Massive Broad Ligament Cellular Leiomyoma with Cystic Change: A Diagnostic Dilemma
Preeti Sharma1, Sufian Zaheer2, Amit Kumar Yadav3, Ashish Kumar Mandal4
1 Resident, Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
2 Associate Professor, Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
3 Associate Professor, Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
4 Director Professor and Head of Department, Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Preeti Sharma, Resident, Department of Pathology, 4th Floor, Vardhman Mahavir Medical College, Safdarjung Hospital New Delhi-110002, India.
E-mail: preetisharma261189@gmail.com
Leiomyomas are known to arise from uterus, but rarely from broad ligament. Further, cellular leiomyoma of broad ligament is the least common variant reported in literature. The diagnostic dilemma arises when leiomyomas undergo degenerative changes. This poses both clinical and radiological difficulty in differentiating with an ovarian tumour. We present an unusual case of a huge broad ligament mass measuring 29x19x09cm, mimicking an ovarian tumour both clinically and radiologically. Histopathology revealed cellular leiomyoma of broad ligament with cystic and myxoid degeneration hereby being the second case reported in literature. This case is being presented not only because of the rare incidence but also due to its diagnostic confusion with ovarian malignancy on clinical evaluation and radiological findings.
Broad ligament, Cellular leiomyoma, ovarian tumour
Case Report
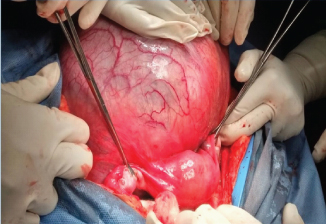
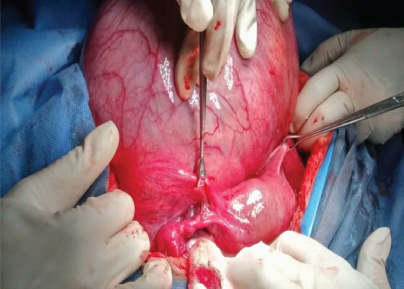
A 50-year-old postmenopausal woman presented with complaints of mass in abdomen and abdominal discomfort since 2-3 years. It was gradual in onset and progressive in nature with history of rapid increase in size since last 2 months. There was history of incomplete voiding of urine since 2 months not associated with fever, anorexia or weight loss. On physical examination the woman was afebrile, haemodynamically stable with normal vitals parameters. On per abdominal examination there was a well-defined lower abdominal mass of size 28-30 weeks. The mass was non-tender and cystic in consistency. The lower pole of mass could not be reached. Per vaginum examination revealed a healthy vagina and cervix. Uterus was deviated towards right side and exact size of uterus could not be assessed. A large non-tender mass was felt on left side through left and posterior fornix. Routine blood analysis as well as liver function and kidney function tests were within normal limits. CA-125 levels were: 155 mU/ml. CT scan of abdomen revealed a large septate cystic lesion in the pelvic cavity with extension to upper abdomen. The lesion showed mass effect on the urinary bladder along with displacement of the bowel loops to the periphery. No myometrial mass was seen. Bilateral ovaries were not visualized separately. Based on the clinico-radiological findings diagnosis of an ovarian mass lesion was made and the patient was planned for an explorative laparotomy. Intra-operative findings revealed a normal sized uterus. Bilateral tubes and ovaries were normal [Table/Fig-1]. A large cystic mass was present between the bladder anteriorly and the uterus posteriorly. The mass seemed to be arising from the left broad ligament [Table/Fig-2]. The mass had no attachment with the uterus. Specimen was sent for histopathological examination.
Intraoperative findings revealed a normal uterus, bilateral fallopian tubes and bilateral ovaries.
Intraoperative findings revealed large cystic mass arising from the left broad ligament. the mass had no attachment with the uterus.
On gross examination, uterus with cervix measured 8x6x3cm. Cut surfaces of uterus and cervix were normal. Bilateral tubes and ovaries were within normal limits. Received separately was a mass measuring 29x19x09cm and weighing 2100grams. Its outer surface was encapsulated and smooth. The cut surface of mass revealed solid and cystic areas. The solid foci had a brown fleshy homogenous appearance. The cysts contained altered haemorrhagic fluid [Table/Fig-3].
The cut surface of mass revealed solid and cystic areas. The solid foci had a brown fleshy homogenous appearance and the cysts contained altered haemorrhagic fluid.

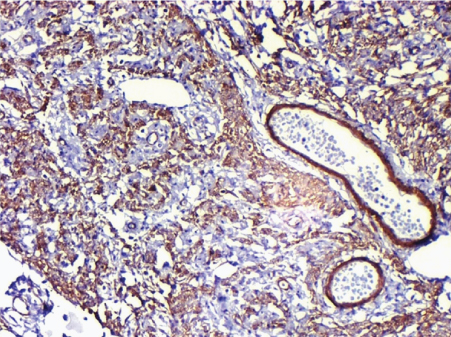
Microscopically, sections from cervix and uterus showed chronic cervicitis, atrophic endometrium and an unremarkable myometrium. Bilateral tubes and ovaries were also within normal limits. The cystic mass revealed a well encapsulated tumour composed of spindle cells arranged in interlacing bundles and sheets. The individual cells were elongated with abundant dense eosinophilic cytoplasm and cigar shaped nuclei [Table/Fig-4]. Numerous foci showing increased cellularity and mitosis (2-3/10 hpf) were observed. Areas of cystic and myxoid degenerations were also seen microscopically. Immunohistochemically, the tumour cells were positive for smooth muscle actin [Table/Fig-5]. Based on the above mentioned findings a histopathological diagnosis of a broad ligament cellular leiomyoma with secondary changes was given.
Pictomicrograph showing cellular tumour composed of spindle cells arranged in interlacing bundles and sheets. (H&E 20X)

Immunohistochemically, the tumour cells were positive for smooth muscle actin (20x).
Discussion
Uterine leiomyomas are the most common myomas of the female genital tract [1]. They can also arise in smooth muscles at extra uterine sites such as broad ligament, round ligament and ovarian ligament. Even though broad ligament is the commonest extra uterine site for the occurrence of leiomyoma, the incidence is however <1% [2]. Further, the variants of leiomyomas have been described on the basis of their histomorphology. These include cellular leiomyoma, atypical leiomyoma, symplastic leiomyoma, mitotically active leiomyoma, epithelioid leiomyoma, etc. Of these histopathological forms the least common variant is cellular leiomyoma (<5%). Only one case of cellular leiomyoma of broad ligament has been reported in literature till date [3]. The patient was a 29-year-old nullipara who presented with a parametrial mass. The clinical symptoms and USG findings were suggestive of a myoma with the tumour markers within normal limits. Thus the authors reported no clinical dilemma. Histopathology revealed cellular leiomyoma. Our case, on the other hand presented with elevated tumour markers and a solid cystic mass on radiology thereby posing great diagnostic difficulty both for the clinicians as well as radiologists.
Tumours of the broad ligament can be of epithelial or mesenchymal origin, of which the former are more common. Among the mesenchymal tumours the bulk is constituted by leiomyomas [4] which can be of two types- false and true. While the false myomas have a pedicle connecting it with the uterus, the same is not true for the true type [5]. Cellular leiomyomas contain more smooth muscle fibres than conventional leiomyomas and are defined by the World Health Organization as typical leiomyomas that exhibit hypercellularity [6,7].
Broad ligament leiomyomas are usually asymptomatic but if neglected for a long time, they can reach an enormous size resulting in chronic pelvic pain, menstrual abnormalities, compression and dysfunction of the bladder and bowel [2]. Broad ligament fibroids can produce elevated cancer marker CA-125 levels, like in our case thereby leading to diagnostic confusion with metastatic ovarian carcinoma. However, CA-125 is a non-specific marker and is also raised in endometriosis and serous ovarian tumours thereby posing greater difficulties in preoperative diagnosis [8].
Extra-uterine fibroids especially those which undergo massive cystic degeneration may pose clinical and radiological diagnostic difficulties. These are considered to be due to inadequate blood supply and depend on the degree of vascular insufficiency [9]. The most commonly encountered degenerations include myxoid and calcific degenerations. Cystic degeneration is considered as an extreme sequel of oedema in leiomyomas. Its incidence has been reported to be as 4% [10].
In females, the differential diagnosis of such massive cystic lesions in lower abdomen or pelvis includes ovarian cysts (benign and malignant), paraovarian cysts, broad ligament and round ligament cysts and lymphoceles [9]. While two cases of broad ligament leiomyomas with myxoid and cystic degenerative changes have been previously reported from India [11,12], no prior case of broad ligament cellular leiomyoma has been reported from the Indian subcontinent and thus deserves mention.
Conclusion
Unusual location, large size of the lesion, marginally elevated CA-125 levels and massive cystic degeneration were the diagnostic challenges in our case which led to confusion with an ovarian malignancy on clinical and radiological grounds. Histopathological examination revealed the diagnosis of a cellular leiomyoma with myxoid and cystic degeneration. Thus, massive extrauterine leiomyomas can mimic ovarian tumours on clinical and radiological examination. Broad ligament leiomyoma should be kept as an important differential diagnosis for such solid-cystic adnexal masses.
[1]. Jagtap VS, Khatib GM, Jagtap SS, Kshirsagar NS, Large leiomyoma of the broad ligamentJ Med Allied Sci 2013 3:85-87. [Google Scholar]
[2]. Bakari F, Sulayman HU, Avidime S, Ameh N, Adesiyun AG, Huge Broad Ligament Leiomyoma: A Case ReportCase Reports in Clinical Medicine 2015 4:55-59. [Google Scholar]
[3]. Chmaj-Wierzchowska K, Buks J, Wierzchowski M, Szymanowski K, Opala T, Leiomyoma cellulare in the broad ligament of the uterus – case report and review of literatureGinekol Pol 2012 83:301-04. [Google Scholar]
[4]. Thor AD, Young RH, Clement PB, Pathology of fallopian tube, broad ligament, peritoneum and pelvic soft tissuesHum Pathol 1991 22:856-67. [Google Scholar]
[5]. Parker WH, Uterine myomas: An overview of development, clinical features and managementObstet Gynecol 2005 105:216-17. [Google Scholar]
[6]. Wilkinson N, Rollason T, Recent advances in the pathology of smooth muscle tumours of the uterusHistopathology 2001 39:331-41. [Google Scholar]
[7]. Clement P, The pathology of uterine smooth muscle tumours and mixed endometrial stromal smooth muscle tumours: A selective review with emphasis on recent advancesInt J Gynecol Pathol 2000 19:39-55. [Google Scholar]
[8]. Jagtap VS, Gupta A, Kshirsagar NS, Broad Ligament Leiomyoma Mimicking As Ovarian TumourSch J App Med Sci 2014 2:258-60. [Google Scholar]
[9]. Yuel VI, Kaur V, Broad ligament fibroid: An unusual presentationJ K Sci 2006 8:217-18. [Google Scholar]
[10]. Bansal P, Garg D, A Case of Massive Broad Ligament Leiomyoma Imitating an Ovarian TumourJ Clin Diagn Res 2014 8:136-37. [Google Scholar]
[11]. Asotra S, Kaushik R, Gulati A, Broad ligament fibroid with neurilemmoma like patternJ K Sci 2009 11:215 [Google Scholar]
[12]. Godbole RR, Lakshmi KS, Vasant K, Rare case of giant broad ligament fibroid with myxoid degenerationJ Sci Soc 2012 39:144-46. [Google Scholar]