Microfilariae, a Common Parasite in an Unusual Site: A Case Report with Literature Review
C.S. Rohini Dhanya1, H.T. Jayaprakash2
1 Tutor, Department of Pathology, Dr. B.R. Ambedkar Medical College & Hospital, Bangalore, India.
2 Professor and HOD, Department of Pathology, Dr. B.R. Ambedkar Medical College & Hospital, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rohini Dhanya. C.S, Tutor, Department of Pathology, Dr. B.R. Ambedkar Medical College & Hospital, Bangalore - 560045, India.
E-mail: dr.rohinidhanya@gmail.com
Filariasis is common in tropical countries. Wuchereria bancrofti is the most common parasite which causes lymphatic filariasis in India. This paper reports the finding of microfilariae in cervicovaginal smear of a 61-year-old post menopausal woman with a brief review of literature. There are limited numbers of reports describing the presence of microfilariae in the cervicovaginal smears and even rarely as an incidental finding. It is very important to keep in mind and screen for microfilariae in the non-endemic areas also.
Cervicovaginal smear, Filariasis, Postmenopausal woman
Case Report
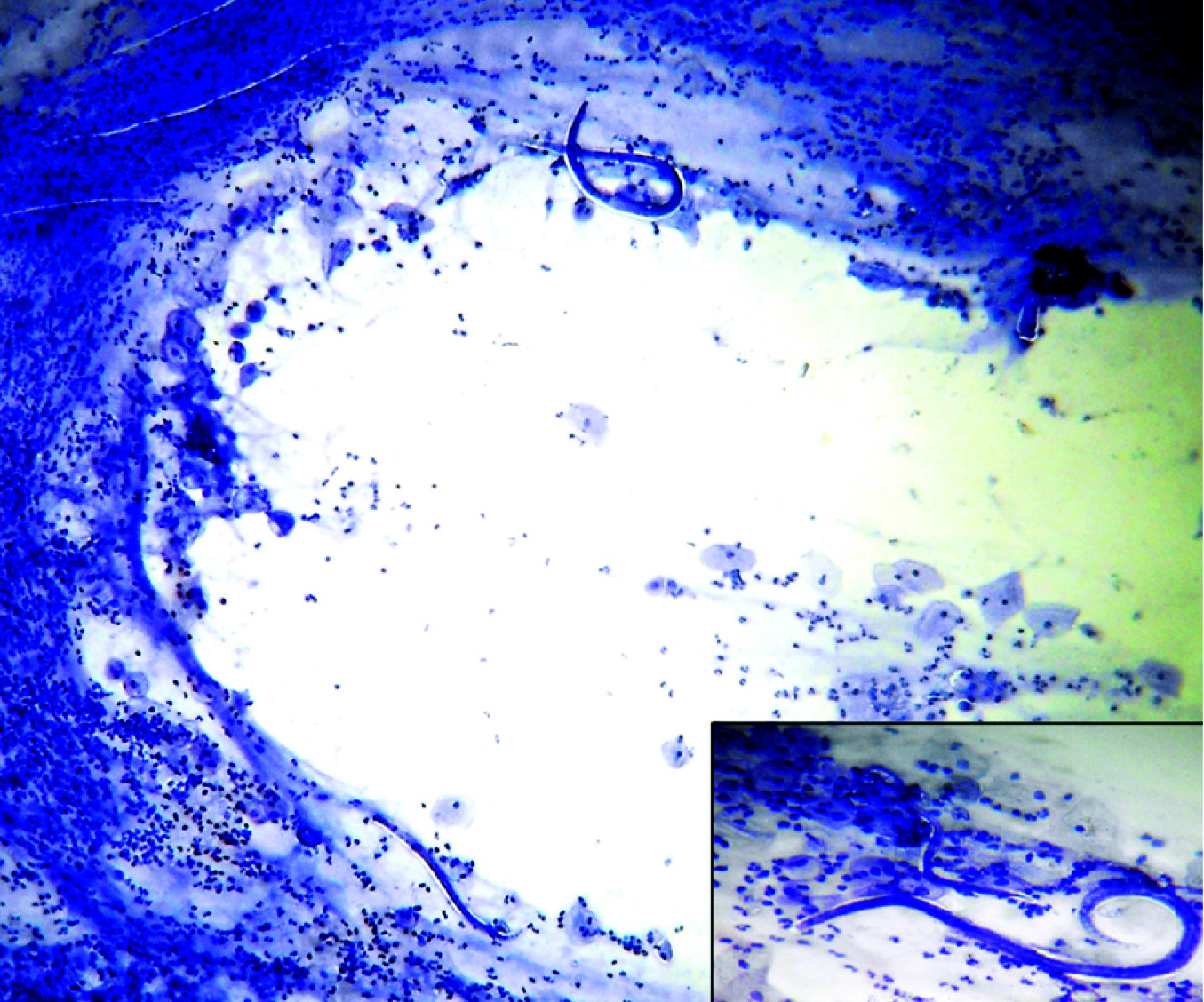
A 61-year-old postmenopausal woman presented to Obstetrics and Gynaecology Department with chief complaints of generalized weakness and white discharge per vagina of 1 week duration. She had mild fever fluctuating for 7 days about one month back. Her vital parameters and systemic examinations were normal. Haematological and biochemical findings were within normal limits. Per vaginal examination revealed a cervical polyp measuring 1.5×1cm with white discharge. Cervicovaginal smears were wet fixed in 95% ethyl alcohol and stained with Papanicolou stain. The smears revealed sheathed microfilariae with its smooth graceful curves and well stained nuclei not extending upto the tip of the tail surrounded by intense inflammatory cells [Table/Fig-1,2].
Microfilariae of Wuchereria bancrofit in the cervico-vaginal smear [PAP stain x 40]. Inset: Microfilariae [x400]
Microfilara showing smooth graceful curves, well stained nuclei and the tip is free
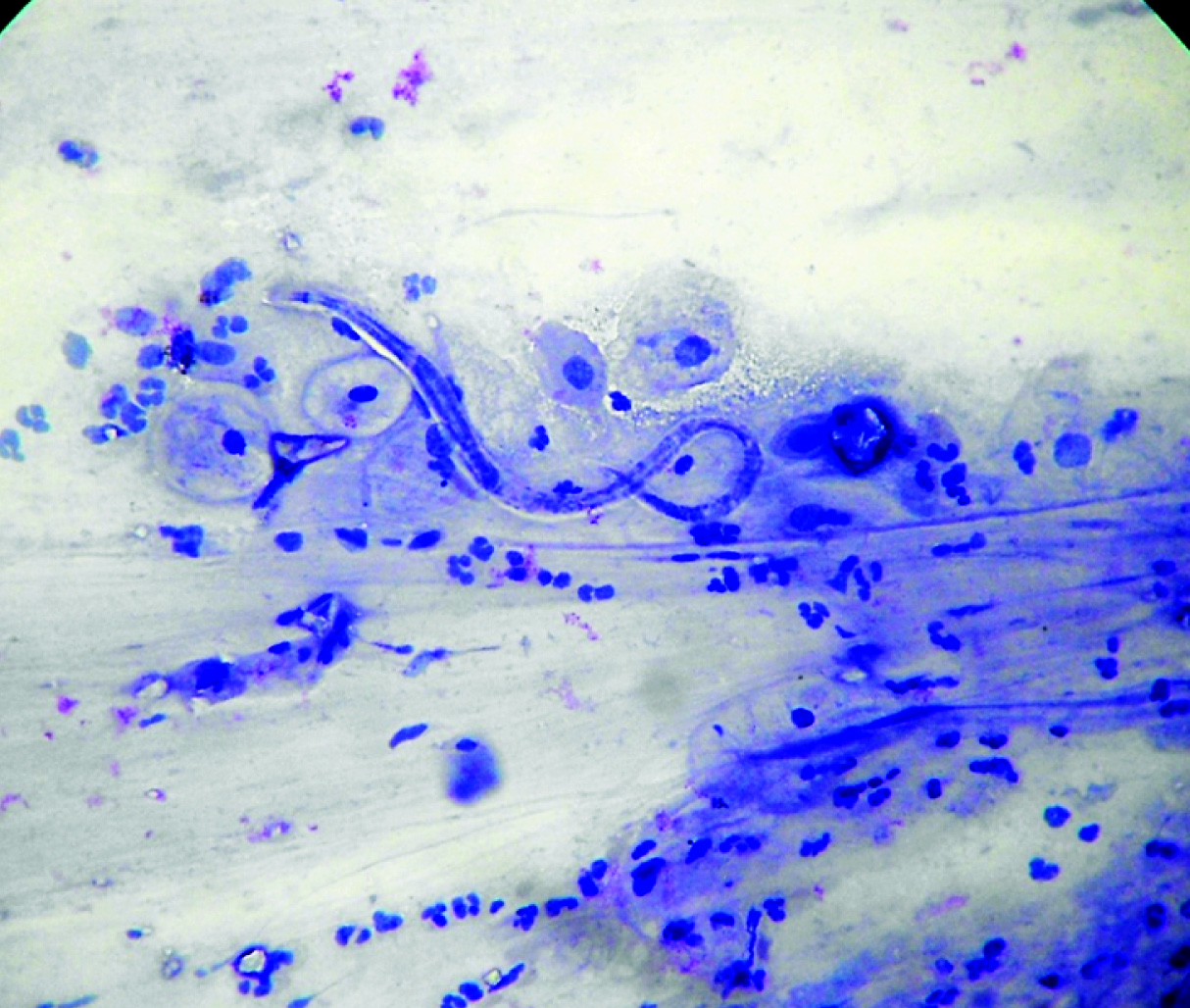
There was no clinical evidence of filariasis or microfilaraemia. Further investigations with repeat peripheral smear study of post-noon and night blood samples by finger-prick method was done to rule out subperiodic form or nocturnal periodicity. Microfilariae were not found in the smears. We are reporting an incidental finding of microfilariae of Wuchereria bancrofti in cervicovaginal smear – an occult filariasis. Histopathologic examination of cervical polypectomy specimen did not show any microfilariae or adult worms. The patient was treated with Diethylcarbamazine citrate in the dose of 6mg/kg body weight per day for 12days and further follow-ups showed complete recovery with no recurrence.
Discussion
Filariasis is a serious public health problem in developing countries like India. It is endemic in Uttar Pradesh, Bihar, Orissa, Jharkhand, Gujarat, Andra Pradesh, Tamil Nadu and Kerala [1]. Lymphatic filariasis is a neglected tropical disease [2]. Clinical filariasis is conventionally diagnosed in peripheral smear, associated with eosinophilia and other clinical manifestations. It has a great impact on the physical well-being, economic status and on the quality of life of the infected person, their families and the community. Here we report a case of microfilariae in cervicovaginal smear of an elderly woman.
Lewis found the microfilariae in blood in 1872. Filariasis is a major social and economic burden in the tropics and subtropics of Africa, Asia, Western Pacific and parts of America. Currently, more than 1.4 billion people in 73 countries are at risk and about 25 million men are afflicted with genital disease [2].
Humans are the only known reservoir host. The filarial parasites are transmitted to humans through the mosquitoes especially culex mosquitoes across urban areas, anopheles mosquitoes in rural areas and aedes in endemic islands [2]. Stains such as Giemsa, Wright’s, Papanicolou or Delafield’s haematoxylin are used to differentiate the morphological features for species identification [Table/Fig-3] [3,4].
Morphological features of species causing human filariasis [4]
| Species | vector | Location ofadult | Location ofmicrofilaria | periodicity | Sheath,appearance | Length [μm] | Tail nuclei |
|---|
| 1 | WuchereriaBancrofti | CulexAedesAnopheles | Lymphatic | BloodHydrocele fluid | NocturnalSubperiodic | PresentGraceful sweeping curves | 260(244-296) | Do not extend to tip of tail, tail tapers to delicate point |
| 2 | Brugia malayi | MansoniaAnopheles | Lymphatic | Blood | NocturnalSubperiodic | PresentStiff with secondary kinks | 220(177-230) | Subterminal & terminal, tail contricted at 2 terminal nuclei |
| 3 | Brugia timori | Anopheles | Lymphatic | Blood | Nocturnal | PresentTapering gradually | 310(290-325) | Subterminal & terminal |
| 4 | Loa loa | Deerfly | Subcutaneous | Blood | Diurnal | Present | 275(250-300) | Continous to tip of tail |
| 5 | Mansonella perstans | Midge | Body cavitiesMesentryperirenal | Blood | None | Absent | 195(190-200) | Continous to tip of tail |
| 6 | Mansonella ozzardi | MidgeBlackfly | SubcutaneousBody cavities | Blood | None | Absent | 200(173-240) | Do not extend to tip of tail |
Chronic filariasis presents with swelling of legs, hands, scrotum, labia or breast [2]. No evidence of clinical filariasis such as lymphoedema or swelling of labia or lower limbs was seen in our case. Cervicovaginal smears revealed microfilariae without eosinophilia and microfilaraemia. All other parameters were normal. We consider the presence of microfilariae in our case as an incidental finding. It is also an unusual finding in our institute. The patient had visited a place in Tamil Nadu one year back. Filarial infection should always be considered in the differential diagnosis of tissue and haemoparasites in all the individuals who have resided in and/or migrated from endemic areas [5].
Anticipated oxidative stress during inflammatory response to infective conditions might complicate the immune response and thus alter the disease outcome. This may explain the reason for the absence of peripheral blood eosinophilia seen in the chronic and occult filariasis [6].
When we reviewed the literature, similar findings were reported by Walter A et al., and others [7–10]. Walter A et al., found such cases in the absence of clinical filariasis. Symptomatic vaginal bleed was present in 9 out of 17 cases [7]. In our case, the patient presented with white discharge per vagina. Fitzhugh et al., showed the significance of pap smear in diagnosing several microorganisms including microfilariae [10]. The paucity of such cases merits its presentation.
A review of literature reveals incidental detection of microfilariae in various locations including aspirates of lymph node, joint spaces, thyroid, bone marrow, brain, breast, nipple discharges, pleural and pericardial effusions, bronchial washings, urine, CSF, cutaneous swelling, soft tissue aspirates, endometrial smears, ovarian cyst fluid, cervicovaginal smear, epididymis, hydrocele fluid [1,7,11].
Broad spectrum antibiotics are given usually for fever which is ineffective for the parasitic infestations. This leads to unnecessary consumption of antibiotics.
Circulating filarial antigens can be detected in the peripheral blood using commercial kits- ELISA Og4C3 monoclonal antibody - based assay and immunochromatography for quantitative and qualitative assessment respectively.
Over 120 million people are currently infected with filariasis out of which around 40 million patients are disfigured leading to social stigma as well as financial hardship from medical expenses and loss of employment [2]. Since the prevalence and intensity of infection are linked to poverty, its elimination can contribute to achieving the United Nations Millennium Development Goals [2]. Such a public health problem is responded by the WHO by initiating the Global Programme to Eliminate Lymphatic Filariasis (GPELF) and its goal is to eliminate lymphatic filariasis by 2020 [2].
Conclusion
Absence of microfilariae in peripheral smear does not exclude filarial infection. A high index of suspicion in mind and a cautious screening is essential by the cytopathologist in materials from any site of the body for early diagnosis and to direct the clinicians for the definite treatment. This may obviate further serious pathologic changes, especially disfigurement.
[1]. Kolte SS, Satarkar RN, Mane PM, Microfilaria concomitant with metastatic deposits of adenocarcinoma in lymph node fine needle aspiration cytology: a chance findingJ Cytol 2010 27(2):78-80. [Google Scholar]
[2]. http://www.searo.who.int/thailand/factsheets/fs0012/en/ [Google Scholar]
[3]. Webber CA, Eveland LK, Cytologic detection of wuchereria bancrofti microfilariae in urine collected during a routine workshop for haematuriaActa Cytol 1982 26(6):837-40. [Google Scholar]
[4]. Lynne Shore Garcia, Filarial nematodesDiagnostic Medical Parasitology4th ed:330 [Google Scholar]
[5]. Hira PR, Lindberg LG, Ryd W, Behbehani K, Cytologic diagnosis of Bancroftian filariasis in a non-endemic areaActa cytol 1988 32:267-69.[PubMed] [Google Scholar]
[6]. Pal BK, Kulkarni S, Bhandari Y, Ganesh BB, Goswami K, Reddy MVR, Lymphatic filariasis: possible pathophysiological nexus with oxidative stressTransactions of the Royal Society of Tropical Medicine & Hygeine 2006 100(7):650-55. [Google Scholar]
[7]. Walter A, Krishnaswami H, Cariappa A, Microfilariae of Wuchereria Bancrofti in cytologic smearsActa Cytol 1983 27:432-36.[PubMed] [Google Scholar]
[8]. Punia RS, Khullar U, Handa U, Mohan H, Microfilaria in cervicovaginal smearCytopathology 2005 16(3):156-57. [Google Scholar]
[9]. Valand AG, Ramraje SN, Surase S, Microfilariae of Wuchereria Bancrofti in cervicovaginal smearsIndian J Pathol Microbiol 2004 47(4):597-98. [Google Scholar]
[10]. Fitzhugh VA, Heller DS, Significance of a diagnosis of microorganisms on pap smearJ Low Genital Tract Dis 2008 12(1):40-51. [Google Scholar]
[11]. Varghese R, Raghuveer CV, Pai MR, Bansal R, Microfilariae in cytologic smears: A report of six casesActa Cytol 1996 40:299-301. [Google Scholar]