The cornea is the transparent avascular tissue of the eye, for which its transparency is essential for optimal clarity and vision. The cornea is an immune-privileged site; i.e. the immune response to antigens is absent in order to protect this highly organized structure of the eye. The corneal avascularity is considered as corneal angiogenic privilege [1].
Neovascular and infectious diseases of the cornea and other parts of the eye represent a major public health burden. Although the exact incidence and prevalence rates of Corneal Neovascularization (CNV) globally is still unknown, the incidence rate was estimated at 1.4 million patients per year based on an extrapolation of the 4.14% prevalence rate at the Massachusetts Eye and Ear Infirmary in1998 [2]. Under physiological conditions, the corneal avascularity requires low levels of angiogenic factors and high levels of anti-angiogenic factors, any disturbance in the balance between which results in new vessel formation i.e., corneal neovascularization. This phenomenon occurs in a variety of pathological conditions, such as limbal stem cell deficiency [3], hypoxia, chemical burns, ischemia, inflammation, infection and trauma [4].
The new blood vessels thus formed are immature leading to lipid exudation, persistent inflammation and scarring, ultimately posing a threat to corneal transparency and visual acuity and, in patients with corneal grafts, may contribute to rejection [5].
Various methods have been developed and used over years to occlude corneal vessels to avoid above mentioned untoward effects. These include medical treatments; such as, topical steroids [6], nonsteroidal anti-inflammatory drugs [7], cyclosporin A [8] and anti- VEGF agents [3]. Radiation, diathermy [9], conjunctival resection and limbal stem cell transplantation [3] are the invasive methods used.
Due to the untoward effects of corneal neovascularisation like interference with corneal transparency, increasing the risk of graft rejection ultimately resulting in reduction in visual acuity, their is a dire need to treat corneal neovascularisation, laser photocoagulation (first reported in early 1970s in humans) [10] being one of the modality for treating corneal neovascularisation.
In this study, we are evaluating the efficacy and safety profile of laser photocoagulation in treating corneal neovascularisation.
Materials and Methods
A total of 40 eyes of 40 patients of either sex suffering from corneal neovascularistion in quiescent eyes were prospectively evaluated and were treated by frequency doubled Nd:Yag laser after taking informed consent in the Department of Ophthalmology, Maharani Laxmi Bai Medical College, Jhansi (U.P.). The essential inclusion criteria were: 10 years of age or more with superficial and/or deep corneal vascularisation up to two quadrants with healed corneal disease. Patients with active inflammation of the ocular surface, an active corneal stromal infiltrate, a corneal epithelial defect, adherent leucoma, uveitis, raised Intraocular Pressure (IOP), corneal dystrophies, corneal degeneration, any chronic co-morbid eye condition like cataract, glaucoma, diabetic retinopathy, hypertensive retinopathy, etc.
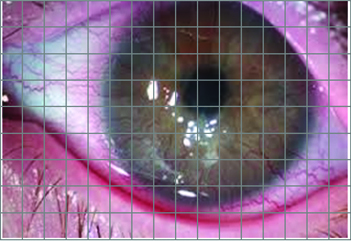
Complete ophthalmic examination of all the patients was done which included recording of the best corrected visual acuity, IOP, extent of corneal opacity and vascularisation. Corneal vascularisation and opacity was measured using retroillumination on Haag Streit Slit lamp (X16 magnifications). To map or record the extent of corneal vascularisation and corneal opacity colour coded grid diagrams (1 mm2 on grid representing 0.2 mm x 0.2 mm of cornea) [Table/Fig-1] and anterior segment photographs were used.
Grid diagram to measure area of corneal neovascularisation.
Laser photocoagulation was done using frequency-doubled Nd:YAG (532 nm) laser and Abraham contact lens. Abraham lense helps in stabilization of the globe, magnification of the corneal vessels and focusing laser energy on the corneal vessels. Laser parameters used were 120-480 mw of power, 50-150μm spot size and 0.05 seconds pulse duration. Laser parameters were set after subjective verification of the diameter and position of corneal vessels. The ocular surface was anaesthetised using topical 4% xylocaine hydrochloride. Patient was positioned properly on the slit lamp. Methylcellulose eye drop was used as a coupling agent between the eye and the Abraham contact lens. The lens was placed on the corneal surface. The slit lamp beam and the red light spot were focused at 30°-45° oblique illumination and X16 magnification on the vessel to be lasered and the laser was applied starting from the limbus towards the paracentral cornea (2-3mm inwards) along the new vessels first and then from limbus towards the periphery. The cessation of blood flow or blanching of the lasered vessel was taken as the end point. We avoided applying laser in the central corneal region to prevent any possible damage in the visual axis and also the central vessels regress on their own because blood supply to them is cut off when the paracentral and peripheral vascularization is effectively photocoagulated. The laser power used starting from minimal i.e., 120 mw, was increased further upto 480 mw depending on the subjective variability of corneal vessels (superficial to deep vessels and from patient to patient). The patients were prescribed topical lubricants four times daily as a placebo and timolol two times daily for one week following laser treatment.
The follow up of the patients was done at first week and then monthly for first 3 months after the last laser treatment. At each follow up, complete ocular assessment was done recording the effect of laser on vessels as complete occlusion, partial occlusion, recanalisation and appearance of shunt vessels on slit lamp biomicroscopy. The vessels with complete cessation of blood flow distal to laser treated vessel or discontinuity of vessel wall at the point of laser treatment was labelled as completely occluded and the vessels with narrowing of the vessel distal to point of laser treatment or partial continuity of distal end with proximal end of treated vessel were categorised as partially occluded. Shunt vessel referred to the appearance of new vessels connecting the proximal and distal end of the occluded vessel.
No intervention was done and no additional treatment was given to avoid any confounding factor or bias. Data analysis was done by Epi Info 7.1.3.0 version. The observations were documented and statistically analysed using the paired t-test.
Results
The age of the patients included in the study ranged from 17 to 70 years with the mean age of 41.32±16.45 years. In our study, out of 40 patients satisfying the inclusion criteria, 27 (67.5%) patients were male and 13 (32.5%) were female, showing male preponderance.
The mean area of corneal vascularisation in patients before laser treatment was 31.93% of the total corneal area; this decreased to 17.62% of the total corneal area at three months follow-up after laser treatment which was statistically significant [Table/Fig-2]. The mean area of corneal opacity in patients included in our study before laser treatment decreased from 30.75% of the total corneal area to 23.74% after three months of the laser treatment [Table/Fig-3].
Mean percentage area of corneal neovascularisation.
| Duration | Mean percentage area of corneal neovascularisation | p-value* | t-test |
|---|
| Pre laser | 31.93% | - | - |
| Post laser 1 week | 20.47% | 0.0001 | 15.90 |
| Post laser 1 month | 20.26% | 0.0001 | 13.54 |
| Post laser 2 month | 18.30% | 0.0001 | 12.79 |
| Post laser 3 month | 17.62% | 0.0001 | 12.72 |
*significant p-value is depicted in bold
Mean percentage area of corneal opacity.
| Duration | Mean percentage area of corneal opacity | p-value* | t-test |
|---|
| Pre laser | 30.75% | | |
| At 1 week | 29.41% | 0.0001 | 12.63 |
| At 1 month | 27.14% | 0.0001 | 15.85 |
| At 2 month | 25.27% | 0.0001 | 15.74 |
| At 3 month | 23.74% | 0.0001 | 16.38 |
*significant p-value depicted in bold
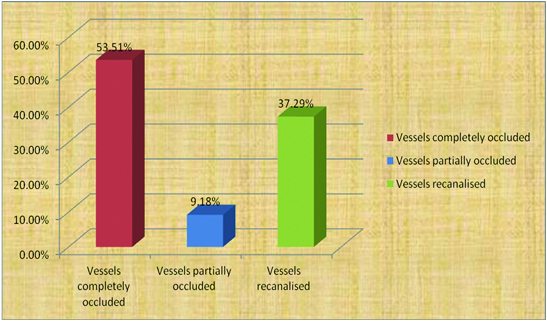
Out of 185 corneal vessels from 40 eyes of 40 patients included in this study, we found that 99 (53.51%) vessels were completely occluded, 17(9.18%) vessels were partially occluded and 69(37.29%) vessels were recanalised at the end of 3 months after laser treatment [Table/Fig-4].
Status of corneal vessels 3 months after laser treatment.
In this study, the mean BCVA increased by 8.21% 3 months after the laser treatment from the baseline value [Table/Fig-5] which was not found to be statistically significant (p=0.5931).
| Duration | † BCVA (Log MAR±SD) Mean | p-value | t-test |
|---|
| Mean | SD |
|---|
| Baseline | 0.73 | 0.24 | - | - |
| At 1 week | 0.73 | 0.24 | - | - |
| At 1 month | 0.71 | 0.20 | 0.4174 | 0.8196 |
| At 2 month | 0.69 | 0.19 | 0.4898 | 0.6972 |
| At 3 month | 0.67 | 0.19 | 0.5931 | 0.5389 |
* significant p-value depicted in bold † BCVA –Best corrected visual acuity
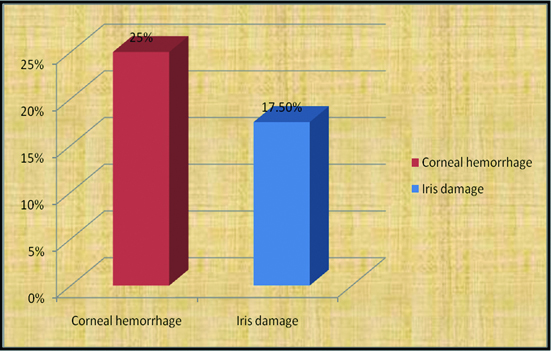
Out of 40 patients included in this study, 17 patients had complications after laser treatment. Amongst them corneal haemorrhage was found to be most frequent occurring in 10(25%) of our patients and the other 7(17.50%) patients having iris damage as a complication [Table/Fig-6]. For the rest 23 patients, the post laser period was satisfactory without any complication.
Complications of yag laser.
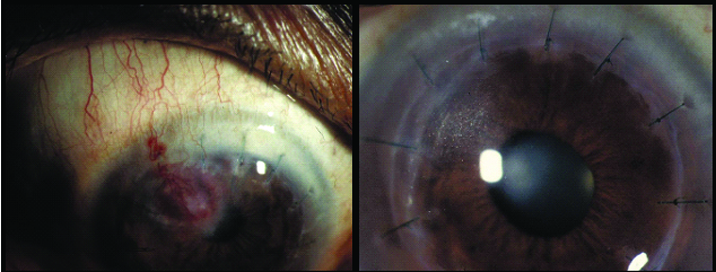
Cornea of a patient before and after laser treatment of corneal neovascularvisation.
Discussion
In our study, Frequency-doubled Nd:YAG (532 nm) laser photocoagulation appeared to be a safe and effective modality for treating corneal vascularisation showing an effective reduction in the area of corneal vascularisation from 31.94% to 17.63% area thus accounting for a percentage decrease of 44.08% in the area of corneal neovascularisation at the end of 3 months follow up after the frequency-doubled Nd:YAG (532 nm) laser treatment which is comparable to 41.2% reduction in mean percentage area of corneal vascularization at three months follow up in the study conducted by Bhatti N et al., and Sharma A et al., with a reduction of 54.15% in percentage area of corneal neovascularisation at 3 months follow-up (p<0.05) [10,11]. In the study by Sharma A and Samal A, topical betamethasone 0.1% drops twice daily for one week after laser therapy was used resulting in higher success rate as topical steroids [11] has additional therapeutic effect on corneal neovascularisation [12].
In the study by Baer and Foster the mean reduction in area of corneal vascularisation was 41% following yellow dye laser treatment at 9.3 months’ follow up [13]. The results of our study with frequency-doubled Nd:YAG (532 nm) are similar.
In the study by Sheppard and Epstein, they reported 7 patients of corneal neovascularization who were treated with argon laser (514 nm) using Dihaematoporphyrin Ether (DHE) showing a reduction of 52.5% in corneal neovascularization at 6 months follow-up. In addition to laser therapy DHE was used as photosensitizer in their study which helps in better visualization and photocoagulation of corneal neovascularisation [14]. Nirankari VS conducted a study on 13 eyes having corneal neovascularisation reporting a reduction of 45.3% in corneal vascularization at 4 months follow-up after argon laser photocoagulation [15].
Corneal Opacity
In the present study, the percentage mean area of corneal opacity was decreased from 30.75 to 23.74% at the end of 3 months accounting for a decrease of 7.01% in the total area of corneal opacity following laser treatment. In the study conducted by Sharma A et al., the mean reduction in the area of corneal opacity was 4.39% following laser treatment at 3 months’ follow-up and three patients had a decrease in the density of lipid exudation and in the area of opacity [11]. Baer and Foster (577 nm laser) reported a mean reduction in the area of corneal opacity by 7% at 9.3 months’ follow-up which is similar to ours [13].
Visual Acquity
Although the increase in mean best corrected visual acuity was statistically insignificant but we observed improvement in visual acuity in 5 out of 40 patients during our study. One patient with best corrected visual acuity of 2/60 before laser improved to best corrected visual acuity of 6/36 and the other improved from 4/60 to 6/24 at the end of 3 months after laser treatment. Two of our patients improved to the best corrected visual acuity of 6/24 from 6/60 at the end of three months. One of our patients had an improvement of two snellen’s lines from 6/36 to 6/18. Increase in visual acuity was an encouraging finding in our study. Visual acuity of rest of the patients was unaltered. In the study of Bhatti N et al., two of their patients with best corrected visual acuity of less than 4/60 improved to the best corrected visual acuity of 6/24 at the end of three months [10]. Sharma A et al., described visual acuity improvement in two patients at 3 months’ follow up. One improved from 6/60 to 6/36 and the other 6/18 to 6/9 [11].
Baer and Foster reported an improvement by 0.7 Snellen lines in visual acuity of five (17.5) patients after 9.3 months’ follow up using yellow dye (577 nm) laser [13].
Sequential Changes in Corneal Blood Vessels
The sequential changes in corneal blood vessels following laser treatment was evaluated which showed that the number of totally occluded corneal vessels increased while most of the partially occluded vessels closed completely during follow-up due to thrombus formation in the lumen of vessels [16]. We found that out of 185 vessels, 99 corneal vessels (53.51%) were completely occluded and 17 (9.19%) were partially occluded after laser treatment at 3 months follow up. The number of occluded vessels increased from 76 at one week to 99 at 3 months follow up. Out of 194 vessels, 80 (41.2%) vessels were completely occluded in study of Bhatti N et al., [10].
In addition, the numbers of recanalised vessels increased from 48 at one week to 69 at 3 months follow up. In this study, 37.29% (69 out of 185 vessels) of corneal vessels were recanalised at the end of 3 months which is much less than 58.8% (114 out of 194 vessels) of recanalised vessels by Bhatti N et al., and comparable to 35.14% recanalised vessels in the study conducted by Sharma A et al., [10,11]. Recanalisation of vessels can occur due to inadequacy of laser on those vessels and relatively deeper situation of few vessels. At the end of 3 months 3 shunt vessels were formed in our study as against the 2 shunt vessels reported by Sharma A et al., in the year 2001 [11].
The complications of laser therapy of vascularised corneal lipid keratopathy include bleeding into lipid keratopathy (corneal haemorrhage), corneal thinning, iris atrophy, crystalline deposits on iris and peaking of pupil following corneal laser therapy [17]. We observed superficial corneal haemorrhage in ten (25%) of our patients. Corneal haemorrhage resolved within one week in all the patients without any additional treatment. Sharma A et al., found corneal haemorrhage in 4 (13%) of their patients which also resolved without any treatment [11]. We also found iris damage in seven (17.5%) of our patients as a complication of laser treatment which is comparable to Bhatti et al., and Epstein and Hendricks who reported iris damage in 16% and 18% of patients [10,18]. Marsh RJ reported iris damage as minor complication [17]. In our study iris damage was associated with slight peaking of pupil in the direction of damaged iris patch. Iris excavation and peaking of pupil were almost imperceptible after six to eight weeks. No other complications such as corneal thinning, descemetocele, and corneal perforation were observed following laser therapy in any of our patients.
Our study demonstrates that frequency-doubled Nd:YAG (532 nm) laser photocoagulation is an effective method of decreasing the area of corneal vascularisation in quiescent eyes without causing any significant serious complications.
Laser photocoagulation is a safe outpatient procedure and can be performed under topical anaesthesia, is simple and well tolerated by the patient. Lack of serious complications makes it an effective alternative to other methods for reducing corneal vascularization in quiescent eyes with vascularised corneal opacities
The power of laser should be adequate enough just to blanch the respective corneal vessel. Use of excess laser power results in increased post laser inflammation thus acting as a stimulus for revascularization. None of the patients had an increase in corneal stromal vascularization immediately after laser treatment or recurrences later.
Therefore, we propose that laser photocoagulation is a valuable adjunctive tool in the treatment of corneal stromal vascularization.
Conclusion
Frequency doubled Nd:yag laser is an effective and safe method for treating corneal neovascularisation.
*significant p-value is depicted in bold
*significant p-value depicted in bold
* significant p-value depicted in bold † BCVA –Best corrected visual acuity