Pseudoexfoliation (PXE) is an age related disease was first described by Lindberg in 1917 [1]. The complete description of PXE was made by a Swiss Ophthalmologist Alfred Vogt [2]. PXE is a genetically inherited condition affecting elderly aged over 50 years. The reported prevalence rate of PXE varies from as low as 0.4 % among Chinese population and to as high as 6.45% in Pakistani population [3–5]. A prevalence of 3.8% is reported in rural South Indian population [4].
Cataract surgery on eyes with PXE has difficulties related to altered structures due to PXE material, hence, susceptible for increased risk of surgical complications like posterior capsular rupture, zonular dialysis, anterior chamber hyphema and vitreous loss. According to Scorolli et al., intraoperative complications are 5 times greater compared to normal eyes [6].
Proper workup of all cases of PXE with a detailed examination on slit lamp both before and after pupillary dilatation is mandatory. Thus, a thorough pre-operative workup can help us to choose appropriate surgical procedure along with the need for additional Accessories like iris hooks, capsular tension rings, iris clip or scleral fixated IOLs may need to be kept ready.
The present study was concerned mainly with perioperative complications encountered during and after cataract surgery in patients with PXE. Proper preoperative workup can help us anticipate potential intraoperative complications and we can plan the surgical procedure to reduce risk of complications to achieve the best postoperative visual outcomes.
Materials and Methods
This interventional observation study was done on 50 patients diagnosed with both cataract and PXE who were admitted to the Ophthalmology Department of MS Ramaiah Medical College and Memorial Hospital, Bangalore from June 2012 to September 2014. All patients were evaluated with a slit-lamp before and after dilatation to diagnose PXE to look for white grey material on the anterior lens capsule and pupillary area.
Patients aged more than of 50 years belonging to either sex diagnosed with cataract and PXE on the basis of slit lamp examination before and after pupillary dilatation were included in the study.
Patients less than 50 years of age, with previous history of trauma, complicated cataract, ocular surgeries, true exfoliation and presence any systemic complications like uncontrolled diabetics, cardiovascular disease or stroke were excluded.
Institutional ethics committee clearance was obtained and an informed consent was obtained from the patients.
Fifty patients were admitted a day prior to surgery for preoperative workup. All patients underwent a complete ophthalmic examination which included Visual acuity testing using Snellen’s chart, Goldman applanation tonometry for intraocular pressure. Detailed slit lamp examination was done to look for pseudoexfoliative deposits on the cornea, iris and pupillary margin and after dilatation, on the anterior capsule of the lens. Ultrasound pachymetry using Axis II PR, Quantel Medical was done for measuring corneal thickness. Corrected intraocular pressures for corneal thickness were documented finally. Angle evaluation was done using Goldmen three mirror gonioscope and graded by Shaffer’s grading system [7].
Patients underwent cataract surgery with either manual small incision cataract surgery or phacoemulsification. All patients were operated by consultants.
Patients who had good pupillary dilatation and nuclear sclerosis between grade 2-3 according to LOCS [8,9] were selected for phacoemulsification, rest of the patients underwent manual SICS.
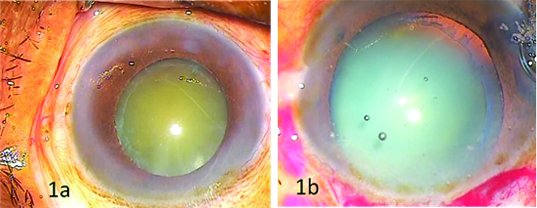
Preoperatively pupillary diameter after dilatation was graded as follows poor (2-4 mm), moderate (5-6 mm) and good (7-9 mm or more) [Table/Fig-1a,b]. This grading of pupillary dilation was similar to one used by Pranathi K et al., in their study [10].
(a) Moderately dilated pupil with white deposits at margin (b) Capsular membrane line deposits.
Prophylactic antibiotics drops moxifloxacin 0.5% eye drops started one day before surgery. Patients were dilated with tropicamide 0.5% solution and non-steroidal anti-inflammatory drops flurbiprofen sodium 0.03% was used 3 times every 15 minutes to maintain the dilatation.
Surgical Procedure
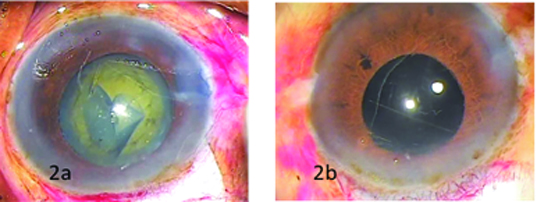
After peri-bulbar block with 5 ml of 2% xylocaine and 5 ml of 0.5% bupivacaine with 150 units/ml of hyaluronidase. Povidine-iodine 5% was instilled into the conjunctival sac. For SICS a fornix base conjunctival flap was made, scleral incision was made with bard parker knife with 15 no. blade temporally or supero-temporally and sclerocorneal tunnel was constructed with crescent. Continuous curvilinear capsulorhexis (CCC) aimed at 5mm to 5.5 mm [Table/Fig-2a] was done using the needle cystitome and completed using Utrata’scapsulorhexis forceps or microrhexis forceps if necessary. A thorough hydrodissection was performed to separate cortex from nucleus. Nucleus was delivered by visco expression. Irrigation and aspiration was done with Simcoe’s two way irrigation and aspiration cannula. Rigid, single piece, biconvex, polymethyl meth acrylate posterior chamber intraocular lens (IOLs) with optic diameter of 5.25 mm was implanted in bag [Table/Fig-2b].
(a) Continuous Curvilinear Capsulorhexis (b) In bag Intraocular Lens.
In patients who were operated by phacoemulsification, a temporal clear corneal incision was made and nucleus was emulsified by stop and chop technique, foldable IOL was placed in bag. Postoperatively, patients were put on topical antibiotics and steroids with a tapering dose over 4-6 weeks depending upon the postoperative inflammation. Patients were followed on the postoperative day 1, day 14 and at 6 weeks to evaluate intraocular pressure, presence of intraocular inflammation, intraocular decentration and corneal endothelial decompensation.
Data was analysed using statistical package for social sciences version 15.0 (IBM).
Results
Out of 50 patients, 32 were males and 18 were females. The mean age was 70 (range 50- 80yrs). Out of the 50 patients, 10 underwent phacoemulsification surgery. Pre-operatively visual acuity: 50% had counting fingers, 16% better than 6/60, 20% hand movements, 14% only perception of light [Table/Fig-3].
Preoperative visual acuity analysis.
| Visual actuity | Pre-operative | Percentage |
|---|
| 6/60-6/12 | 8 | 16% |
| CF | 25 | 50% |
| HM | 10 | 20% |
| PL/PR | 7 | 14% |
A total of 5 patients were diagnosed has pseudo exfoliative glaucoma, preoperative IOP- ranged from 10 -50 mmHg with mean of 14 mmHg. 45 patients had IOP within normal levels (<21mm Hg), 2 patients had IOP more than 22 mmHg but less than 30 mmHg, they underwent medical management. Three patients under went combined procedure cataract with trabeculectomy as they had IOP greater than 30 mmHg along with optic neuropathy [Table/Fig-4].
| Intraocular pressure mm of Hg | No. of Patients | Medical management | Trabeculectomy |
|---|
| 10-19 | 45 | | |
| 20-29 | 2 | 1 | 1 |
| 30-50 | 3 | 1 | 2 |
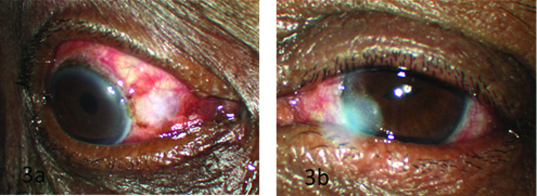
Forty patients (80%) underwent SICS, out of which 3 patients underwent a combined procedure along with SICS., 10 patients (20%) underwent Phacoemulsification, 37 eyes of 40 SICS procedures had a PMMA rigid IOL implant whereas 2 patients underwent a posterior iris clip lens [Table/Fig-5a,5b] and one patient underwent a secondary Scleral fixated IOL. Out of 10 eyes who had undergone phacoemulsification in 9 cases a foldable IOL was implanted and 1 patient had a scleral fixated IOL.
(a) Trabeculectomy. (b) Iris claw IOL.
Five patients had small pupil i.e. less than 4 mm. Iris hooks were used for 3 of them and in 2 patients stretch pupilloplasty was done. Corneal thickness analysis revealed 82% of patients had corneal thinning less than 535 microns while corneal thickness was within normal range in only 10% of patients with while 8 % had thicker corneas i.e. >565 microns [Table/Fig-6].
Corneal thickness analysis.
| Corneal thickness | In microns | No of case | Percentage |
|---|
| Very thin | <510 | 25 | 50% |
| Thin | <535 | 16 | 32% |
| Average | 540-560 | 5 | 10% |
| Thick | >565 | 3 | 6% |
| Very thick | >600 | 1 | 2% |
Two cases of severe zonular weakness, 1 patient with a dialysis of less than 4 clock hours underwent capsular tension ring while another patient underwent a SFIOL.
The incidence of complications encountered during surgery were [Table/Fig-7] zonular dialysis in 3 patients (6%), posterior capsular rupture in two (4%) and vitreous loss in 3 cases (6%).
| Surgical complication | No of eyes | % |
|---|
| Poorly dilating pupil | 5 | 10 |
| Lens dislocation | nil | |
| Posterior capsule rupture | 2 | 4 |
| Vitreous loss | 3 | 6 |
| Retained lens matter | nil | |
| Decentered IOL | nil | |
| Zonular dialysis | 3 | 6 |
| Post operative hypema | nil | |
Mean postoperative IOP was 12 mmHg. Postoperatively visual acuity was better than 6/12 in 78% (39 eyes) [Table/Fig-8]. Whereas 10% had vision worse then 6/60, due to corneal oedema. Postoperative pachymetry revealed that there was 10 to 15 microns increase in corneal thickness in above cases. We could not do specular microscopy for our patients due to lack of facility.
Post operative visual acuity.
| Visual actuity | No of eyes (n=50) | Percentage (%) |
|---|
| 6/6-6/12 | 39 | 78% |
| 6/18-6/36 | 06 | 12% |
| 6/60 or less | 05 | 10% |
Discussion
PXE syndrome affects mainly the elderly age group of patients who are likely to undergo cataract surgery. Many a time there is a chance to miss these findings when operating in community camp settings. A detailed preoperative evaluation that includes a thorough slit lamp evaluation to specifically look for PXE after dilation of pupil, signs of zonular instability such as lens subluxation, zonular dialysis, iridodonosis or phacodonosis is very essential. Early iridodonesis can be better appreciated prior to pupil dilatation whereas lens capsular deposits, zonular integrity, type of cataract can be evaluated post dilatation [1,11].
Disease is characterised by progressive deposition of abnormal fibrillar extracellular material which was believed to be inflammatory in earlier days, but now it is recognised as protein like material deposited from abnormal basement membrane of epithelial cells. External environmental factors like excess sun exposure has also be implicated for PXE [12].
Histopathologically the material produced by aging epithelial cells of basement membrane from, lens, iris, cilairy body and basement membrane of endothelial cells of iris, trabecular meshwork and conjunctival vessels. This extra-cellular material is nothing but a protein core surrounded by glycoaminoglycans. Similar, material deposition involving skin and visceral organs also were reported suggesting it may be ocular manifestation of a generalized disease [13,14].
In PXE Fibrino-granular material deposited on the lens capsule is more obvious in the pupillary area and pre-equatorial region appearing as a grey membrane like structure. Second most common site is at the pupillary margin seen as a grey dandruff like material associated with pupillary atrophic changes giving a moth eaten appearance on trans illumination. Other sites of ocular deposition are over the iris stoma, corneal endothelium, anterior hyaloid face and zonular fibres.
Although there was a correlation with lesser the AC depth more the complication risk [15], amount of PXE material over zonules showed no correlation with that of zonular weakness [16,17].
Mohammad reported 16% of cases presenting with spontaneous anterior subluxation with PXE [18]. Capsular contraction and fibrosis can continue even postoperatively leading to higher incidence of IOL tilt, posterior capsular opacification rarely spontaneous dislocation of intraocular lens has been reported [19,20].
In our study among 50 patients, 32 (64%) were male and 18 (36%) were female. A male preponderance was found in our study similar to a study by Abid Naseem et al., [21]. While Arvind et al., reported no sex predilection, Avramides et al., have reported a female preponderance in their study [4,22].
Of the 50 patients studied, 80% had nuclear sclerosis. Most of them had grade 2 to 3, 20% had cortical cataract and both changes were seen in 30% of cases. Similar to our finding a strong association between PXE and nuclear cataract was found in various studies [15,23].
Various studies have shown that the corneal thickness measurement in PXE cases is below normal in most cases. This may lead to underestimation of the IOP [24,25]. In our case series 82% of cases showed corneal thinning (<535microns), 25cases (50%) very thin cornea and 16cases (32%) with thin cornea. In only 5 cases (10%) it was within normal range and while 8% had thick cornea [Table/Fig-6]. Hence, it is very important to do pachymetry in all cases of PXE to prevent underestimating IOP.
Patients with PXE have a high prevalence of rigid pupil with poor dilatation. Pupillary dilation of less than 7 mm is reported to be as high as 94.1% [11]. While Alfaiate et al., reported a prevalence of 48.4%, in our case series 64 %(32 cases) had dilatation less than 7mm [26]. In the 27 eyes with poorly dilating pupils (5-7mm) intraoperative bimanual stretching was performed with and along with use of cohesive viscoelastic. Whereas, in 5 patients with very poor dilatation (2-4mm) required iris hooks and retractors for pupillary dilatation.
Intraoperatively, it is a challenging task to make adequate capsular rhexis of 5.0 to 5.5 mm in diameter in PXE eyes due to co-existing poor pupillary dilatation, thin fragile capsule and zonular weakness. Sometimes there is also a presence of false capsule due to deposits of exfoliative material. We were able to achieve a complete rhexis in 80% (40cases) of patients. In 20% (10 cases) there was difficulty to perform rhexis as 2 cases had phacodonesis with weak zonules in these patients a semi-circular opening of capsule was done. In 6 cases of hypermature cataract with thin capsule with calcififcation and poor capsular support (shrunken nucleus) capsular opening was performed using vannas scissor. In two cases with very thin capsule and large nucleus a loss of rhexis was encountered while attempting a larger rhexis. It is important to achieve a capsular opening of adequate size as smaller rhexis increases the risk of intraoperative and postoperative complications like excessive zonular stress, difficulty in phacoemulsification and an increased risk of anterior capsular tear by second instrument. Postoperatively there is a higher incidence of capsular phimosis.
Presence of severe zonular weakness can lead to dreaded complications like lens subluxation [19] and vitreous loss. Postoperatively there is a higher incidence of capsular phimosis [16,27] postoperative iritis and corneal oedema associated with excessive intraoperative manipulations due to small pupil and unhealthy endothelium.
In our study, the rate of vitreous loss was 6%, while other studies have reported rates varying from 0% to 11% [17,23]. Other complications, we encountered are small rigid pupil in 5 eyes (10%), posterior capsular rupture in 2(4%) and zonular dialysis 3 eyes (6%). In our study, we used capsular tension rings in 2 cases with zonular dialysis to prevent postoperative IOL decentration.
Postoperatively, 17(34%) cases had significant corneal odema. A similar experience has been reported by Dwivedi NR et al., [28]. Reasons for corneal oedema include prolonged surgical time due to small pupil, retained lens matter, poor endothelial function, Postoperative iritis, retained viscoelastics leading to temporary rise in intraocular pressure.
Thorough, preoperative workup regarding zonular integrity, papillary dilatation, and intraocular pressure helps to decrease intra and postoperative complication in these patients. Surgical planning includes choice of viscoelastic, pupil expansion devices, capsular tension rings, choice of surgery and having an IOL inventory of iris claw or scleral fixated IOLs helps to increase the safety margin while operating on these complicated cases.
Limitation
The main limitations of our study include small sample size and shorter follow-up. Long term follow-up is needed to comment on IOP, capsular contracture and IOLs decentration.
Conclusion
Although cataract with pseudoexfoliation is a challenging scenario to operate upon, a proper pre-operative assessment and case based management plan is required as the magnitude of problems may vary from patient to patient. It is possible to achieve good results in most patients by taking adequate preoperative precautions and readiness to handle intraoperative complications. Affordable and easy access to surgical accessories like iris claw, scleral fixated IOLs, capsular tension rings, iris retractors and hooks have helped us to manage intraoperative complications appropriately with acceptable visual outcomes.