The meniscus is a biconcave fibrocartilage in the knee joint interpose between the femoral condyles and tibial plateau [1]; the meniscus has functions in load bearing, load transmission, shock absorption joint stability, joint lubrication and joint congruity [1–3]. There are generally two common types of meniscal tears seen in clinical practice: Traumatic tears and Degenerative tears. Meniscal pathology in younger patients is likely to be consequent to an acute traumatic event, while degenerative changes are more frequent at an older age [4]. The diagnose of a meniscal tear is generally based on the analysis of clinical history, physical examination, magnetic resonance imaging (MRI) studies and gross morphology of the meniscus under arthroscopic findings [5,6]. Patients with traumatic tears usually give a history of a twisting, pivoting or hyper flexion mechanism of the knee, while patients with degenerative tears mostly give the history of insidious joint line pain, give away, locking and catching sensation in the absence of trauma or a known event, and in some cases patient may first notice symptoms only with high demand activities [5]. Using magnetic resonance imaging, meniscal tears are present in approximately 20% of people without knee symptoms [7]. Selecting the correct treatment can be challenging and involves multiple factors. Today treatment options for meniscal tears fall into three broad categories; conservative, meniscectomy or meniscal repair [8,9].
The aim of the present study is to determine whether there is a difference in terms of clinical outcome between traumatic and degenerative meniscal tears between 1 and 4 years after arthroscopic meniscus surgery.
Materials and Methods
Data Collection: The study protocol was approved by the institutional ethics committee of the tertiary care center. Consecutive hospitalized patients with meniscus injury treated with arthroscopic surgery at the tertiary care center by the same group of surgeons from January 2010 to June 2013 were included in the present study. Patients’ data were retrospectively collected from June to August 2014. Clinical information and follow-up data were obtained from their medical records, by telephone calls and at subsequent visits. The Lysholm score was used to evaluate the performance and patient’s activity restriction and the RAND 36-short form health survey (SF-36) was used to evaluate patient’s life quality after the surgery.
Inclusion and Exclusion Criteria: Inclusion criteria for the study group were patients who: 1) were diagnosed with a meniscal tear under MRI and arthroscopic findings; 2) underwent arthroscopic meniscus surgery performed by the same group of surgeons at the Orthopedic department of Southeast University affiliated Hospital; and 3) were followed up for at least one year. Exclusion criteria was as follow: 1) patients older than 75-year-old; 2) suffering from a co-existing knee condition such as ACL/PCL injury, knee instability; 3) patients with BMI≥30, according to the Chinese criteria of weight WS/T 428-2013; 4) suffering from a major condition influencing his/her life quality such as advanced coronary heart disease, sequels from previous surgery, advanced Osteoarthritis; 5) follow-up loss.
Study design: Patients who satisfied the criteria of inclusion were divided into two groups, traumatic group (T group) and non-traumatic group (NT group), according to the presence of previous known trauma history. Clinical data were collected from their medical records including patients name, sex, age, weight, high, medical history, diagnoses, surgery date and procedure. Assessments were made by telephone calls and at subsequent visits. Two subgroups were created in each T and NT group according to the patients follow up duration, respectively at a mean follow up of 1year±3 months (1 year group) and 4years±3 months (4 years group) after surgery. Clinical outcome were assessed using the lysholm scale and the RAND SF-36 health survey.
Assessment: The Lysholm scale [10] is a well validated functional score designed for knee injuries. A questionnaire where each possible response to each of the 8 items has been assigned an arbitrary score on an increasing scale. The total score is the sum of each response to the 8 items. A score of 100 means no symptoms or disability. (95–100) is Excellent, (84–94) is Good,(65–83) is Fair and (<65) is Poor.
The SF-36 health survey questionnaire [11] is exclusively used to assess health-related quality of life. The 36 questions questionnaire is subdivided in eight domains assessing the physical and social status of the patient: 1) physical functioning, PF; 2) role limitations due to physical health, RP; 3) role limitations due to emotional problems, RE; 4) energy/fatigue, VT; 5) emotional well-being, MH; 6)social functioning, SF; 7) body pain, BP; and 8) general health, GH. The questions are scored on a scale of 0 (worst health) to 100 (ideal health).
Statistical Analysis
All data were registered in a Microsoft Excel database, and analysis was performed by SPSS for Windows version 17.0. T-test, Chi-square test were used for comparisons. Statistical significance was accepted at p<0.05.
Results
One hundred and seventeen patients were included in the present study with 60 patients in the traumatic group and 57 patients in the degenerative (non-traumatic) group. Patients demographics at follow up are presented in [Table/Fig-1] where it shows that 70 (59.82%) patients in total suffered of an injury of the posterior horn of the meniscus, with 43 (75, 43%) in the non-traumatic (degenerative) group compare to 27 (45%) in the traumatic group. No significant differences were found for patient’s sex, BMI and Ages between both groups. We loss follow up of 11 traumatic and 9 non-traumatic participants mostly due to loss of contacts. Two patients were excluded from the degenerative group after undergoing TKA during follow up.
| Item | T | NT | p-value |
|---|
| Number of patients | 60 | 57 | |
| Subgroups |
| 1year | 22 | 21 | |
| 4year | 18 | 19 | |
| Sex | .573 |
| M | 22 | 26 | |
| F | 38 | 31 | |
| Age | .867 |
| Mean±SD | 44.8y±9.70 | 48.58y±8.25 | |
| Range | 18y-67y | 21y-72y | |
| BMI | .691 |
| Mean±SD | 24.62±3.24 | 24.88±3.73 | |
| Overweight | 20 | 21 | |
| Posterior horn | 27 | 43 | |
| Other parts | 33 | 14 | |
| Follow up loss | 11 | 9 | |
In [Table/Fig-2] we compared Lysholm scores in both groups between 1 and 4 years after arthroscopic surgery. There were no significant differences between both groups at 1 year follow up (p=0.7726), but the difference was quit significant at 4 years follow up(p<0.0001). Also, there was a significant improvement between 1 and 4 years follow up in the traumatic group, while no significant difference was noticed in the non-traumatic (degenerative) group.
Mean values of Lysholm scores in the subgroups.
| Groups | Lysholm | p-value |
|---|
| 1year | 4years |
|---|
| T | 85.25±8.78 | 92.63±7.31 | 0.0306 |
| NT | 86.38±12.14 | 72.90±20.77 | 0.0606 |
| p-value | 0.7726 | < 0.0001 | |
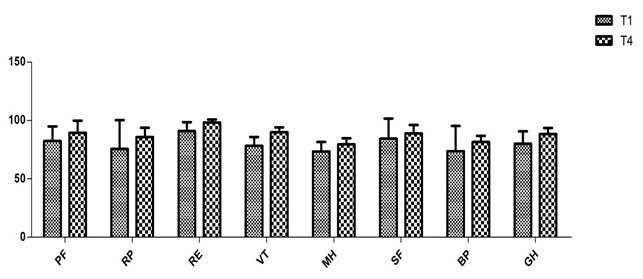
We also assessed patient’s quality of life using the Rand SF-36 health survey and results are presented in the following graphics.
A total of 95(81.19%) patients in total were satisfied with their health status at follow up. [Table/Fig-3] compares Rand SF-36 survey results in the traumatic group between 1 year and 4 years after arthroscopic surgery and [Table/Fig-4] compares Rand SF-36 survey results in the degenerative group between 1 year and 4 years follow-up.
T group SF-36 between 1 and 4 years follow up.
PF physical functioning, RP role limitations due to physical health, RE role limitations due to emotional problems, VT energy/fatigue, MH emotional well-being, SF social functioning, BP body pain, GH general health.
NT group SF-36 between 1 and 4 years follow up.
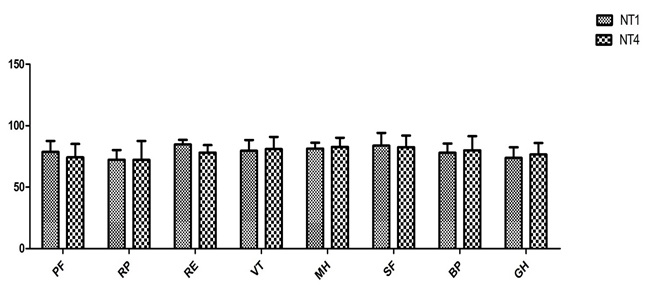
T-test was used for statistical examinations in all domains of the survey. T test results for T group are shown in [Table/Fig-5] and for NT group are shown in [Table/Fig-6].
T group SF-36 survey’s t-test results.
| domains | PF | RP | RE | VT | MH | SF | BP | GH |
|---|
| t | 24.12 | 15.85 | 24.87 | 14.32 | 24.97 | 37.10 | 19.81 | 19.48 |
| df | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p | 0.0264 | 0.0401 | 0.0256 | 0.0444 | 0.0255 | 0.0172 | 0.0321 | 0.0327 |
NT group SF-36 survey’s t-test results.
| domains | PF | RP | RE | VT | MH | SF | BP | GH |
|---|
| t | 10.91 | 5.912 | 5.570 | 104.2 | 25.32 | 7.218 | 5.368 | 9.114 |
| df | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p | 0.0582 | 0.1067 | 0.1131 | 0.0061 | 0.0251 | 0.0876 | 0.1173 | 0.0696 |
Results from [Table/Fig-3,5] shows that there was a significant improvement in all domains of the SF-36 health survey between 1 and 4 years follow up for the traumatic group (p<0.05 in all domains).
According to [Table/Fig-4,6], significance was reported only for VT and MH (p<0.05). There was no significant differences in other domains of SF-36 health survey between 1 and 4 years follow up for the non-traumatic group (p>0.05).
Discussion
The meniscus is vital to normal function and longevity of the knee, as meniscal loss causes increased contact pressures and articular cartilage degeneration [12,13]. Arthroscopic meniscus surgery is a high-volume surgery in many countries around the world, reason why it’s necessary to study the effect and burden of such a treatment. Meniscal repair and partial meniscectomy procedures are the standard therapies for meniscal treatment, however physical therapy have proven to be an efficacious course of management for some cases of meniscal tears [5,8,14]. Knowledge about the potential difference of the effect of arthroscopic meniscus surgery on patient symptoms between patients with traumatic and degenerative tear is sparse [15].
The most important finding of the present study was that compared to patients with degenerative (non-traumatic) meniscal tear, patients with traumatic meniscal tear had better improvements in terms of clinical outcome 4 years after arthroscopic surgery, this implies that arthroscopic surgery have a better mid-term clinical outcome as a treatment for traumatic meniscal tear compare to non-traumatic or degenerative meniscal tear. A similar conclusion was reported by Camanho et al., after monitoring 435 patients with isolated meniscal injuries for 4 years, the study demonstrated that arthroscopic meniscectomy for the treatment of traumatic meniscal injury gives better results than arthroscopic meniscectomy for the treatment of degenerative meniscal injury [16]. The only difference between Camanho’s report and the present study is that Camanho focuses his study on one specific type of arthroscopic meniscus surgery, which is menisectomy, while in our study patients underwent meniscectomy, meniscal repair or combined menisectomy and repair; therefore it becomes necessary to find out if the type of surgery could have an influence on the outcome. A comprehensive review of the literature will make understand that based on type of arthroscopic meniscus surgery, no differences have ever been reported at a short or mid-term follow up. Stein et al., reported that mid-term examinations showed no significant differences between meniscal repair and mesicectomy regarding osteoarthritis progress, no loss of sports activity, and no deficit of knee function for traumatic meniscal tears [17]. All the papers reporting a different outcome for meniscus surgery based on the type of surgery, repair or meniscectomy, are all long-term follow up studies [18].
We explain the relatively worst results found in the degenerative group is linked to the fact that knee Osteoarthritis (chondral damage) development is more important in this group of patients. A recent study from Thorlund et al., also implies that arthroscopy for degenerative knee provide small inconsequential benefit and is limited in time [19], this explains why in our study there was no significant improvement between 1 year and 4 years. Another recent study from Moin Khan et al., even recommends non-operative management as a first line treatment for degenerative meniscal tear in middle age patients [20].
During the present study we also found that 70(59.82%) patients in total suffered of an injury of the posterior horn of the meniscus with 43(75, 43%) in the non-traumatic (degenerative) group compare to 27(45%) in the traumatic group. The posterior horn of the meniscus is considered essential for maintaining hoop tension and preventing meniscal extrusion during axial loading because of it strong attachment to the central tibial plateau [21]. Recently, there have been several studies on medial meniscus posterior horn tears and it has been demonstrated that it’s very frequent in the Asian population and most medial meniscus posterior horn tears are reported as being degenerative in nature in older patients [22,23].
In the present study patients’ sex, age, BMI were not significant in the study subgroups. The influences of age and BMI on the long-term outcome of arthroscopic surgery have been demonstrated by many studies in the literature [24], but in this case we assessed short and mid-term outcome after arthroscopic surgery. Another reason why age and BMI were not significant might be the age and BMI limit set for inclusion in the present study.
Limitation
The main limitation of our present study was that both groups traumatic and non-traumatic were separated essentially based on the existence of a previous known trauma history to the knee, however all trauma history were not holder than six months prior surgery, many studies in the literature have used this approach to separate traumatic and degenerative meniscal tears [16,25]. Another limitation was the low numbers of patients in the subgroups.
Conclusion
In conclusion, 95(81.19%) patients in total were satisfied with their health status at follow up, however, we found that Arthroscopy as a treatment for meniscal tear have a relatively better mid-term clinical outcome for traumatic meniscal tears than for non-traumatic/degenerative meniscal tears.