Sebaceous Gland Carcinoma of Eyelid- A Tarnished Masquerade
Bijnya Birajita Panda1, Sucheta Parija2, Susanta Pujahari3, Jyotiranjan Mallick4
1 Senior Resident, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
2 Assistant Professor, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
3 Senior Resident, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
4 Senior Resident, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bijnya Birajita Panda, Senior Resident, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
E-mail: bigyan_panda@yahoo.co.in
Malignant tumours of the face are usually seen in the periocular region, mainly on eyelids most commonly in the inferior eyelid, medial canthus and superior eyelid, respectively. The prime treatment for eyelid malignant tumours is the total excision of the lesion with frozen section control or by Mohs Micrographic surgery. The postoperative defects should be reconstructed judicially taking care that the near normal anatomical and functional recovery is achieved. The Cutler-Beard flap procedure, a good alternative in the reconstruction of superior near-total eyelid defects resulted in good restoration of anatomy and function in our patient. We report a case of an eyelid growth persisting for 2 year duration mimicking a chalazion. Clinically the eyelid mass had malignant features and hence was planned for wide excision with frozen section of margins. After confirming the tumour free margins, we performed reconstruction of the eyelid defect with Cutler Beard flap procedure. She was followed up for one year which showed no local recurrence or regional/distant metastases.
Chalazion, Cutler-Beard flap, Frozen section, Lid reconstruction, Metastases
Case Report
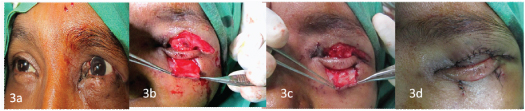
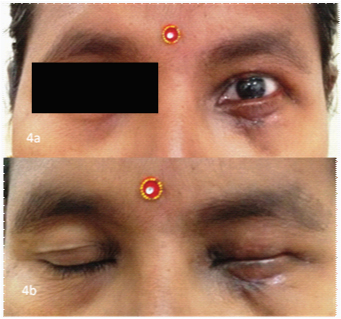
A 50-year-old woman, a homemaker, presented with a slowly growing nodular mass in her left upper eyelid for the last 2 years which had lately rapidly increasing in size for one month duration. On examination, the mass was 40x30mm [Table/Fig-1a] hard, rubbery in consistency, yellow in colour and tethering to the tarsal plate (seen on everting the eyelid) [Table/Fig-1b]. There were sparse eyelashes in the upper eyelid. Rest ocular examination revealed within references ranges except for early cataractous changes. Clinically, it resembled a nodular variety of meibomian gland carcinoma. She gave history of some past ocular surgery 1 year back of which no documents were available. She was not a known diabetic. She gave no history of anorexia/weight loss, drug allergy, and no exposure to radiation etc. General physical examination was within reference ranges. There was no regional or distant lymphadenopathy. Metastatic work up was negative. Her chest X-Ray, USG Abdomen and pelvis, liver function tests, renal function tests were within normal limits. Our patient was classified as stage T3aN0M0 according to AJCC (American Joint Commission on Cancer) [1]. After taking consent from the patient, we planned to go ahead with the surgical procedure. A wide margin (5mm) excision was performed and sent for frozen section histology. The frozen section technique [2] was completed intraoperatively, pagetoid spread was confined to a small portion of the lesion which was subsequently excised and after confirmation of tumour free margins, eyelid reconstruction was planned. The histopathology showed zones of necrosis, marked nuclear atypia, and abnormal mitotic figures, and an infiltrative growth pattern [Table/Fig-2]. However, immunohistochemistry was not done in our patient. A Cutler-Beard procedure was planned [Table/Fig-3]. Stage 1 was accomplished after creating a lower eyelid flap with a horizontal incision and advancing to the superior eyelid below the eyelash margin by separating the anterior and posterior lamellae. The anterior and posterior lamellae were sutured separately to the levator muscle and the orbicularis oculi muscle by placing the flap on the area of defect. Local dressing of the wound was done regularly for six weeks with frequent follow-ups (every 2 weeks till six weeks) for keeping surveillance for graft failure. The patient returned to us after six weeks and stage 2 was planned. The graft was in situ with good vascularity. The bridge flap was cut and conjunctiva sutured to reconstructed upper eyelid. The lower eyelid wound margins were freshened, underlying tissues and skin sutured to the surrounding tissue. Postoperatively after one week, there was no lag ophthalmos or exposure keratitis, and no residual periocular malpositioning [Table/Fig-4]. She was regularly followed up for one year to look for loco-regional metastases and her metastatic work-up was found to be negative.
(a) External photograph of the left upper eyelid mass; (b) measuring 40x30mm, hard, rubbery in consistency, yellow in colour and tethering to the tarsal plate on eyelid eversion

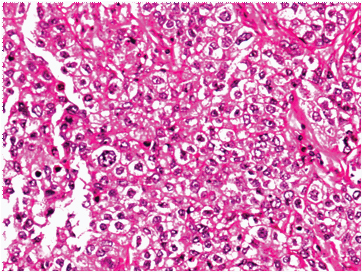
Histopathology under 10 X magnification showing zones of necrosis, marked nuclear atypia, and abnormal mitotic figures, and an infiltrative growth pattern.
(a) Intraoperative photograph showing > 75% upper eyelid defect after wide excision of the mass, (b) Cutler beard lid sharing procedure after suturing of innermost conjunctiva, (c) middle muscular layer; and (d) outer skin layer
Postoperative External photograph showing good functional and cosmetic recovery after Cutler beard stage 2 procedure: (a) with eyelids open showing good eyelid contour, (b) showing good eyelid closure.
Discussion
Sebaceous carcinoma is a highly malignant neoplasm of eyelids arising from meibomian glands and glands of Zeis and less commonly from sebaceous glands of caruncle and eyebrow. It is a rare and potentially aggressive cutaneous tumour with high recurrence rate, a substantial potential for metastases and significant mortality rate. Although it is relatively rare, it is the fourth most common neoplasms of the eyelid [3,4]. It metastasizes through lymphatic spread to regional lymph nodes [5]. It affects all races (mostly Asian and South-Asian races), women more than men and usually presents in sixth to seventh decades [6]. Associated risk factors include prior irradiation, and with production of nitrosamines and photosensitization from previous use of diuretics. Clinically, the tumour is a firm or rubbery, yellowish nodule adherent to the tarsus and adjacent tissues, size varies from 2-10 mm, resembling a chalazion. The tumour most commonly affects the upper eyelid, and to a lesser extent the lower eyelid or both eyelids [7].
Our case was a middle aged female of Indian origin without previous history of irradiation or any genetic predisposition who presented with a tumour of size 40x 30mm that resembled a giant chalazion but on eversion of the upper eyelid we could see involvement of the tarsus and surrounding tissues with yellowish multiple nodules. The patient came to us only when the mass showed aggressive increase in size and hence this delay in presentation predisposed for bad prognosis.
Histopathogically, it was composed of lobules of large hyperchromatic neoplastic cells with vacuolated, basophilic cytoplasm suggestive of sebaceous gland carcinoma. Histologically, it may resemble the appearance of squamous cell carcinoma but the difference lies in the type of cytoplasmic content which is basophilic in sebaceous gland carcinoma whereas eosinophilic in squamous cell carcinoma. Typically, four histological patterns have been described: lobular, comedocarcinoma, papillary and mixed. Special stains for lipid (oil red-O) on fresh tissue may help in further confirmation of diagnosis [8–10]. Rao et al., have described four histological patterns with poor prognosis: multicentric origin of the tumour, moderate to low sebaceous differentiation, infiltration and pagetoid invasion [11].
A comprehensive history and physical exam is a must in any case of eyelid mass. Baseline metastatic work-up should also be performed in these patients to rule-out metastatic disease. Standard treatment involves wide local excision with at least 4mm clear margins under frozen section control or Mohs Micrographic surgery. Once the tumour margins are clear, reconstruction can be done by variety of flap procedures. However, conjunctival map biopsies are recommended before start of the surgery as there is always a chance of intraepithelial pagetoid spread. If the tumour is very large or recurrent, or if there is pagetoid spread, or if it has spread to other eyelid or to orbital tissues, a subtotal or complete exenteration may be required or more tissue sparing alternatives such as cryotherapy or topical chemotherapy with Mitomycin C may be tried. In our case however there was very early pagetoid invasion which could be excised completely. If there is any evidence of spread to regional lymph nodes, the patient should be referred to a head and neck surgeon for possible lymph node or radical neck dissection. Radiation therapy can be considered as an adjunct treatment to local surgery since primary radiarion therapy is associated with high chance of recurrence [12]. However, few published studies have shown good results with primary radiation therapy due to improved irradiation techniques and newer technology [13–15].
Our patient was classified as stage T3aN0M0 and had a favourable clinical course. She showed no recurrence or metastasis to the regional lymph nodes or distant metastases even after one year following surgery.
Conclusion
Sebaceous carcinoma is not a very uncommon, aggressive tumour of the eyelids that mimics many inflammatory and neoplastic lesions. Precise diagnosis followed by apt management with a multimodal approach should be undertaken to achieve good tumour control and reduce the morbidity and mortality in these patients.
[1]. Edge SB, Byrd DR, Compton CC, AJCC Cancer Staging Manual 2009 7New YorkSpringer:523-30.Carcinoma of the eyelid; [Google Scholar]
[2]. Wilson LB, A method for the rapid preparation of fresh tissues for the microscopeJ Am Med Assoc 1905 45:1737 [Google Scholar]
[3]. Johnson S, Nerad JA, Syed NA. Sebaceous Cell Carcinoma: A Masquerade Syndrome. EyeRounds.org. January 23, 2007; Available from: http://webeye.ophth.uiowa.edu/eyeforum/62-Sebaceous-Cell-Carcinoma-A-Masquerade-Syndrome [Google Scholar]
[4]. Shields JA, Demirci H, Marr BP, Sebaceous carcinoma of the ocular region: a reviewSurv Ophthalmol 2005 50:103-22. [Google Scholar]
[5]. Nelson BR, Hamlet KR, Gillard M, Sebaceous carcinomaJ Am Acad Dermatol 1995 33:1-15. [Google Scholar]
[6]. Bailet JW, Zimmerman MC, Arnstein DP, Wollman JS, Mickel RA, Sebaceous carcinoma of the head and neck. Case report and literature reviewArch Otolaryngol Head Neck Surg 1992 118:1245-49. [Google Scholar]
[7]. Chao AN, Shields CL, Krema H, Outcome of patients with periocular sebaceous gland carcinoma with and without conjunctival intraepithelial invasionOphthalmology 2001 108:1877-83. [Google Scholar]
[8]. Ni C, Guo BK, Pathologic classification of meibomian gland carcinomas of eyelids: clinical and pathologic study of 156 casesChin Med J (Engl) 1979 92:671-76. [Google Scholar]
[9]. Abdi U, Tyagi N, Maheshwari V, Tumours of eyelid: a clinicopathologic studyJ Indian Med Assoc 1996 94:405-09. [Google Scholar]
[10]. Font RL, Eyelids and Lacrimal drainage system. In: Spencer WH, edOphthalmic pathology: an atlas and textbook 1996 Vol 44th edPhiladelphiaWB Saunders:2218-433. [Google Scholar]
[11]. Rao NA, Hidayet AA, McLean IW, Sebaceous carcinomas of the ocular adnexa: a clinicopathologic study of 104 cases, with 5-year follow-up dataHum Pathol 1982 13:113 [Google Scholar]
[12]. Nunery WR, Welsh MG, McCord CD, Recurrence of sebaceous carcinoma of the eyelid after radiation therapyAm J Ophthalmol 1983 96(1):10 [Google Scholar]
[13]. Yen MT, Tse DT, Wu X, Wolfson AH, Radiation therapy for local control of eyelid sebaceous cell carcinoma: report of two cases and review of the literatureOphthal Plast Reconstr Surg 2000 16(3):211-15. [Google Scholar]
[14]. Hata M, Koike I, Maegawa J, Kaneko A, Odagiri K, Kasuya T, Radiation therapy for primary carcinoma of the eyelid: tumour control and visual functionStrahlenther Onkol 2012 188(12):1102-07. [Google Scholar]
[15]. Hata M, Koike I, Omura M, Maegawa J, Ogino I, Inoue T, Noninvasive and curative radiation therapy for sebaceous carcinoma of the eyelidInt J Radiat Oncol Biol Phys 2012 82(2):605-11. [Google Scholar]