Body temperature is regulated through a dynamic balance between heat production and heat loss. The regulatory mechanisms fail to work above the body temperature of 40oC resulting in multi organ injury [5]. In hotter conditions cooling effect of evaporation from the skin becomes an important factor. Efficiency of this cooling depends on air humidity [6]. It has been observed that deaths due to heat wave are more over the regions where the normal maximum temperature itself is more than 40°C [7]. In our earlier study (2011), we compared perioperative morbidity in elderly (>60 years) surgical patients over a period of one year. It was observed that elderly surgical patients had a poor perioperative outcome in hot and humid weather [8]. Bhattacharya et al., found higher admissions due to trauma with increase in average daily temperature [9]. Farmers and labourers working in open fields are exposed to direct atmospheric heat. Moreover industrial workers get exposed to industrial pollution and high humidity levels in factories. Many of factories in India do not have facility of air conditioning. Although a lot of research have been carried out to evaluate effect of hot climatic conditions and its correlation with other medical conditions, but very less has been studied in trauma patients. Thus we proposed to study trauma patients who are exposed to hot weather and higher risk of injury [7–9]. We thus designed study to evaluate the impact of hot climatic conditions on perioperative complications in trauma patients.
To evaluate the impact of hot climatic conditions on perioperative morbidity among trauma patients and to compare it with comfortable climatic conditions.
Materials and Methods
This prospective study was conducted in a tertiary care hospital of India after approval by the Hospital Ethical Committee and University. In Punjab, the climatic conditions often vary seasonally from a cool winter to a very hot summer as per the meteorological data from Punjab Agricultural University (PAU), Ludhiana, Punjab. The temperature and relative humidity in summer remain often above 400C and nearly 100% respectively making it uncomfortable weather. In months from mid February to end of March and Mid October to end of November, the weather is very pleasant and comfortable. The study data was collected from March 1, 2010 to June 30, 2011 to enroll the required number. We gathered daily data from meteorological department, PAU to enroll patients. A written informed consent was taken from all the patients or attendants if patient is incompetent to give consent. As per observations from our previous published work [8], we enrolled 100 trauma patients aged between 20-70 years of either gender with ASA grade I-III scheduled for surgery with 50 patients in each group patients were grouped as Control Group (C) when outdoor temperature ranged in comfortable zone i.e. 20-290C and Study Group (S) when outdoor temperature ranged 400C or more. Patients living in regular air conditioned environment (more than 18 hours per day) or patients who stayed in air conditioned area of hospital for > 72 hours prior to surgery were excluded. Patients with medical conditions which were likely to bias study; hyperthyroidism, hypothyroidism, neurosurgical, malignant hyperthermia were excluded. Patients on drugs interfering with temperature regulation such as- -β blockers, anticholinergics, phenothiazines or other neuroleptic drugs, were excluded from study. Environmental record: Peak outdoor temperature, relative humidity and evaporation index were noted from Meteorological Department, Punjab Agricultural University, Ludhiana. Heat index was derived from the above noted values with the formula given below:
Heat Index (HI) [10] or apparent temperature (AI) = –42.379 + 2.04901523(Tf) + 10.14333127(RH) – 0.22475541(Tf) (RH) – (6.83783x10-3) (Tf2) – (5.481717 x10-2) (RH2) + ((1.22874x10-3) (Tf2)(RH) + (8.5282 × 10-4) (Tf) (RH2)) – (1.99x10-6) (Tf2) (RH2)
Tf = Temperature in Fahrenheit
RH = Relative humidity
All patients included in the study were assessed pre-operatively in detail for old and new medical problems, injury details, economical status and medications including alternative medicine. We noted socioeconomic status also as poor patients had poor living conditions [11]. Socioeconomic status of patients was assessed using Kuppuswamy’s socioeconomic status scale [12]. Patient’s risk stratification was done on basis of ASA physical status [13], trauma index score [14] and Shoemaker’s risk criteria [15]. Nature of surgery was also recorded. Preoperative vitals and investigations were noted. Nature of surgery (emergency/elective), nature of anaesthesia, operative procedure, duration of surgery and vitals was recorded. Total blood and blood component transfusions were noted. Perioperative complications, if any, were recorded in the performa attached along with the time of the episode (hypotension, tachycardia/bradycardia, dysarrhythmias, myocardial ischaemia and myocardial infaraction, respiratory distress, oliguria, anuria, acute renal failure, liver dysfunction, multiple organ dysfunction syndromes, infections including details).
The Post Anaesthesia Care Unit, Intensive Care Unit and Hospital stays were noted in every patient. All patients showing signs of postoperative ischemia or unexplained hypotension were subjected to troponin-T investigation to rule out ischemic injury. Postoperatively patients were observed for any signs of septicaemia (as evident from fever, increased white cell count or culture report). All these observations were recorded in the Performa and analysed using student’s t-test, z-test and chi-square test for statistical significance. Multivariate logistic regression analysis was used to compare the risk factors for morbidity.
Results
Patients were comparable in both groups with regards to their demographic characteristics, socioeconomic status, ASA physical status, trauma index score and Shoe Maker’s risk score [Table/Fig-1,2]. Most patients (92% in group C and 94% in group S) belonged to middle socioeconomic class (II & III). Most of patients in group C and S belonged to ASA physical status I & II. Most patients in both groups (40 in C and 46 in S) suffered from minor trauma (TIS 0-7). Mean Trauma Index Score was 6.20 ± 1.56 and 5.80 ± 1.31 in both groups respectively with a p-value 0.071. However, there was more number of patients with moderate trauma (Trauma Injury Score 8-18) in group C (10) than group S (4). Both groups had similar number of patients 96% and 4% belonging to low risk and high risk respectively as per Shoe Makers Risk Score.
Comparison of demographic parameters and risk score among two groups.
| Parameters | Group-C | Group-S | p-value |
|---|
| Age | 38.20 ± 12.93 | 40.14 ± 15.98 | 0.25 |
| Male | 46 (92) | 38(76) | NS |
| Females | 4(8) | 12(24) | NS |
| ASA I and II | 49 (98) | 48 (96) | 0.28 |
| Trauma index score | 6.20 ± 1.56 | 5.80 ± 1.31 | 0.07 |
| Trauma index score0-7 | 40 (80%) | 46 (92%) | NS |
| Trauma index score8-11 | 10(20%) | 4(8%) | NS |
| Shoe Makers Risk CriteriaLow Risk | 48 (96%) | 48 (96%) | NA |
| Shoe Makers Risk CriteriaHigh Risk | 2(4%) | 2(4%) | NA |
Distribution according to socio-economic status.
| SES | Group-C | Group-S |
|---|
| No. | %age | No. | %age |
|---|
| I | 0 | 0.00 | 1 | 2.00 |
| II | 36 | 72.00 | 30 | 60.00 |
| III | 10 | 20.00 | 17 | 34.00 |
| IV | 4 | 8.00 | 1 | 2.00 |
| p-value | 0.07737 |
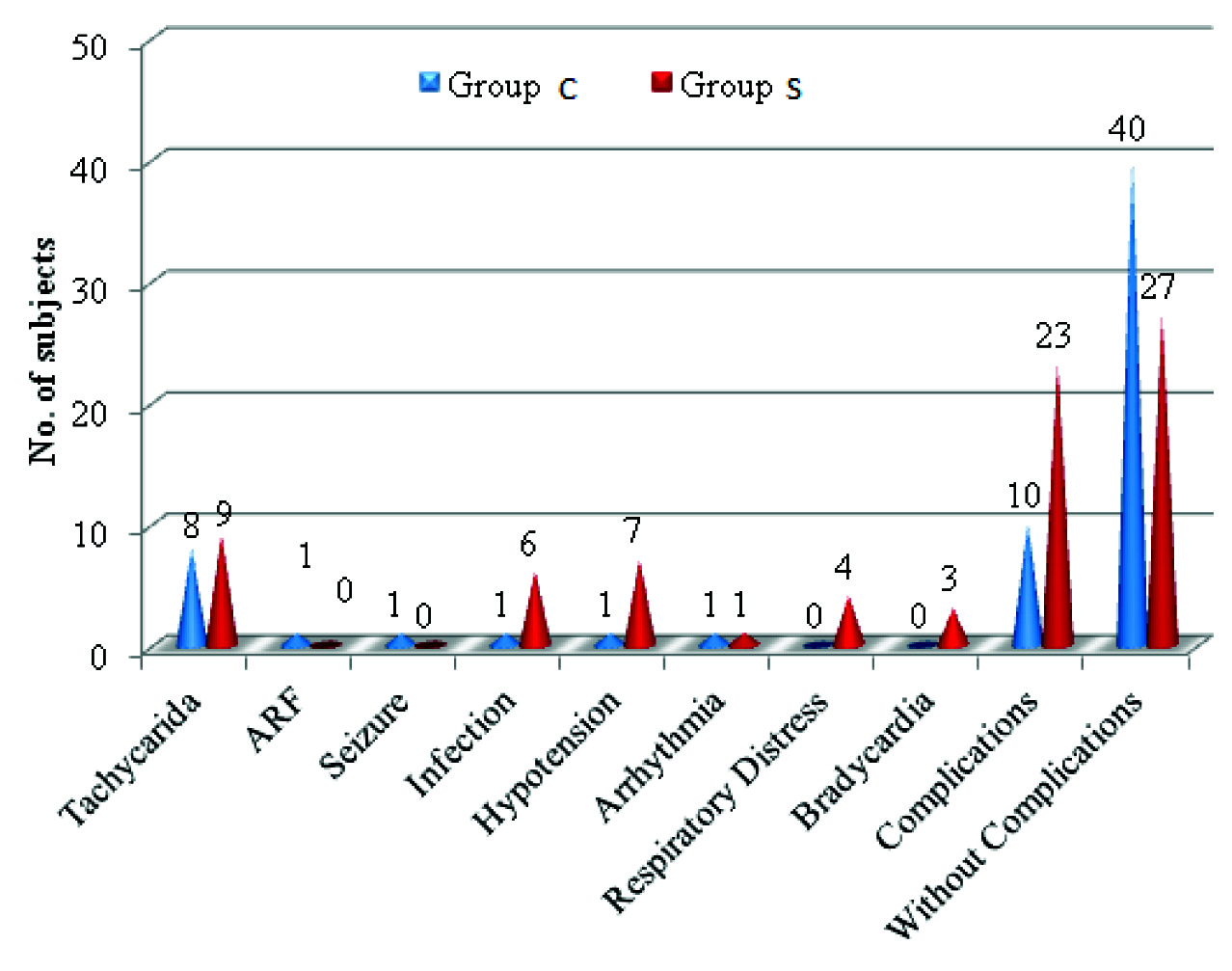
In group C (comfortable zone), mean temperature was 24.14 ± 3.07°C whereas in group S (zone of great discomfort) it was 41.12 ± 1.09°C (p-value 0.00001) [Table/Fig-3]. On further sub grouping within group I, 68% of patients were admitted when ambient temperature prevailed between 20-25°C and 32% in 25-29° C. Whereas in the second group, 52% had admission to hospital when peak temperature was between 40-41°C and the rest 48% had temperature >41°C at the time of admission. Mean relative humidity (%) in group C was 93.24 ± 6.73 compared to 55.82 ± 14.46 in group S (p-value 0.00001). We found significant difference among both groups with regards to the peak evaporation index. Mean peak evaporation index (mm) was higher in group S (9.67 ± 1.63) as compared with group C (2.12 ± 1.13) with a p-value of 0.00001. There was statistically significant difference in the two groups on basis of heat index (p-value =0.00001). Mean heat index in Group C and S were respectively 77.62 ± 13.28 and 148.48 ± 21.80. No statistical difference was found among both groups in relation to PACU and ICU stay [Table/Fig-4]. Mean duration of hospital stay (days) was found to be 12.16 ± 8.50 in group C and 10.98 ± 6.90 in group S and was non-significant statistically (p-value 0.22). 50% of patients in group C and 58% in group S were discharged within 10 days of admission. 6 patients in each groups stayed in the hospital for > 20 days. Patients belonging to ASA class I and II were found to have higher complications in study group during hot weather (p-values 0.009) [Table/Fig-5]. Patients belonging to lower middle and upper lower socioeconomic classes (classes III and IV) were found to have higher complications if they got admitted to hospital during hot climate (p-values 0.009 & 0.04 respectively) [Table/Fig-6]. Patients with even minor trauma (on the basis of trauma index score) had significantly higher risk of perioperative complications in group S (p-value 0.008) as compared to control group I [Table/Fig-7]. In group C, only 10 patients (20%) whereas in group S, 23 (54%) patients had complications (p-value = 0.009). Incidence of tachycardia was comparable in both groups. There was significantly higher incidence of infectious complications (p-value= 0.05) as well as respiratory distress (p-value= 0.04) in group s patients. Six patients (12%) in group S but only 1 (2%) in group C suffered from infection during the course of their hospital stay. There was a higher incidence of hypotension in group S (14%) compared to group C (2%) with a p-value of 0.04. In group S, 4 patients (8%) suffered from respiratory distress and 3 (6%) had bradycardia. In group C, one patient had acute renal failure and one had seizures postoperatively [Table/Fig-8]. Multiple logistic regression analysis was used to compare patients on the basis of age, gender, different heat variables and trauma index score. Peak environmental temperature was found to be the single independent risk factor for predicting perioperative complications (p-value =0.003).
Distribution of Heat variables.
| Group-C | Group-S | p-value |
|---|
| Peak Temperature (°C) | 24.14 ± 3.07 | 41.12 ± 1.09 | 0.00001 |
| Relative humidity (%) | 93.24 ± 6.73 | 55.82 ± 14.46 | 0.00001 |
| Evaporation index (mm) | 2.12 ± 1.13 | 9.67 ± 1.63. | 0.00001 |
| Heat index | 77.62 ± 13.28 | 148.48 ± 21.80 | 0.00001 |
Note: values are shown as mean ± SD in table and text.
Comparison of subjects according to duration of hospital stay.
| Duration of Stay (days) | Group-C | Group-S |
|---|
| No. | %age | No. | %age |
|---|
| Upto 10 | 25 | 50.00 | 29 | 58.00 |
| 11-20 | 19 | 38.00 | 15 | 30.00 |
| 21-30 | 4 | 8.00 | 6 | 12.00 |
| 31-40 | 2 | 4.00 | 0 | 0.00 |
| Mean | 12.16 | 10.98 |
| SD | 8.50 | 6.90 |
| p-value | 0.21650 |
Complications in relation to ASA status.
| ASA Status | No. of patients with Complications | p-value |
|---|
| Group-C | Group-S |
|---|
| Total no. of pts | Pts with comp | %age | Total no. of pts | Pts with comp | %age |
|---|
| I+II | 49 | 9 | 18.37 | 48 | 22 | 45.83 | 0.009 |
| III | 1 | 1 | 100.00 | 2 | 1 | 50.00 | |
Complications in relation to socio-economic status.
| SES | No. of patients with Complications | p-value |
|---|
| Group-C | Group-S |
|---|
| Total no. of pts | Pts with comp | %age | Total no. of pts | Pts with comp | %age |
|---|
| I | 0 | | | 1 | 1 | 100.00 | |
| II | 36 | 10 | 27.78 | 30 | 12 | 40.00 | 0.157 |
| III | 10 | 0 | 0.00 | 17 | 9 | 52.94 | 0.009 |
| IV | 4 | 0 | 0.00 | 1 | 1 | 100.00 | 0.044 |
Complications in relation to Trauma Index Score.
| Trauma Index Score | No. of patients with Complications | p-value |
|---|
| Group-C | Group-S |
|---|
| Total no of pts | pts with comp | %age | Total no of pts | Pts with comp | %age |
|---|
| 4-7 | 40 | 6 | 15.00 | 46 | 22 | 47.83 | 0.008 |
| 8-11 | 10 | 4 | 40.00 | 4 | 1 | 25.00 | |
Discussion
The relationship between human health and stressful weather is a complex medical, social and environmental issue. A study by Chaudhary SK et al., has shown that the average annual loss of human life due to heat wave over India is 153 [7]. The loss of human life due to heat wave is maximum in Rajasthan followed by Bihar, UP and Orissa. Sartar F et al., found that elevated outdoor temperature combined with high ozone concentrations were the likely important causes of excess mortality in hot climate which has been corroborated in various surveys [2,3]. They observed that heat related deaths were more prone to occur on day with peak daily temperature > 38oC and incidence of these deaths showed an exponential dependence on the number of hot days. Medical disorders like bronchitis, peptic ulcer, eczema, herpes zoster are related to seasonal variations in temperature. Myocardial infarction and cerebrovascular accidents represent two general mortality categories which have been correlated with monthly ambient temperature [16]. In this study we observed that hot climate adversely affects the perioperative period in trauma patients.
Our patients were comparable on the basis of their demographic profile i.e. age and socioeconomic status. Most patients in our study were young males belonging to middle socioeconomic status. However, on further subgrouping according to socioeconomic status as per [Table/Fig-2], patients belonging to poor socioeconomic status (class III and IV) in study group had higher complications than in group C [Table/Fig-5b]. It corroborates the findings of McGeehin et al., and Kuan-che Lu et al., that poor socioeconomic status groups were more prone to side effects of hot weather despite their adaptation due to prolonged heat exposure [3,5]. As heat loss is proportional to square root of wind velocity, lower socioeconomic status populations are at a higher risk of heat related illnesses [5]. Probably they were more exposed to risk and have poor air conditioning facility. We did not record the exact demographics i.e. housing, type of urbanization etc. Patients in both groups were comparable in risk scores as per [Table/Fig-1]. Most of patients in our study suffered from minor degree of orthopedic trauma (80% in C and 92% in S) with a mean Trauma Index Score of 6.20 ± 1.56 and 5.80 ± 1.31 in group C and S respectively with p-value 0.07. Patients mostly belonged to low risk Shoemaker’s score. The mean duration of PACU and ICU stay as well as the overall hospital stay were found to be similar in both the groups [Table/Fig-9]. However, in our previous study among elderly surgical patients, they had prolonged hospital stay in hot climate [8]. This may be due poor reserves in elderly patients resulting in higher morbidity. We found that 46% patients in group S and only 10% patients in group C had complications (p-value = 0.009). It was further seen that there were more complications related to the cardiorespiratory system. Probably, it resulted from the decompensation of these systems due to SIRS (severe inflammatory response syndrome) due to hot weather and trauma. Also, body’s ability of thermoregulation is impeded when too much blood is diverted from vital organs to skin surface on exposure to high temperature, putting increased stress on the vital organs like heart and lungs [16]. There was even a higher incidence of infectious complications in group S. Probably, high temperature and humidity led to dehydration compromising splanchnic circulation leading to translocation of bacteria from gut [17]. Secondly, it may be high humidity and sweat resulting in infectious pockets in skin folds and leading to infections from breached skin due to trauma and intravascular catheters. However, we did not study the pattern and epidemiology of infections in our patients. Traumatic hypothalamic injury may facilitate and potentiate heat related illness. On multivariate regression analysis comparing age, gender, various heat variables and trauma index score it was found that temperature was the single most important risk factor for the development of perioperative complications. It is obvious from our results that patients having surgery in hot climate had more complications and that there was a better perioperative outcome in patients during comfortable ambient temperature.
Comparison according to PACU and ICU stay (days).
| PACU/ICU Stay (days) | Group-C | Group-S |
|---|
| No. | %age | No. | %age |
|---|
| Upto 2 | 48 | 96.00 | 48 | 96.00 |
| 2-3 | 2 | 4.00 | 1 | 2.00 |
| 3-4 | 0 | 0.00 | 0 | 0.00 |
| 4-5 | 0 | 0.00 | 1 | 2.00 |
| Mean | 0.84 | 0.89 |
| SD | 0.57 | 0.72 |
| p-value | 0.42857 |
Temperature, humidity, wind and sunshine are the important climatic elements of the environment which directly influences body’s comfort as well as well being [17]. However, when temperature changes are sudden or extreme it does lead to morbidity and health hazards due to poor adaptation. Excess heat is lost by radiation to surroundings, evaporation from skin and respiratory passages, conduction to air and cold objects and convective transport in moving air. Ambient temperature and other outdoor climatic factors such as relative humidity, evaporation, air pollution etc affect the dissipation of heat. Active sympathetic cutaneous vasodilatation can increase skin blood flow by up to 8 litres/minute. As blood gets shunted from the central circulation to skin and muscles in order to facilitate heat dissipation, there occurs reduced visceral perfusion, particularly in the intestines and kidneys [17].
There is no universal definition of heat wave as this term is relative to the usual weather in a particular area. So, heat wave as recommended by the glossary of meteorology is defined as: A period of abnormally and uncomfortably hot and usually humid weather. More realistically, the comfort criteria for any one region are dependent upon the normal conditions of that region. With the current concern for global warming it is reasonable to suppose that they may increase in frequency, severity, duration, or a real extent in the future. According to the India Meteorological Department (IMD), at places where normal maximum temperature is more than 40°C heat wave is said to occur if day temperature exceeds by 3-4°C and when the day temperature is 5°C or more than normal severe heat wave is said to persist. At places where maximum temperature is usually 40°C or less, increase in day temperature by 5-6°C defines a moderate heat wave and if day temperature exceeds by more than 6°C, then severe heat wave occurs [7]. The old saying “its not the heat, its the humidity” holds true. So, humid air can be significantly less comfortable than drier air at the same temperature [18]. It interferes with evaporation. Semenza et al., found higher rate of hospital admissions in months of June & July during periods of heat wave. Heat related illnesses were more among people with underlying medical conditions [19]. There are number of studies which reported the heat wave related morbidity and mortality indicated that it is a major health hazard [1,3,20]. Some reported that it affects the extremes of age [4].
Our study is novel, so there is a paucity of literature to compare. However, if we see the physiological adaptation of hot weather, it becomes a supportive evidence that patients who have compromised cardiorespiratory reserves have higher rate of morbidity and thus would have poor surgical outcome in hot and humid weather. Current study corroborates some of the findings of our previous study on hot climate and perioperative outcome in elderly patients. As in our region, the change in weather is gradual as compared to coastal regions and also there is a balancing effect of wind on high temperature i.e. whenever temperature is high, the evaporation index also goes up to counteract the effect of humidity, so there is better adaptation and acclimatization to climate.
Limitations
There were many limitations of our study. Overall sample size was small to find out the relationship of complications with various variables and intragroup comparison. Secondly climatic conditions are never controlled and impact of temperature gets biased with wind and humidity level. Weather is never uniform over time and place. We have recorded temperature from our city and it may not represent the true climate where patient has resided over last week. Another limitation is type of trauma. All patients had minor orthopedic trauma. Major trauma patients may be at higher risk. There were more females in group S. Although it is well known that female gender generally tolerates stress better than males, but as per various climatic studies, females are more prone to heat related complications [20,21].
Global warming is increasingly recognized as a threat to the survival of human beings and it heats up the whole world thus there is a greater tendency to experience heat waves everywhere [22,23]. Due to its large population and widespread environmental degradation, Asian region will be particularly vulnerable to future climate change and global warming. So, it is a forthcoming concern of trauma patients during hot weather due to its relation and adverse impact on trauma morbidity. Particularly neurosurgical trauma may be at higher risk of these complications [24].
Conclusion
High ambient temperature adversely affects the outcome of trauma patients. Patients with poor cardiorespiratory reserves may be at a higher risk of peri-operative complications. Patients belonging to lower socioeconomic status have a higher chance of getting complications during hot climate.
Note: values are shown as mean ± SD in table and text.