Capillary Hemangioma of the Fallopian Tube
Richa Katiyar1, Shashikant C.U. Patne2, Shreekant Bharti3, Madhu Jain4
1 Service Senior Resident, Department of Pathology, IMS, BHU, Varanasi, U.P., India.
2 Assistant Professor, Department of Pathology, IMS, BHU, Varanasi, U.P., India.
3 Assistant Professor, Department of Pathology, IMS, BHU, Varanasi, U.P., India.
4 Professor and Head, Department of Obstetrics & Gynecology, IMS, BHU, Varanasi, U.P., India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shashikant C.U. Patne, Assistant Professor, Department of Pathology, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221005, U.P., India.
E-mail: Scup.pathology08@gmail.com
Neoplastic lesions of the fallopian tube are rarely seen by surgical pathologists. Haemangioma of the fallopian tube is an extremely rare benign neoplasm. A 30-year-old lady with polymenorrhea and dysmenorrhea underwent hysterectomy and bilateral salpingo-oophorectomy. Her left fallopian tube showed a 2mm sized solid nodule in the wall. Histopathological examination revealed a well-defined vascular lesion in the left fallopian tube, consistent with capillary haemangioma. The vascular endothelium was highlighted by CD34 immunostaining. Our literature review has identified 10 cases of cavernous haemangioma of the fallopian tube. To the best of our knowledge, we report the first ever case of capillary haemangioma of the fallopian tube. This is also the smallest detected haemangioma in the fallopian tube.
Female genital tract, CD 34, Vascular tumour
Case Report
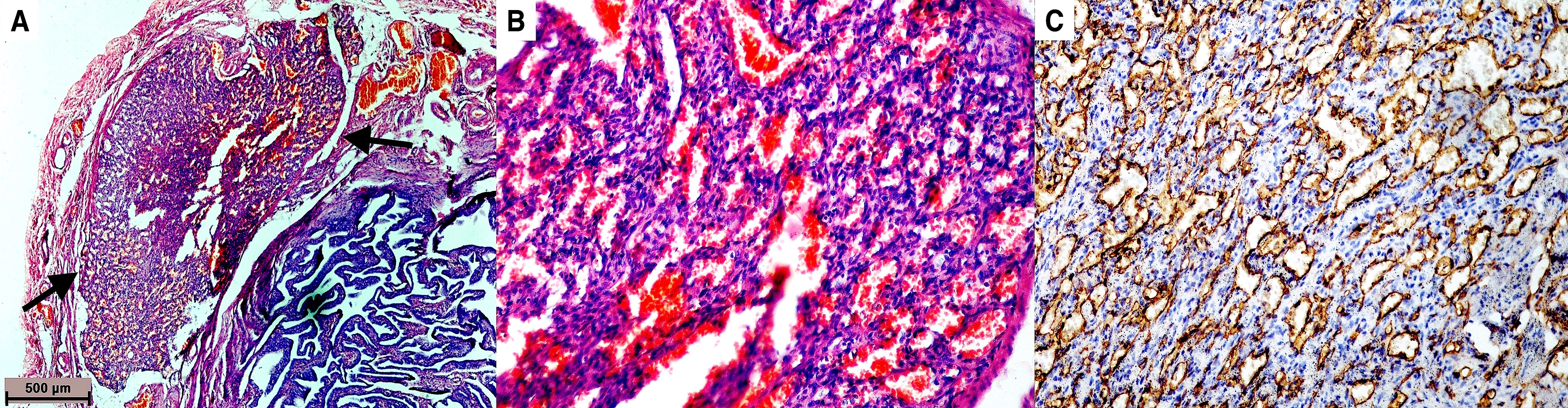
A 30-year-old lady complained of excessive and painful menstruation, which persisted for 8-10 days in each menstrual cycle. Her pre-operative investigations including haemogram (except haemoglobin 9.5 gram%), and serum creatinine were within the normal limits. Her tests for HIV, HBsAg and HCV were non-reactive. Her family was complete. She underwent hysterectomy with bilateral salpingo-oophorectomy. On gross examination, uterus and cervix measured 7×5×3.5 cm. Cut sections of the endometrial and the endocervical cavities were unremarkable. The endometrial thickness was 3mm. The right ovary measured 3.2×1.5×1.5 cm, which on cut showed two cysts of 0.5 cm diameter each, and both the cysts were filled with clear fluid. The right fallopian tube measured 2.5×0.5 cm with patent lumen and unremarkable wall. The left ovary measured 3×1.6×1.5 cm, cut surface showed a cyst of 0.5cm diameter, filled with clear fluid. The left fallopian tube measured 3×0.6 cm, cut surface revealed a 2 mm sized solid nodule in its wall and patent lumen. The nodule was sampled in entirety and could not be seen on subsequent cut sections. Haematoxylin and eosin- stained sections showed features of chronic cervicitis, proliferative endometrium, unremarkable myometrium and follicular cysts in the bilateral ovaries. Histology of the right fallopian tube was unremarkable. Histopathologically, wall of the left fallopian tube showed a well-defined vascular lesion [Table/Fig-1a], composed of proliferating thin walled capillary lumina lined by flattened mature endothelial cells that contains red blood cells [Table/Fig-1b]. Significant nuclear atypia, mitotic activity or necrosis was not seen in lining endothelial cells. There was no evidence of trophoblastic tissue. The endothelial lining was highlighted by CD34 immunostaining [Table/Fig-1c]. Finally, the lesion was diagnosed as capillary haemangioma of the left fallopian tube. Six-months after the surgery patient was doing well at the last follow-up.
a) Microphotograph showing a well-defined vascular tumour (arrows) in the wall of fallopian tube (Haematoxylin and eosin stain, 40×). b) Vascular tumour is composed of closely packed capillaries with luminal red cells and lined by flat endothelial cells (Haematoxylin and eosin stain, 200×). c) Immunostaining highlighting CD34 positive endothelial cells (Diaminobenzidine,100×).
Discussion
Non-neoplastic lesions are more common than neoplastic lesions in the fallopian tube [1]. Surgical pathologists frequently receive the fallopian tubes for examination, as these are prophylactically removed during surgeries of other gynaecological lesions [1]. Many benign tumours of the fallopian tube are too small to be detected. Mostly these are found incidentally during the pathological examinations. Haemangioma of the fallopian tube is an extremely rare benign tumour. Our literature review has revealed that only 10 cases of the fallopian tube haemangioma have been reported till date [2–11]. All these 10 reported cases are cavernous haemangioma of the fallopian tube. To the best of our knowledge, capillary haemangioma in the fallopian tube has not been reported in the published English literature.
We herein report capillary haemangioma- one of the extremely rare benign tumours of the fallopian tube. Because of rarity, clinical signs, symptoms and outcome of the fallopian tube haemangioma are infrequently reported. In the published literature, previous 10 reported cases of fallopian tube haemangiomas have occurred in patients aged 13-77 years [8,9]. The fallopian tube haemangiomas are usually small tumours ranging from 5 mm to 30 mm in size [9,11]. In comparison to previous cases, 2 mm-sized haemangioma of our case is the smallest detected haemangioma in the wall of fallopian tube. Small size of haemangioma does not cause any morbidity unless it grows in size or lead to haemorrhagic manifestations. Likewise, most of the fallopian tube haemangiomas have been incidentally identified in the left fallopian tube [11]. However, in contrast, three cases of cavernous haemangiomas have presented with acute abdomen due to haemoperitoneum [5,7,8]. Histologically, cavernous haemangiomas are composed of irregularly dilated thick-walled vascular spaces lined by endothelium, whereas capillary haemangiomas consists of proliferating endothelial cells resulting in formation of lumina with single-layer of endothelial lining and red blood cells [9]. Histological differential diagnosis of the fallopian tube haemangioma includes - lymphangioma, vascular leiomyoma, mesothelioma, and adenomatoid tumour [9]. Although there is no problem in differentiating haemangiomas from these entities, immunohistochemistry may be used for confirmation. Immunohistochemically, haemangiomas are positive for CD31, CD34 and smooth muscle actin (SMA). Lymphangiomas show positivity for LYVE-1. Both adenomatoid tumour and mesothelioma exhibit positivity for mesothelial markers- calretinin, D2-40 and WT-1 protein. Vascular leiomyoma will be positive for SMA, desmin and caldesmon [12]. We have seen characteristic histology of capillary haemangioma and confirmed the same by CD34 immunostaining. Treatment of the fallopian tube haemangioma is surgical excision. Recurrence has not been reported in any of the previous 10 cases. Follow-up may be done to look for vascular lesions at other sites in rare cases of congenital vascular malformation.
Conclusion
To conclude, we are for the first time reporting an incidentally detected capillary haemangioma of the fallopian tube. This is also the smallest detected haemangioma of the fallopian tube. Surgical pathologists should be watchful while sampling and examining the fallopian tube so that smallest of the lesions are not missed.
[1]. Vang R, Wheeler JE, Diseases of the fallopian tube and paratubal region. In:Kurman RJ, Ellenson LH, Ronnett BM, edsBlaustein’s pathology of the female genital tract 2011 6th editionNew YorkSpringer Science +Business Media [Google Scholar]
[2]. Ragins AB, Crane RD, Cavernous haemangioma of the fallopian tubeAm J Obstet Gynaecol 1947 54:883-86. [Google Scholar]
[3]. Gusmano G, Angioma of the Fallopian tubes; anatomopathological contributionMinerva Ginecol 1951 3:616-20. [Google Scholar]
[4]. Talerman A, Haemangioma of the fallopian tubeJ Obstet Gynaecol Br Commonw 1969 76:559-60. [Google Scholar]
[5]. Patel DR, Kawalek R, Iger J, Cavernous haemangioma of the fallopian tubeInternational Surgery 1972 58:420-21. [Google Scholar]
[6]. Ebrahimi T, Okagaki T, Haemangioma of the fallopian tubeAm J Obstet Gynaecol 1973 115:864-65. [Google Scholar]
[7]. Joglekar VM, Haemangioma of the fallopian tubeBr J Obstet Gynaecol 1979 86:823-25. [Google Scholar]
[8]. Gowri R, Soundararaghavan S, Oumachigui A, Iyengar KR, Fallopian tube haemangiomaJ Obstet Gynaecol Ind 2004 54:85-86. [Google Scholar]
[9]. Wojnar A, Drożdż K, Dzięgiel P, Cavernous haemangioma of the oviductPol J Pathol 2010 61:103-04. [Google Scholar]
[10]. Atere-Roberts N, Angelopoulos L, Ghataura S, Vijayanand R, Cavernous haemangioma of the fallopian tube presenting as appendicitis in an adolescent girlJ Obstet Gynaecol 2010 30:70-71. [Google Scholar]
[11]. Deb P, Singh V, Dutta V, Kapoor K, An unusual case of cavernous haemangioma of the Fallopian tubeJ Can Res Ther 2014 10:363-64. [Google Scholar]
[12]. Mills SE, Greenson J, Hornick JL, Longacre TA, Reuter VE, Sternberg’s diagnostic surgical pathology 2015 6th editionWolters Kluwer Health [Google Scholar]