Acute Urinary Retention due to Primary Pelvic Hydatid Cyst: A Rare Case Report and Literature Review
Santanu Sarkar1, Priyanka Sanyal2, Mohan Kumar Das3, Sandeep Kumar4, Soumyajyoti Panja5
1 Assistant Professor, Department of General Surgery, Burdwan Medical College & Hospital. Burdwan, West Bengal, India.
2 PG Resident, Department of Obstetrics and Gynaecology, NRS Medical College & Hospital, Kolkata, West Bengal, India.
3 Assistant Professor, Department of General Surgery, Burdwan Medical College & Hospital, Burdwan, West Bengal, India.
4 PG Resident, Department of General Surgery, Burdwan Medical College & Hospital, Burdwan, West Bengal, India.
5 PG Resident, Department of General Surgery, Burdwan Medical College & Hospital, Burdwan, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Santanu Sarkar, 1/3/1 C Ramlal Agarwala Lane; Sinthee; Kolkata- 700050, West Bengal, India.
E-mail: drsantanu.surg@gmail.com
Causes of urinary retention in old men include benign prostatic hyperplasia, prostatitis, prostate cancer, Scarring of the urethra or bladder neck as a result of injury or surgery, use of certain medicines particularly NSAIDs and opioid analgesics, constipation and neurogenic bladder. When the above common causes are not quite obvious by clinical examination and relevant investigations, then it is necessary to think of other rare diseases. It is with the above in our mind that a case of bladder outflow obstruction due to a large primary retrovesical hydatid cyst is herein reported in a 58-year-old man. Ultrasonography (USG) and Contrast Enhanced Computed Tomography (CECT) scan of the abdomen and pelvis of the patient revealed a large, multilocular, nonenhancing, cystic lesion in the rectovesical pouch having typical cartwheel appearance without any other intraabdominal organ involvement. These typical radiological characteristics led us to suspect the presence of a hydatid cyst. He underwent exploratory laparotomy where cystopericycstectomy was done. Pre-operative and post-operative albendazole prophylaxis was also given. In conclusion, hydatid cyst should always be considered in the differential diagnosis of pelvic cystic masses, specially in endemic regions.
Echinococcal infection, Lower urinary tract symptoms, Rectovesical pouch of douglas
Case Report
A 58-year-old male patient was admitted in surgical ward with retention of urine for the last 16-hours. He had a history of difficulty in passing urine for last three years along with sense of incomplete bladder evacuation and increased frequency for the same duration. Abdominal examination revealed that suprapubic bloating was due to full bladder, which was tender on palpation and dull on percussion. On per rectal examination, a smooth cystic extraluminal mass was felt anteriorly in the rectovesical pouch without any rectal mass or prostatic enlargement. He was immediately catheterised to relieve his discomfort. There was no history of burning micturition, fever or significant weight loss in the recent past. He had no history of surgery, instrumentation or trauma to the lower urinary tract and there was no history of taking regular medicines (like NSAIDs) which can cause bladder outflow obstruction. General physical examination of the patient was unremarkable and examination of the other systems including neurological system was essentially normal. His complete blood count, serum urea, creatinine and electrolytes, liver function tests and urinalysis were essentially normal. Ultrasound examination (USG) revealed a large, encapsulated SOL with both solid and cystic components, measuring 7.8×7.4×7cm in the pelvis, posterior to urinary bladder. On colour flow study no vascularity was seen in the lesion. There was no lesion in the liver or any other abdominal organ, and also no abnormality detected in prostate and seminal vesicles. Contrast enhanced computed tomography (CECT)scan of the abdomen and pelvis revealed a 8.3×8×7.5 cm, well defined, multilocular, non-enhancing lesion having typical cartwheel appearance [Table/Fig-1a] occupying the rectovesical pouch of Douglas pushing the rectum and anal canal backward and urinary bladder forward. Radiological examination of chest was normal. Flexible cystoscopy revealed an impression of the mass on posterior wall of urinary bladder. There were no duplications, ureterocoele or diverticule on intravenous urogram. Provisional diagnosis of primary pelvic hydatid disease was made based on aforesaid findings, but hydatid serology (serum anti-echinococcus granulosus IgG antibody on ELISA) was not suggestive. Albendazole (10mg/kg/day) was given to the patient for a period of 12-weeks but there was no regression in size of the lesion and symptoms persists. Then surgical excision under general anaesthesia was planned. He underwent an exploratory laparotomy for excision of the large retrovesical cyst [Table/Fig-1b]. On laparotomy the pelvic cyst was unroofed after injecting 10% savlon (1.5% cetrimide-0.15% chlorhexidine) inside it and after shielding the surrounded area with savlon soaked mops; a total cysto-percystectomy was done. During the surgery great care was taken to avoid spillage of hydatid fluid into peritoneal cavity and inadvertent injury to bladder, rectum and ureters especially right ureter which was densely adhered to the mass.
(a) CECT showing large cyst in the pelvis with multiple internal septations (honeycomb appearance, marked by white arrow); (b) Intra operative photograph of pelvic hydatid cyst between sigmoid colon and urinary bladder; (c) Numerous daughter cysts within the main large cyst.
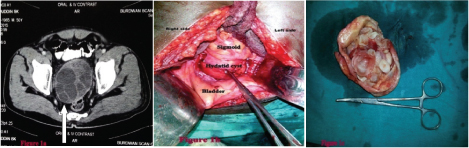
Patient had an uneventful postoperative recovery; urinary catheter was removed on 3rd post-op day. He could void normally from the 4th post-op day. Macroscopical examination of the surgical specimen revealed multiple daughter cysts [Table/Fig-1c] and the histopathological examination confirmed the diagnosis of a hydatid cyst The patient had received albendazole 10 mg/kg/day for 3 months postoperatively and he was free from urinary symptoms for last 12-months follow-up period. Ultrasound examination was done twice in last one year which showed no recurrence.
Discussion
Echinococcus granulosus is a cyclophyllid cestode (tapeworm), which causes hydatid disease. Although E. multilocularis and E. olgarthus can also infect human beings [1,2]. These cestodes have a worldwide distribution but the prevalence is much higher in developing countries including India. The eggs of the parasite released in the stool of the primary hosts (Dogs, wolves, jackals). Human beings (accidental intermediate hosts) may ingest eggs by intimate handling of infected dogs or drinking contaminated water (fecal–oral transmission). The most common sites of involvement are liver (59–75%), followed in frequency by lung (27%), kidney (3%), bone (1–4%), and brain (1-2%). Pelvic echinococcosis is extremely rare, with an incidence of only 0.2–2.25% [3]. Bickers et al., reported the occurrence of pelvic hydatid cyst in only 12 cases out of 532 cases of proven hydatid disease [4]. Clements et al., reported two cases of primary pelvic hydatid cysts in a series of 43 patients with pelvic hydatid cysts [5]. The vast majority of abdominal and pelvic hydatid cysts are considered to be secondary to spontaneous rupture from a primary hepatic focus or it may be due to inadvertent surgical inoculation, but primary pelvic cysts can occur rarely. A hydatid cyst in the pelvic cavity can be considered primary only when no other cysts are present, and in such cases the hydatid embryo gains access to the pelvic cavity either by hematogenous (bypassing the hepatic and pulmonary filters) or by lymphatic route. Connective tissue beneath the pelvic peritoneum is the usual site of origin of pelvic hydatid disease. From here it may spread to the uterus, ovaries, fallopian tubes, urinary bladder or to the rectum after contact [6].
Due to its location in a fixed bony pelvic cavity, it usually presents with pressure symptoms affecting the adjacent abdominal or pelvic organs. An extensive search of english medical databases (Pubmed, google scholar etc.), using key word ‘pelvic hydatid cyst’ revealed some interesting case reports with different clinical presentations which were compiled in [Table/Fig-2] [7–14].
Published case reports of pelvic hydatid cyst with variable clinical presentations.
| Author | Journal & year of publication | Age & sex | Presentating symptoms | Treatment | Outcome(Recurrence) |
|---|
| Gupta Aet al., [7] | J Bone Joint Surg. 1998 | 24[F] | Right gluteal cystic swelling; Numbness and weakness involving the right leg. | Endocystectomy with pericystectomy (partial) for a dumb bell-shaped retroperitoneal cystic mass | — |
| Emir Let al., [8] | Journal of Pediatric Surgery, 2001 | 11[M] | Mass in the right lower abdomen; polydipsia, urinary frequency and secondary nocturnal enuresis. | Endocystectomy with pericystectomy (partial) | — |
| NdaguathaPLWet al., [9] | East African Medical Journal 2003 | 31[M] | Iinability topass urine. | Excision of cyst and post op albendazole. (Inadvertent injury to rectum due to strong adhesions). | No recurrence in 9-year follow up. |
| Adilay Uet al; [10] | Minim Invasive Neurosurg. 2007 | 31[M] | Cauda equina syndrome | Total excision of intraspinal hydatid cyst. | No recurrence in 3-year follow up |
| Parray FQet al., [11] | Case Reports in Surgery (Hindawi Pub Corp 2011) | 23[M] | Dull pain in hypogastric region; frequent micturition. | Excision of cyst, Post op albendazole. | — |
| Nasr Ret al., [12] | Urology Annals. 2014 | 43[M] | Left flank pain and progressive severe obstructive urinary symptoms. | Excision of large retrovesical cyst, along with a left nephroureterectomy. Post op albendazole. | No recurrence in 16-months follow up. |
| BhattacharjeePK et al., [13] | J Med Sci. 2015 | 25[M] | Acute retention of urine and severe agonizing pain radiating along the back of thighs and constipation. | Endocystectomy; pericystectomy(partial) and post op albendazole. | — |
| Sarkar RNet al., [14] | International J of Res in Med. Sciences 2015 | 37[F] | Dull aching pain in lower abdomen;abd distention; breathlessness due to huge right ovarian cystic mass. | Excision of cyst and TAH with BSO. Post op albendazole. | No recurrence in 4-months follow up. |
Age in years; sex: M= Male, F= Female; TAH and BSO=total abdominal hysterectomy and bilateral salpingo-oopherectomy.
The usual differential differential diagnosis of pelvic cysts in an adult male includes seminal vesicle cyst, mullerian duct cyst, ejaculatory duct cyst, prostatic cyst or abscess, bladder diverticulum, ureterocele, Tailgut cysts or retrorectal cystic hamartomas, mesenteric cysts, colonic lymphatic cysts, intestinal duplications, ancient schwannoma and other cystic intrapelvic neoplasms [15]. Even in an endemic country, retrovesical space is an extremely rare site for a hydatid cyst [16]. Ultrasonography is the preferred first-line imaging. The classification proposed by Gharbi et al., for liver hydatid disease based on USG appearance, can be adopted for other locations also. Type I appears cystic and unilocular. Type II is a fluid filled with a floating membrane (the water lily sign). Type III has a typical honeycomb appearance. Type IV is a heterogeneous mass, and Type V is a calcified lesion [17]. CECT provides the exact morphology of the cyst and helps in differentiating other causes of pelvic cysts and hydatid disease in other parts of the abdomen [18]. Serological tests may help in confirming the diagnosis. Gold standard treatment for hydatid cyst is surgery, either conventional open cysto-peicystectomy or by laparoscopic surgery [19]. Percutaneous drainage can be done unilocular cysts(Gharbi type 1 and type 2 cysts). Medical treatment with albendazole before and after surgery reduces morbidity and chances of recurrence [20]. Treatment decision should be individualized for each patient, considering the number of cysts, it’s location, Gharbi classification and patients factors.
Conclusion
Primary pelvic hydatid cyst is a rare entity, albeit it must be considered while making the differential diagnosis of cystic masses in the pelvis, especially in endemic areas. Retrovesical hydatid cysts may have varied and non-specific presentation. USG and CECT both are excellent imaging modalities for the detection of hydatid cysts. The treatment of choice for pelvic hydatid cyst is principally a careful and complete surgical excision, which can be achieved either by open or laparoscopic surgery. Sometimes these large cysts may densely adherent to the neighbouring structures, where complete surgical extirpation is hazardous. In such cases Endocystectomy with partial pericystectomy can be done avoiding any intraperitoneal spillage.
List of Abbreviations Used
NSAIDs: Nonsteroidal anti-inflammatory drugs.
SOL:Space-occupying lesion.
USG: Ultrasonography.
CECT: Contrast enhanced computed tomography.
ELISA: Enzyme linked immunosorbent assays.
TAH & BSO: Total abdominal hysterectomy and bilateral salpingo-oopherectomy.
Age in years; sex: M= Male, F= Female; TAH and BSO=total abdominal hysterectomy and bilateral salpingo-oopherectomy.
[1]. Yuksel M, Demirpolat G, Sever A, Bakaris S, Bulbuloglu E, Elmas N, Hydatid disease involving some rare locations in the body: a pictorial essayThe Korean Journal of Radiology 2007 8(6):531-40. [Google Scholar]
[2]. Khuroo MS, Hydatid disease: Current status and recent advancesAnn Saudi Med 2002 22:56-64. [Google Scholar]
[3]. Perigela HC, Reddy MK, Prasad BV, Narahari J, Giant pelvic hydatid cystJNTR Univ Health Sci 2013 2:218-21. [Google Scholar]
[4]. Bickers WM, Hydatid disease of the female pelvisAm J Obstet Gynecol 1970 107:477-83. [Google Scholar]
[5]. Clements R, Bowyer FM, Hydatid disease of the pelvisClin Radiol 1986 37:375-77. [Google Scholar]
[6]. Salvaggi FP, Fabiano G, Santa Croce S, Tragicante A, A retrovesical echinococcal cyst. Unusual cause of urinary retentionEur J Urol 1978 4:60-62. [Google Scholar]
[7]. Gupta A, Kakkar A, Chadha M, Sathaye CB, A primary intrapelvic hydatid cyst presenting with foot drop and a gluteal swelling: a case reportJ Bone Joint Surg Br 1998 80(6):1037-39. [Google Scholar]
[8]. Emir L, Germiyanoglu C, Lokumcu A, Erol D, Retrovesical Echinococcal Cyst Causing Renal Failure and Nocturnal Enuresis in a ChildJ Pediatr Surg 2001 36(7):E14 [Google Scholar]
[9]. Ndaguatha PLW, Unusual bladder outflow obstruction: Case reportEast African Medical Journal 2003 80(7):388-90. [Google Scholar]
[10]. Adilay U, Tugcu B, Gunes M, Günaldi O, Gunal M, Eseoglu M, Cauda equina syndrome caused by primary lumbosacral and pelvic hydatid cyst: a case reportMinim Invasive Neurosurg 2007 50(5):292-95. [Google Scholar]
[11]. Parray FQ, Wani SN, Bazaz S, Khan SR, Malik NS, Primary Pelvic Hydatid Cyst: A Case ReportCase Reports in Surgery 2011 2011:809387doi:10.1155/2011/809387 [Google Scholar]
[12]. Nasr R, Saad GA, Shahait M, Khater N, Retrovesical hydatid cyst presenting with urinary retention and left kidney atrophyUrology Annals 2014 6(1):68-70. [Google Scholar]
[13]. Bhattacharjee PK, Halder SK, Chakraborty S, Mukerjee A, Singh R, Pelvic hydatid cyst: A rare case reportJ Med Sci 2015 35:122-24. [Google Scholar]
[14]. Sarkar RN, Vani I, Bhagya Lakshmi A, Radha T, Extensive pelvic hydatid disease mimicking ovarian malignant tumourInt J Res Med Sci 2015 3:980-83. [Google Scholar]
[15]. Ercil H, Gurlen G, Sener NC, Altunkol A, Kuyucu F, Evliyaoglu Y, A rare cause of lower urinary tract symptoms: retrovesical hydatid cystJ Pak Med Assoc 2014 64(9):1087-89. [Google Scholar]
[16]. Devaraju S, Nerli RB, Hiremath MB, A Large Mullerian Duct Cyst Presenting as an Abdominal Mass With Ipsilateral Renal Agenesis: An Unusual PresentationNephro Urol Mon 2012 4(4):640-43. [Google Scholar]
[17]. Gharbi HA, Hassine W, Brauner MW, Dupuch K, Ultrasound examination of hydatic liverRadiology 1981 139:453-59. [Google Scholar]
[18]. Halefoglu AM, Yasar A, Huge Retrovesical Hydatid Cyst with Pelvic Localization as the Primary Site: A Case ReportActa Radiologica 2007 48(8):918-20. [Google Scholar]
[19]. Subramaniam B, Abrol N, Kumar R, Laparoscopic Palanivelu-hydatid-system aided management of retrovesical hydatid cystIndian J Urol 2013 29(1):59-60. [Google Scholar]
[20]. Chai J, Menghebat Jiao W, Sun D, Liang B, Shi J, Clinical efficacy of albendazole emulsion in treatment of 212 cases of liver cystic hydatidosisChin Med J 2002 115:1809-13. [Google Scholar]