Maxillofacial defects caused due to cancer; trauma or congenital disease demand more exhaustive and high quality prosthetic treatment. Such defects are located in a highly visible body area that is associated with one’s own visage. Any minor alteration in facial appearance hampers the mental health of such patients. An aesthetic maxillofacial prosthesis mitigates many difficulties of the patient and may enhance the quality of life [1,2].
Colour matching to human skin during the process of prosthesis fabrication is often a significant challenge to the Prosthodontists [3]. Among the many global inhabitants, the skin colour of Indians is exclusively identified as an alloyed composition varying from light to dark complexion. Such contradistinction in skin colour occurs due to various reasons like genetics, exposure to sunlight, and/or culture, etc. Though many substances affect the actual skin colour, melanin is considered the most vital colour imparting element. When the melanin content is high, an individual possess dark complexion. People with light skin colour have less melanin content and their skin colour is more determined by the bluish-white connective tissue under the dermis and the haemoglobin circulating in the veins of the dermis [4,5].
Many approaches and techniques have been used to achieve a perfect skin colour match [6]. Despite the various improvements in technology and material science, till now utilization of trial and error method for colour replication is widely used in clinical practice. Employment of objective measures for colour determination with the aid of colorimeters or hand held spectrophotometers have not become conventional in India [7,8]. Skin being a multi layered structure limits the use of such instrumental methods as they consume more time and have minimal precision in colour reproduction [9].
Hence, this study was attempted to fabricate a novel custom made intrinsic silicone shade guide in a manner that is similar to that used for tooth shade matching and to evaluate its reproducibility. Employment of this shade guide comprised of different shades will assist the Prosthodontists to obtain a good intrinsic shade and minimise extrinsic colouration of extra oral prosthesis.
Materials and Methods
An observational cross-sectional analytical study was done by the Department of Prosthodontics, Saveetha Dental College & Hospitals, Chennai, Tamil Nadu, India to evaluate the reproducibility of a novel custom made intrinsic silicone shade guide for Indian population to be used in rehabilitation of maxillofacial defects.
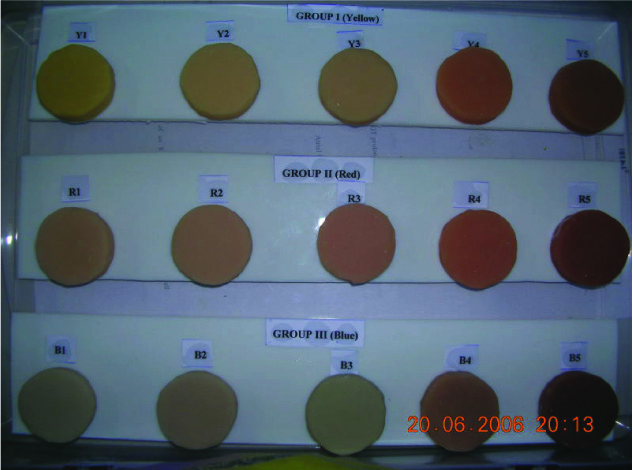
Room temperature vulcanising medical grade silicone (Factor II Inc. A-2186 platinum silicone elastomer, Lakeside, AZ, USA) [Table/Fig-1] was opted as the base material for the shade guide and facial prosthesis because of its documented superiority over conventional acrylic resins and polyvinyl chloride. It has been well documented that very nearly all colours can be matched by merely adjusting the intensities of red, green and blue components of a mixture of coloured light. Spectrophotometric studies of human skin colour enabled to divide the shades based upon hue into the three groups as Group I – Yellow base (Y), Group II – Red base (R) and Group III – Blue base (B) [10]. For the fabrication of shade tabs, each group was further subdivided into five categories (1-5) based upon the value from lighter to darker shades.
Factor II A-2186 Platinum silicone elastomer.

Fabrication of Shade Tabs
A total number of 15 circular shade tabs measuring 2.8cm of 4mm thickness was fabricated initially with modelling wax (Hindustan modelling wax, DPI) [Table/Fig-2]. The wax tabs were invested in dental stone and de waxing was done in a conventional method. Translucent Factor II platinum silicone elastomer was mixed in the ratio of 10:1 by weight with stainless steel spatula. A digital balance (Mettler Toledo precision balance) was used for standardisation of measurements [Table/Fig-3]. Each drop dispensed constituted 0.03gm of measure. Thixotropic agent was added to increase the viscosity of the material. Corresponding intrinsic pigment kit of Factor II material (Functional intrinsic skin kit KT 499 & KT 399) was used for obtaining different shades. As a standard, intrinsic pigments 0.03gm of white (FI-200) and 0.03gm of tan (FI-215) were added to all the tabs. To discriminate the groups into three, 0.03gm of yellow pigment (FI-202) was added to group I, 0.03gm of red pigment (FI- 204) to group II and 0.03gm of blue pigment (FI-203) to group III [Table/Fig-4]. Further subdivisions into five categories were enabled by the addition of 0.03gm of intrinsic pigments Ivory (FI-SK03), blush (FI-SK 13), Santa Fe (FI- SK 11), burnt sienna (FI- 218) and umber (FI- 217). Thus the shades were arranged from a lighter shade to a darker one. To recognise the shade tabs prefix of dominant hue Y for group I, R for group II and B for group III was implicated. The value was indicated by numbering from 1-5 for each group. So Y5 would indicate the darkest shade tab in the yellow hue. The pigmented silicone was packed into the mould and was cured for 30 minutes [Table/Fig-5]. The processed silicone shade tab was retrieved from the mould and finished with fine grit finishing stone (Factor II finishing kit Inc, Lakeside, AZ, USA) [Table/Fig-6]. The colour formula for reproduction of prescribed shade tabs are given in [Table/Fig-7,8 and 9] for all the groups.


Silicone packed into mould.

Custom Intrinsic silicone shade guide.
Colour specifications to obtain shades as in Group I – Yellow hue.
| Pigments | Shade | Quantity |
|---|
| White | | 1* |
| Tan | | 1 |
| Yellow | | 1 |
| Ivory | Y1 | 1 |
| Blush | Y2 | 1 |
| Santa fe | Y3 | 1 |
| Burnt sienna | Y4 | 1 |
| Umber | Y5 | 1 |
1* - Refers to one drop equals 0.03gm
Colour specifications to obtain shades as in Group II – Red hue.
| Pigments | Shade | Quantity |
|---|
| White | | 1* |
| Tan | | 1 |
| Red | | 1 |
| Ivory | R1 | 1 |
| Blush | R2 | 1 |
| Santa fe | R3 | 1 |
| Burnt sienna | R4 | 1 |
| Umber | R5 | 1 |
1* - Refers to one drop equals 0.03gm
Colour specifications to obtain shades as in Group III – Blue hue.
| Pigments | Shade | Quantity |
|---|
| White | | 1* |
| Tan | | 1 |
| Blue | | 1 |
| Ivory | B1 | 1 |
| Blush | B2 | 1 |
| Santa fe | B3 | 1 |
| Burnt sienna | B4 | 1 |
| Umber | B5 | 1 |
1* - Refers to one drop equals 0.03gm
Sample Size and Selection
A cross-sectional survey was performed on 100 random Indian subjects for skin colour matching using the shade guide. A 95% confidence interval with 5.0% margin of error was estimated to obtain a power of 80 in the research. A convenience sampling was done to include the volunteering undergraduate dental students studying in the college to participate in the study. Students between the age group of 17-25 years inclusive of both genders in the ratio of 1:1 were involved. Other inclusive criteria’s were subjects must be devoid of any skin diseases, postsurgical scars, deformities of face, skin bleaching and burn injury. They were restricted from use of skin care products for at least 2 hours prior to the evaluation. Subjects with disorders of skin like hypo or hyper pigmentation, skin tanning, post radiation therapy, and students not willing to participate were excluded.
Evaluation of Colour Matching
The shade tab was placed in close approximation against the skin to examine the match [Table/Fig-10]. Visual evaluation was done independently by the primary author and by three other experienced operators. The evaluators were examined for any colour vision deficiency. All the evaluators underwent the Ishihra colour test (Pseudo Isochromatic Plate (PIP) Colour Vision Test) and were found to have had normal vision. Scoring for each group was done by all the evaluators on the sheet. Each evaluator depicted the colour match thrice for a subject in order to avoid errors. Colour match at first sight was identified instantly. Prolonged time for matching was not permitted as the eyes would fatigue.
Visual colour match with shade tab.

The visual assessment of colour matching was done based on a score sheet using a scoring system. The scoring record was interpreted as:
Total mismatch and unacceptable.
Almost same and acceptable.
Adequate colour match and satisfactory.
Accurate colour match.
Statistical Analysis
Statistical analysis of the data was done at a significance level of p<0.05 with Kappa coefficient to assess the agreement among the evaluators.
Results
The kappa values were found to be 0.47 to 0.78 for yellow based group I, 0.13 to 0.65 for red based group II, and 0.07 to 0.36 for blue based group III as given in [Table/Fig-11]. This revealed that the shade tabs of yellow and red based hues matched well and showed a statistically good colour matching as given by the percentage agreement for groups in [Table/Fig-12]. The statistical data revealed that the shade guide can be effectively used for intrinsic skin colour identification, with yellow based group being more accurate followed by red and then blue based groups.
Kappa values between the evaluators for groups.
| Evaluators | Group I | Group II | Group III |
|---|
| I | 0.6529p = 0.0094 | 0.3243p = 0.0498 | 0.2784p = 0.1258 |
| II | 0.7893p = 0.0082 | 0.6574p = 0.0013 | 0.3657p = 0.0197 |
| III | 0.4745p = 0.0195 | 0.1394p = 0.7563 | 0.0796p = 0.7564 |
| IV | 0.5658p = 0.0036 | 0.4665p = 0.0135 | 0.2876p = 0.1324 |
Percentage agreement for groups
| Evaluators | Group I | Group II | Group III |
|---|
| I | 78.00% | 49.33% | 58.00% |
| II | 84.58% | 79.67% | 79.33% |
| III | 75.33% | 78.66% | 66.67% |
| IV | 80.00% | 67.33% | 62.33% |
Discussion
Rehabilitation of patients affected by either congenital or acquired maxillofacial defects with prosthesis has been documented from the 1600 AD [3]. The functional and aesthetic impairments following extensive surgery traumatise the physical and mental health of the victims. Positive reconstruction can be effective with a multidisciplinary approach. Mere physical restoration with precisely secured prosthesis does not satisfy the patient. Bestowing an aesthetic natural life like prosthesis has become mandatory [11].
Among the many factors that contribute to the natural looking prosthesis, replication of skin colour is an arduous task. The skin is a multilayered structure with dermis, epidermis and subcutaneous tissues, each of varying thickness & composition. Existence of pigments like melanin, beta carotene and haemoglobin within skin cells, coupled with the behaviour of skin towards ambient light, make colour matching altogether strenuous [12]. It is towards achieving this goal that various materials have been developed.
Documented evidence on superior properties of silicone elastomers as maxillofacial prosthetic material has made grounds for silicones as the most commonly recommended material of choice today [13]. Colouration of prosthesis is feasible with addition of intrinsic, extrinsic or combination of both pigments. Incorporation of intrinsic pigments to the base silicone material serves as the foundation and durable colour of the prosthesis [14,15].
Human skin colour measurements can be done both subjectively and objectively. For measuring instruments, contact measuring instruments including most Colorimeters and Spectrophotometers have been commonly used in maxillofacial prosthetic measurement and skin colour research [16,17]. However, employment of such instruments on layered structures like skin or teeth cannot duplicate the translucency and the surface texture. These are contact instruments which come in approximation to the surface of the skin in order to absorb all the reflected light. Human skin being translucent causes some light to scatter beyond the aperture of the instrument without absorption. This produces what is called as “Edge Loss” and is considered as one of the limitation of such devices. The edge loss is directly proportional to the size of the aperture and the beam in the instrument. Errors also occur due to varying contact pressure of the measuring devices [7–9]. Therefore a customised intrinsic silicone shade guide was warranted to be used for shade selection in clinical practice.
Indian natives have pronounced content of melanin pigment in their skin and hence yellow hue was chosen for group I. Wassermann, in an extensive spectrophotometric research on skin colour, proved that irrespective of racial groups, the dominant reflected hue was red [18]. Thus red hue was chosen for group II. The presence of bluish-white connective tissue in the dermis and haemoglobin in the veins made us chose blue hue as group III. As Indian natives range from a mixture of light skin tone to darker tone, various intrinsic pigments were added to obtain the values [19,20].
The interrater agreement with kappa statistics revealed moderate to substantial colour matching with group I yellow based hue, fair to moderate matching with group II red based hue and slight to fair agreement with blue based group III individuals. A 73-84% agreement was depicted with yellow based hue group and agreement was diminished in group III. The results were statistically significant at a p-value of < 0.05. The results inferred a strong colour match with group I and least with group III as given in [Table/Fig-12]. It is evident from the result that shade guide can be very effectively used for colour matching of yellow based skin tone rather than for blue based skin tones.
Quantitative measurement of skin colour with the aid of newer objective instruments like hand held colorimeter, spectrophotometer are yet far from perfect because of few limitations like contact edge loss, minimal accuracy, poor repeatability etc., [21,22]. Not all patients can afford for this high expenditure in objective colour simulation methodologies. Therefore, colour replication with the assistance of shade guide warrants a feasible option in day to day clinical practice.
Limitation
Nevertheless the errors incorporated in visual shade match using the current shade guide, applicability to only silicone maxillofacial elastomer material which is not economical for all patients can be contemplated as the few limitations of the present study.
Conclusion
Thus application of current simple customised intrinsic silicone shade guide can be employed for colour replication among Indian natives. It must be nailed that only base intrinsic colour is gained using the shade guide and not the final colour of the prosthesis. Final colour can be achieved only after extrinsic colouration and characterisation. Future research can lead towards usage of a new measurement tool in objective colour matching system for fabrication of maxillofacial prosthesis.