionJ Tenn Med Assoc 1985 78:619-21. [Google Scholar]
[2]. Alcalay J, Ingber A, Sandbank M, Mask phenomenon: postemesis facial purpuraCutis 1986 38:28 [Google Scholar]
[3]. Rubegni P, Fimiani M, De Aloe G, Thoracocervico facial purpura as the single manifestation of epileptic seizureJ Neurol Neurosurg Psychiatry 1998 65:365 [Google Scholar]
[4]. Adısen E, Eroglu N, Oztas M, Gürer MA, A rare cause of facial purpura: endoscopyEndoscopy 2007 39(Suppl 1):E216 [Google Scholar]