Tympanoplasty is one of the most common surgery performed in the Department of Otolaryngology. During the last hundred years various modifications in the surgical technique have been introduced because of continued efforts made by otologists all over the world to achieve the best surgical outcome. With the advent of otoendoscopes, the traditional techniques have been modified to minimal invasive surgery achieving better results and less complication rate.
Type 1 involves repair of the tympanic membrane alone, when the middle ear is normal. A type 1 tympanoplasty is synonymous to myringoplasty.
Type 2 involves repair of the tympanic membrane and middle ear in spite of slight defects in the middle ear ossicles.
Type 3 involves removal of ossicles and epitympanum when there are large defects of the malleus and incus. The tympanic membrane is repaired and directly connected to the head of the stapes.
Type 4 describes a repair when the stapes foot plate is movable, but the crura are missing. The resulting middle ear will only consist of the eustachian tube and hypotympanum.
Type 5 is a repair involving a fixed stapes footplate.
The surgical procedure tympanoplasty has achieved a state of art over the years. Various techniques have been attempted in order to achieve better results with improved hearing. These include the overlay tympanoplasty [3], the underlay tympanoplasty [4], over underlay tympanoplasty [5], Gelfilm sandwich tympanoplasty [6], Crown cork tympanoplasty [7], Swinging door tympanoplasty [8], laser assisted spot welding techniques [9], microclip techniques [10] and others like the fascial pegging [11], annular wedge tympanoplasty [12], loop tympanoplasty [13], paper patching, lobule fat graft and the self-stabilizing tympanic membrane patchers [14].
Karhuketo et al., has emphasized that the endoscopic method fulfills the requirements of minimally invasive surgery, and has documented better visualization and assessment of ossicles and middle ear structures [16].
The study aimed to compare the graft acceptance and complications associated with the Permeatal Sandwich Tympanoplasty with the help of otoendoscope and traditional Postaural Underlay technique.
Materials and Methods
An Ethical approval was obtained from the institutional ethical committee and a comparative study was under taken in the Department of ENT of a rural tertiary care center.
The study was undertaken for one year period in which, patients attending the ENT OPD suffering from Chronic Suppurative Otitis Media (CSOM) were selected on the basis of type of perforation. Their candidature for tympanoplasty was assessed by performing the workup in the form of thorough examination of the Ear, Nose and Throat and assessment with documentation of the hearing loss was done with the help of pure tone audiometry. Affection of the mastoids were ruled out with the help of x-ray mastoid bilateral oblique view. An oto-microscopic examination of the cases was performed to confirm the findings of otoscopy and assessment of the middle ear structures. A written informed consent was sought from the patients, explaining the benefits and risk, and type of procedure to be performed. The procedure of tympanoplasty was performed by the Permeatal Sandwich Tympanoplasty and traditional Postaural Underlay technique, and, the results were assessed in terms of graft take up, associated complication and improvement in hearing; the results were compared after 21 days of postoperative period.
Inclusion criteria
(1) Patients having chronic suppurative otitis media with inactive disease (6 weeks of dry ear).
(2) Patients of chronic suppurative otitis media with pure conductive hearing loss (assessed by puretone audiometry).
Exclusion criteria
(1) Patients with systemic diseases and other comorbid conditions.
(2) Patients with post operative residual and reccurent perforations of tympanic membrane.
(3) CSOM patients with ossicular chain abnormalities.
(4) Patients with sensorineural hearing loss assessed with the help of Pure tone Audiometry.
(5) Patients with secondary cholesteatoma and granulation tissue in middle ear.
(6) Pregnant females.
Technique
Post aural approach: The postauricular technique is the most commonly performed approach. It was performed with the use of operating microscope.
The basic steps was as follows: The ear canal was suction cleaned and prepared with betadine. Radial canal incisions were made and the canal was packed with cotton soaked in epinephrine.
A postauricular incision was marked 5mm posterior to the auricular crease in a curvilinear fashion, extending them the temporal line to the mastoid tip. The incision was injected with 2% lidocaine with 1:100,000 epinephrine. The incision was carried down through the skin and subcutaneous tissue with care not to enter the ear canal. When the temporalis fascia was reached, a graft was harvested using a Freer elevator and scissors.
A periosteal incision was made and the periosteum raised into the lateral ear canal until the canal incisions was reached. The cotton in the ear canal was removed.
A ribbon gauge was inserted to retract the lateral canal and auricle anteriorly. Mollison self-retaining retractor was used to provide further exposure. The perforation was visualized and margins of the perforation freshened by using sickle knife.
The tympanomeatal flap was raised medially and the middle ear is entered. The integrity and mobility of the ossicular chain was assessed.
The perforation was grafted with the harvested temporalis fascia by underlay technique and the tympanomeatal flap was reposited with gelfoam layered lateral to the grafted membrane. The postauricular incision was closed in layers. The remainder of the ear canal was packed with gelfoam and antibiotic ointment. A pressure dressing was applied to prevent a postauricular hematoma.
Permeatal Sandwich Technique
The permeatal approach, also called as transcanal approach is a procedure which is associated with minimal tissue trauma and is a type of minimal invasive route for tympanoplasty. With the use of endoscopes this approach has become a preferred approach for the procedure. This technique can be challenging for significantly narrow or stenotic ear canals, or individuals with a significant anterior canal bulge. Inspecting the external auditory canal is required to assess that at least a 5mm speculum can be placed in it. Canalplasty can be used to improve visualization if limited. The steps of the surgery are as follows:
The ear canal was suction cleaned and prepared with betadiene. The temporalis fascia graft was harvested through a small incision (5mm to 1cm) in the supra auricular region above the hairline.
The external auditory canal was injected with 2% lidocaine with 1:100,000 epinephrine, primarily for vasoconstriction to optimize visualization during the procedure. In this technique the tympanomeatal flap was not elevated. The perforation in the tympanic membrane was visualized through the External Auditory Canal with the help of 2.7 mm Otoendoscope,
The margins of the perforation were freshened. The middle ear and ossicles were inspected and ossicular continuity and mobility was assessed. Middle ear disease (granulation tissue, tympanosclerosis, adhesions) were completely removed. Ossicular reconstruction was done wherever necessary, elevating the tympanic membrane remnant off the long process of the malleus was done with a sickle knife as this allows closer inspection of the ossicles and better placement of the graft.
The middle ear was packed with Gelfoam soaked in antibiotic ear drops, the graft was trimmed to the size to adequately cover the entire defect. The graft was placed under the freshened margins of the perforation and spread over the medicated gelfoam placed in the middle ear. A layer of medicated gelfoam was placed lateral to “Sandwich” the graft; external auditory canal was packed with antibiotic applied cotton wick for 24 hours.
Results
The data was compiled and statistical comparison was made using chi square test with the help of open EPI Info Software available at Centers for Disease Control and Prevention website.
Patient selection was made on the diagnosis of CSOM and the size of the perforation, the patients were randomly distributed confirming almost equal distribution. A total of 100 patients were included in the study and their distribution on the basis of size of perforation has been summarized in [Table/Fig-1].
Distribution on the basis of size of perforation.
| Type of perforation | Permeatal Sandwhich Technique (n= 52) | Postaural Underlay (n=48) |
|---|
| Large central | 22 | 21 |
| Moderate central | 19 | 17 |
| Small | 11 | 10 |
The graft take up was assessed at the end of 21 days of postoperative period and out of 22 patients having large perforation, 19 grafts were taken up in patients who had undergone Permeatal Sandwich technique compared to 11 out of 21 patients who had undergone Postaural Undelay technique rendering a p-value of 0.021 using chi-square test. Similarly, in cases of moderate central perforation, 18 out of 19 were successful by Permeatal Sandwich technique compared to 11 out of 17 by Postaural Underlay technique, rendering a p-value of 0.036. In case of patients having Small Central perforation, no significant difference was seen by either technique, rendering a p-value of 0.476 shown in [Table/Fig-2]. The overall graft take up was 92.3% in cases of Permeatal Sandwich technique as compared to 64.58% in case of postaural Underlay technique with majority of the failures in the large central perforation group.
There was a marked difference in the complications associated with Permeatal Sandwich technique and postaural underlay technique, with only 2 cases in Permeatal Sandwich Technique compared to 25 cases in Postaural Underlay technique rendering a highly significant p-value 0f 0.000000348 summarized in [Table/Fig-3].
| Type of perforation | Permeatal Sandwhich technique (n= 52) | Postaural underlay (n=48) | |
|---|
| Large Central | 19 (n=22) | 11 (n=21) | p = 0.021 |
| Moderate Central | 18 (n=19) | 11 (n=17) | p = 0.036 |
| Small | 11 (n=11) | 9 (n=10) | p = 0.476 |
| Complication | Permeatal Sandwich Technique (n=52) | Postaural Underlay (n=48) | |
|---|
| Otalgia | 1 | 10 | |
| Post aural wound Infection | 0 | 5 | p = 0.000000348 |
| External Otitis | 1 | 5 | |
| External Auditory Canal Stenosis | 0 | 2 | |
| Vestibular Symptoms | 0 | 3 | |
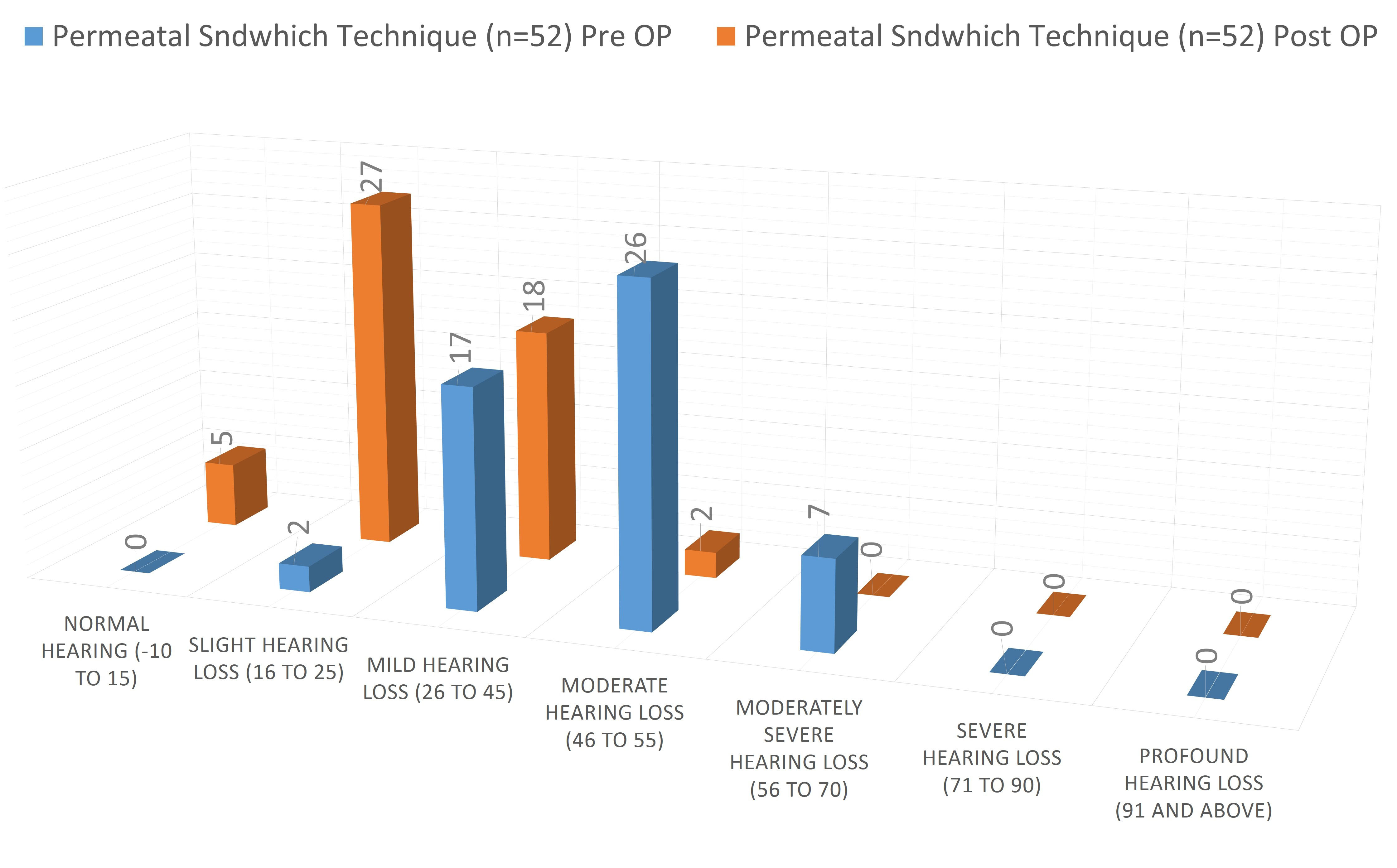
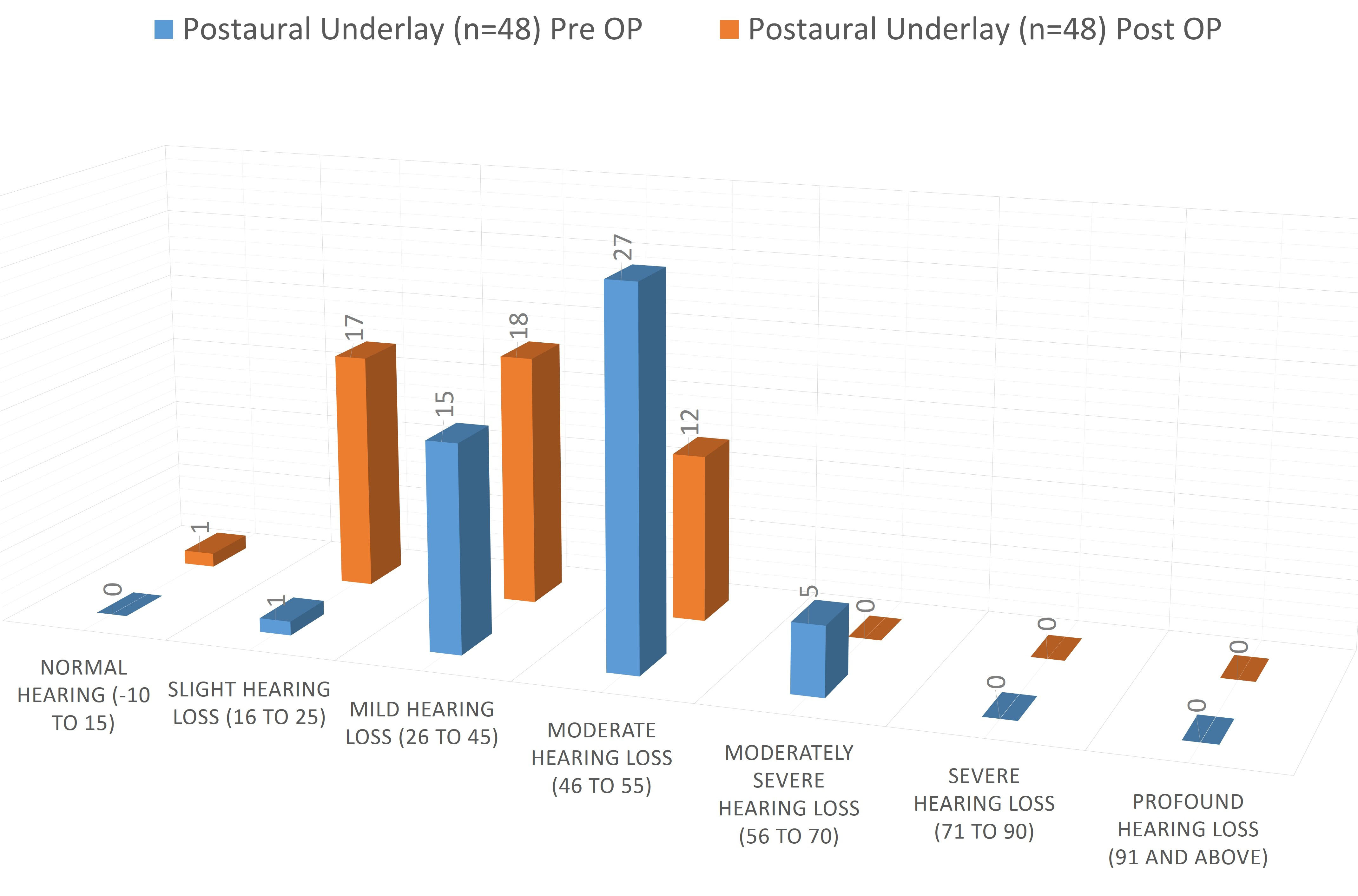
Assessment of hearing loss was done by using average of Hearing Threshold Level obtained by puretone audiometry at 500 Hz, 1,000 Hz and 2,000 Hz. Hearing loss classification accepted by Government of India was considered and distribution of patients was done accordingly with the post-op assessment done after 21 days of surgery which is depicted in [Table/Fig-4]. Majority of the patients in the followup period improved to slight hearing loss in case of Permeatal Sandwich Technique compared to majority having Mild hearing loss in case of Postaural Underlay Technique as shown in [Table/Fig-4] and depicted in [Table/Fig-5,6].
Post-op Assessment of Hearing.
| Hearing Loss | Permeatal Sndwhich Technique (n=52) | Postaural Underlay (n=48) |
|---|
| Pre OP | Post OP | Pre OP | Post OP |
|---|
| Normal hearing (-10 to 15) | 0 | 5 | 0 | 1 |
| Slight Hearing Loss (16 to 25) | 2 | 27 | 1 | 17 |
| Mild Hearing Loss (26 to 45) | 17 | 18 | 15 | 18 |
| Moderate Hearing Loss (46 to 55) | 26 | 2 | 27 | 12 |
| Moderately Severe Hearing Loss (56 to 70) | 7 | 0 | 5 | 0 |
| Severe Hearing Loss (71 to 90) | 0 | 0 | 0 | 0 |
| Profound Hearing Loss (91 and above) | 0 | 0 | 0 | 0 |
Preoperative and postoperative improvement in hearing in permeatal sandwich technique.
Preoperative and postoperative improvement in hearing in postaural underlay technique.
Discussion
Tympanoplasty is a surgical procedure defined as reconstruction of the hearing mechanism with reconstruction of tympanic membrane. Various approaches have been described but with the advent of otoendoscopes the surgery has become quite simplified.
The things to be considered which might have resulted in the difference in results between the two techniques is, first and foremost its tissue trauma which is much more in postaural approach compared to permeatal approach. Secondly handling of the tympanomeatal flap by elevating it from the bony external auditory canal also leads to edema and delayed post-operative healing which is prevented in permeatal technique. Lastly, the preservation of vascular strip comes into consideration which is not affected during the permeatal technique but there are chances of it getting damaged while raising the tympanomeatal flap, these all factors lead to more complications and affect wound healing.
During the initial post-operative period the graft is held in place by the fibrin net formed by the blood clot from the freshened margins of the tympanic membrane. Later on, there is epithelization and also vascularization of the graft material. In the permeatal technique there is preservation of the blood supply of the tympanic membrane in the whole circumference which is affected in post aural technique hence, affecting the graft take up.
Many studies have considered the comparison of postaural underlay grafting with permeatal endoscopic technique. The advantages of the postauricular microscopic approach is bimanual surgical handling and binocular visualization, but the disadvantage of microscopy is that the field of view has to be frequently changed for better visualization of different areas which needs the patient’s head to be manipulated or the microscope has to be repeatedly mobilized. Endoscopic surgery, has the limitation that it is based on a two dimensional visualization of images on the monitor and because of this depth perception becomes difficult [17]. But, a full HD camera system provides much better visualization of endoscopic views and has greatly minimized this drawback. Another drawback with an endoscopic approach is the need for “one-handed” surgery which can also be rectified with the help of trained assistant or endoscope holders. Yadav et al., have emphasized that in the repair of the tympanic membrane perforation done with the help of permeatal endoscopic technique there is no possibility of an iatrogenic cholesteatoma formation as compared to the conventional myringoplasty done with postaural technique [18].
Usami et al., reported on 22 myringoplasty patients treated with endoscopic assistance with a follow-up time of 24.5 months. The rate of perforation closure was 81.8% and improvement in ABG after surgery was 14.8 dB [19]. Karhketo et al., reviewed the records of 29 myringoplasty patients treated with the aid of rigid otoendoscopes with a follow-up time of one year. The rate of perforation closure was 80% and improvement in ABG after surgery was 7 dB [20].
In our study, we got an overall graft take up of 92.3% by Permeatal Sandwich technique compared to 64.58 % by Postaural underlay technique with majority of the patients improving to the range of 16 – 25 dB in Permeatal Sandwich technique and to the to the range of 26 – 45 dB by postaural Underlay technique.
Raj A. emphasizes that with angled endoscopes, it is possible to visualize other structures like round window niche, eustachian tube orifice, incudo-stapedial joint etc. that are difficult to observe through the operating microscope [21]. A comparative study conducted by Thirumaran NS, concluded that there is 93% graft take up rate by endoscopic permeatal approach compared to 91% graft take up rate by post aural approach [22]. Mohindra S. et al., did 49 cases of myringoplasty and 6 cases of ossiculoplasties through the transcanal route using rigid endoscopes. The success rate regarding perforation closure was 91.5% and average air bone gap improvement was 22.24 dB in the myringoplasty groups [17]. Ahmed ELGuindy (Tanta, Egypt) has evaluated the role of the rigid endoscope in the management of 36 cases of dry central perforation of the tympanic membrane. The graft uptake rate was 91.7 percent and air bone gap was closed to less than 10dB in 83.3 percent [23].
Conclusion
With the use of otoendoscopes one can achieve better visualization which will help in better assessment of middle ear structures and the disease. The permeatal approach provides minimal invasive route for the surgery resulting in faster recovery and much less complications arising out of tissue trauma by postaural underlay technique. The complications when compared are much less in Permeatal Sandwich tympanoplasty compared to postaural underlay technique which are directly related to better visualization and minimal tissue trauma.
The authors want to emphasize that the Permeatal Sandwich technique with the help of Otoendoscope provides better results and also help in better demonstration of the procedure to the students. The authors do not totally cast away the operating microscope, as it is required then the external canal is narrow or too much curved and also when mastoids are to be explored.