Sinister Splenic Artery Pseudoaneursym: A Rare Case of Unidentified Aetiology
Pranav Honnavara Srinivasan1, Gopi Ellikunnel Vithon2, Krishna Narayanan Mandyam Dhati3, Vadukkoot Raman Rajendran4
1 Senior Resident, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
2 Professor, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
3 Senior Resident, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
4 Professor and Head, Department of Radiodiagnosis, Government Medical College, Kozhikode, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pranav Honnavara Srinivasan, 816, 37th Cross, 18th Main, 4th T Block, Jayanagar, Bangalore-560041, India.
E-mail: pranavhs8@gmail.com
Splenic Artery Pseudoaneurysms (SAP) are very rare. Giant SAPs are those which are more than 5 cm in diameter and are rarer. SAPs are usually caused by pancreatitis, trauma, surgery or other iatrogenic interventions, vasculitis, local infective or inflammatory processes. We report the successful surgical management of a giant SAP of unidentified aetiology. This case report highlights the significance that this entity may present atypically and hence, early recognition and aggressive management may be life saving.
Aneurysm, Pancreatitis, Partial thrombosis
Case Report
We report a 56-year-old woman who presented with abdominal pain and mass in the left hypochondrium of 2 weeks duration with normal haemodynamic status. She had a negative history for abdominal or chest trauma, abdominal surgeries, percutaneous or endoscopic interventions, previous visits to the hospital for pancreatitis or vasculitis. On further evaluation, her serum amylase and lipase, serum ANA were found to be within the normal reference range.
In Contrast Enhanced Computed Tomography (CECT) of the abdomen, a true splenic artery aneurysm is seen as a round or fusiform dilatation of the splenic artery sometimes with a mural thrombus with wall calcification. In SAP, contrast extravasation with acute haematoma is visualised.
In our patient, CECT abdomen demonstrated a well-defined focal enhancing area of size 8.6 x 8.1 x 8.2 cm involving the tail region of the pancreas closely abutting the splenic hilar vessels signifying acute haematoma with extravasation. The enhancing area showed enhancement similar to that of vascular structures and was surrounded by an area of partial thrombosis. All the above features were in favour of SAP over a true aneurysm [Table/Fig-1,2].
Transverse slice upper abdominal CECT of the abdomen
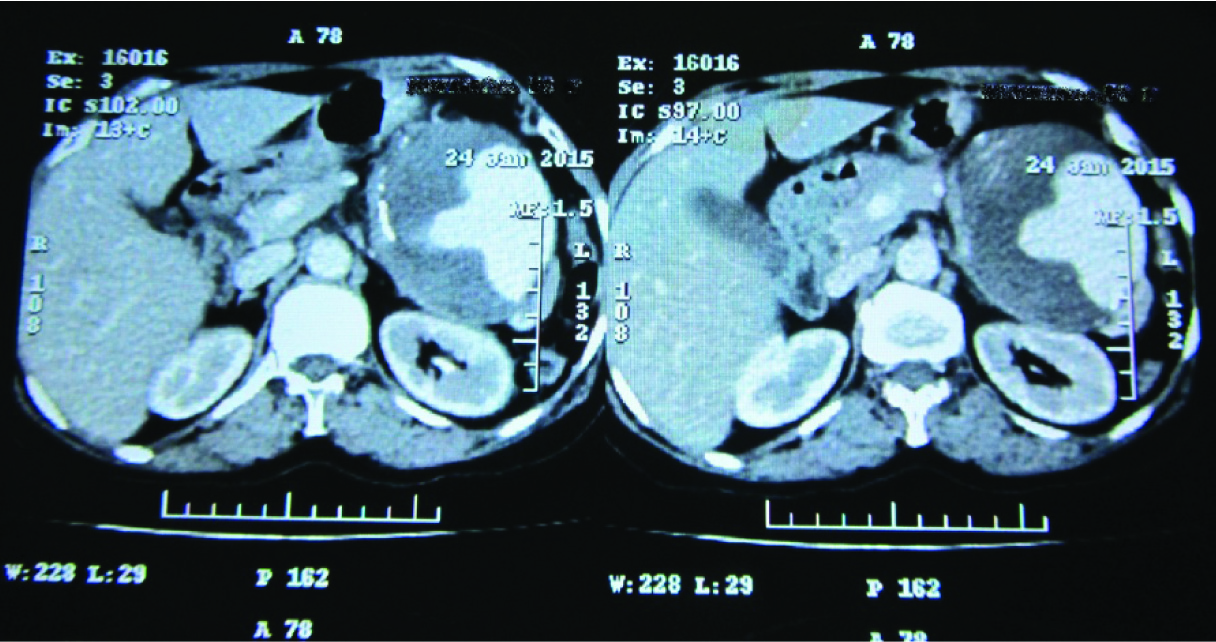
Coronal slice abdominal CECT of the abdomen

The pancreas, spleen and kidneys were visualized as normal.
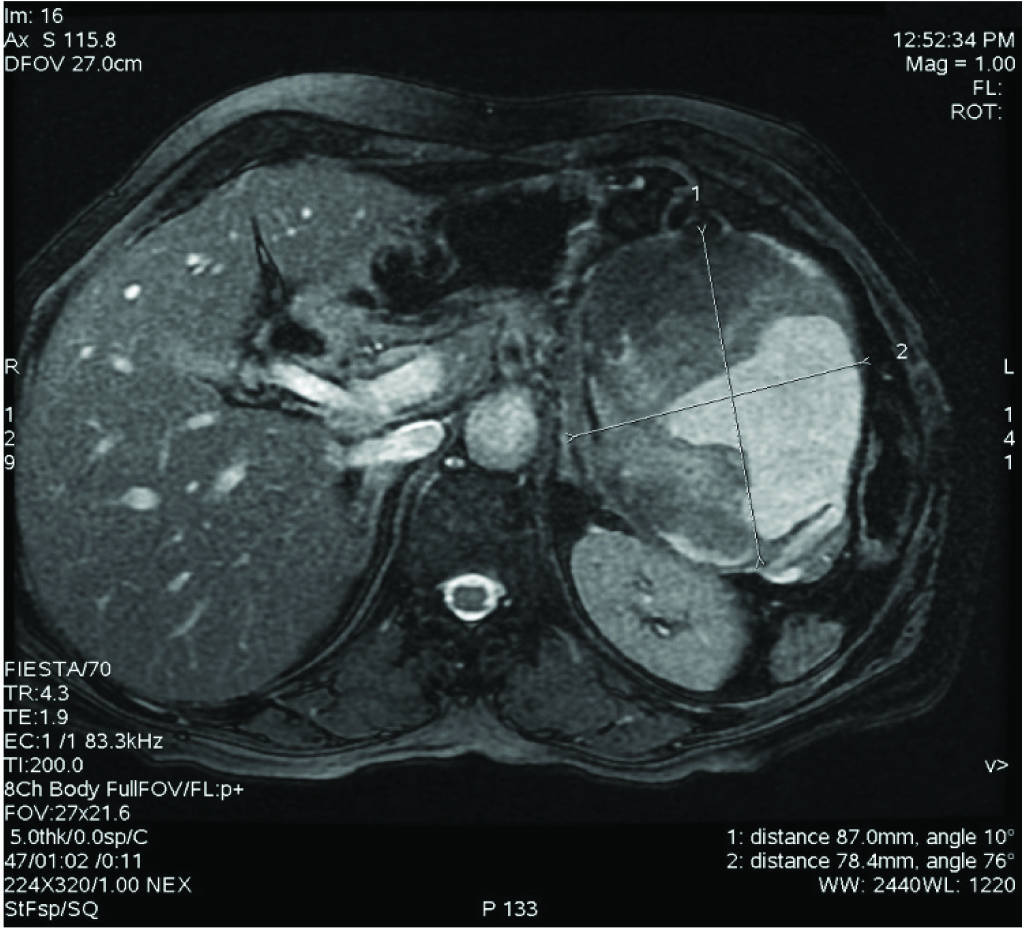
Magnetic Resonance Imaging (MRI) demonstrated a partially thrombosed splenic artery pseudoaneurysm evidenced by a heterointense well defined lesion 8.2 x 7.8 x 7.9 cm, predominantly hyperintense with hypointense periphery. The lesion was visualized as arising from the distal splenic artery.
Posteriorly, the lesion was abutting and compressing the left kidney and anterolaterally the lesion was abutting and compressing the descending colon [Table/Fig-3].
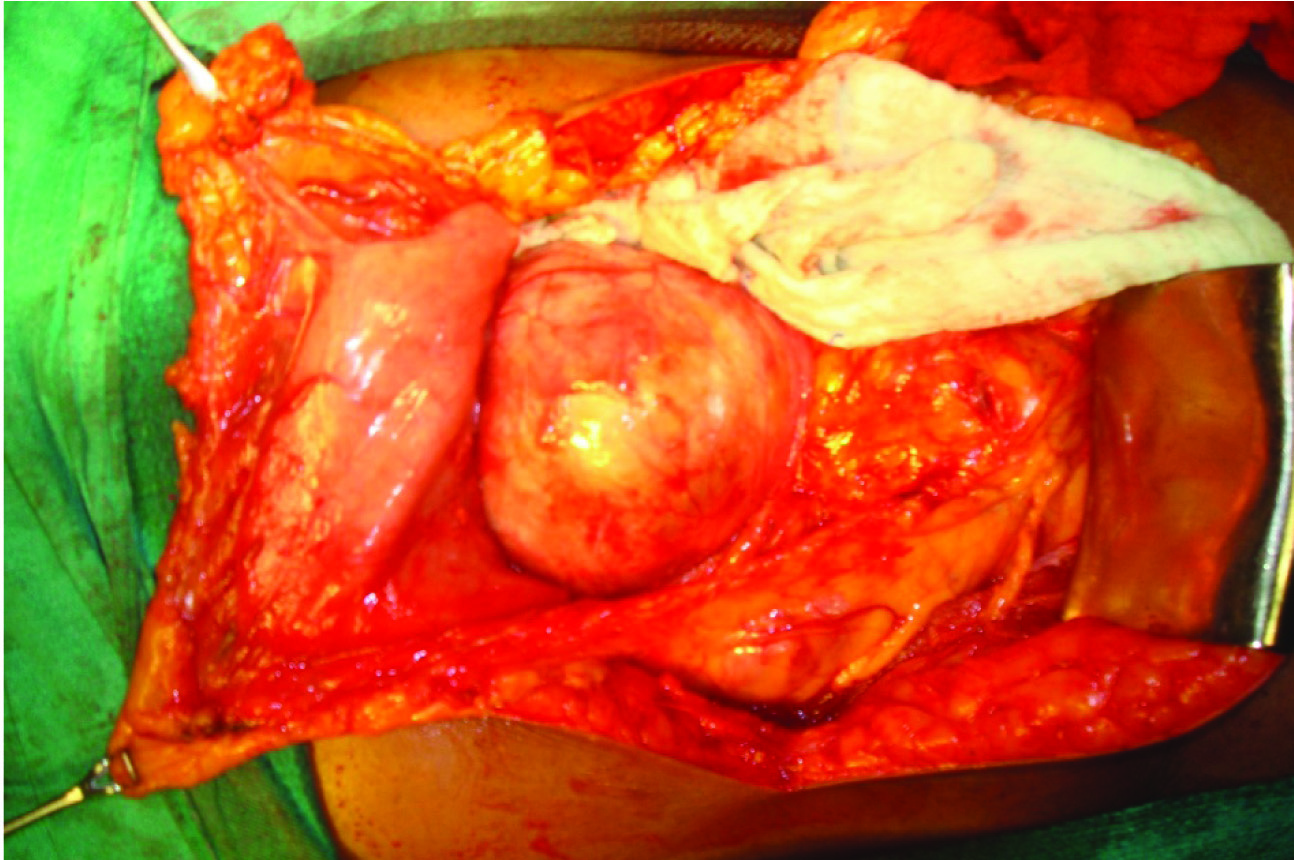
We opted for an open procedure due to the large size of the pseudoaneurysm with vaccination against pneumococcus, haemophilus influenza and meningococcus given on the day of the procedure. At laparotomy, a giant pseudoaneurysm was found in relation to the distal splenic artery [Table/Fig-4]. The pancreas and spleen were grossly normal. With proximal vascular control on the splenic artery, en bloc excision of the pseudoaneurysm with spleen and distal pancreas was performed [Table/Fig-5] with a drain placed at the site of distal pancreatectomy. The patient recovered well with no postoperative complications. The drain was removed on the 5th postoperative day. Patient was discharged on the 9th postoperative day after removing the skin staples with advice to report immediately in case of fever or abdominal pain.
Intraoperative photograph – showing the giant splenic artery pseudoaneurysm. The transverse colon has been retracted inferiorly and the Morris retractor is in the epigastrium. The spleen is not visualized completely.
Photograph of the excised specimen

Discussion
Visceral aneurysms or pseudoaneurysms are those which arise from the celiac artery, superior mesenteric artery, inferior mesenteric artery or from any branches of these vessels [1]. Among these, the most common are from the splenic artery. Pseudoaneurysms have to be differentiated from true aneuryms as the management differs albeit slightly.
SAP is very rare, with less than 250 cases reported in the literature [2]. The aetiology of true aneurysms differs from that of pseudoaneuryms. The causes of true Splenic Artery Aneurysm (SAA) are atherosclerosis, collagen vascular disorders, medial sclerosis and fibromuscular dysplasia [3]. The causes of SAP are trauma, infections/ inflammatory disorders, vasculitis, surgery and other iatrogenic interventions including percutaneous and laparoscopic procedures [3–5].
The clinical presentations of SAA and SAP are highly variable. Most SAA are asymptomatic being previously detected only during autopsy with death being caused by rupture of these lesions. Many SAA are now incidental findings on the growing number of cross sectional imaging studies being done for unallied conditions. In patients who are symptomatic, most present with vague abdominal pain or mass with very few patients presenting as emergencies with features of rupture. Rare giant aneurysms and pseudoaneurysms have been described in the literature which produced symptoms due to pressure on nearby organs. However, there have been cases of aneurysms attaining more than 10cm in size and still being asymptomatic [6,7].
The modality of choice for diagnosis of SAA and SAP is Contrast Enhanced Computed Tomography (CECT) of the abdomen, in which SAA and SAP exhibit classical features [8].
SAA show up as fusiform or saccular dilatations of the splenic artery with or without peripheral calcification and may show evidence of a mural thrombus on the non contrast images. In cases of SAP, well defined focal enhancing areas with high attenuation as that of arteries surrounded by a low attenuation area of haematoma are seen [8].
MRI of the abdomen with contrast is supportive to CECT. SAA are visualized as focal enlargements of the splenic artery, are typically round with sharp margins. Calcification is visualized as signal void on gradient echo T-1 weighted images. SAP typically tend to be irregularly shaped, are not round as compared with true aneurysms and may show a mural thrombus.
The treatment of SAA and SAP is usually individualized. The general principals are outlined. Small SAA less than 2 cm may be managed expectantly with regular follow up and serial imaging. The indications for intervention for SAA include size more than 2 cm, female patient of child bearing age, portal hypertension and symptomatic lesions [1].
The general recommendation is that all splenic artery pseudoaneurysms be treated either with surgery or endovascular interventions regardless of size or symptoms as they have a high tendency to rupture [9–11]. The choice of intervention include open or laparoscopic surgery and endovascular techniques. Treatment with open surgery is a secure and sound approach. The options include aneurysmectomy and bypass grafting, aneurysmectomy and end to end anastomosis and ligation of the offending vessel. The benefits of open surgery are that organs may directly be visualized for causative pathologies like portal hypertension, pancreatitis, pseudocysts and abscesses. Also, the requirement for close follow up and serial imaging as required after endovascular techniques is reduced. Laparoscopic surgery is an efficacious replacement for open surgery in SAA and SAP, but it is usually reserved for small aneurysms close to the splenic hilum. Endovascular therapy is usually reserved for small SAA and SAP. The advantages include short hospital stay, decreased overall cost and quicker return to work. The disadvantages of endovascular therapy include intervention related structural injury, contrast toxicity, a higher rate of failure and the need for more aggressive follow up and serial imaging when compared to open or laparoscopic surgery. Placement of coils, glue, gelfoam, stenting and injection of ethyl alcohol are a few ways by which endovascular techniques are accomplished [12].
About 20-30% of patients with SAA present with rupture which is a true surgical emergency. In the setting of haemodynamic collapse due to rupture, peri-operative mortality rates as high as 70% have been reported [13].
Conclusion
Giant pseudoaneurysms of the splenic artery are very rare. They may not be suspected if there is no history of pancreatitis or trauma. Through this case report we would like to highlight the significance that SAP may present atypically and hence, early recognition and aggressive management may prevent adverse outcomes and be life-saving.
[1]. Bakhos CT, McIntosh BC, Nukta FA, Fiedler PN, Staged arterial embolization and surgical resection of a giant splenic artery aneurysmAnn Vasc Surg 2007 21(2):208-10. [Google Scholar]
[2]. Schatz RA, Schabel S, Rockey DC, Idiopathic Splenic Artery Pseudoaneurysm Rupture as an Uncommon Cause of Haemorrhagic ShockJ Investig Med High Impact Case Rep 2015 3(2):2324709615577816 [Google Scholar]
[3]. Carroccio A, Jacobs TS, Faries P, Endovascular treatment of visceral artery aneurysmsVasc Endovascular Surg 2007 41(5):373-82. [Google Scholar]
[4]. Nicholson AA, Patel J, McPherson S, Shaw DR, Kessel D, Endovascular treatment of visceral aneurysms associated with pancreatitis and a suggested classification with therapeutic implicationsJ Vasc Interv Radiol 2006 17(8):1279-85. [Google Scholar]
[5]. Ceppa EP, Evans DC, Upton EC, Miller MJ, Endovascular treatment of a traumatic visceral aneurysmJ Trauma 2008 65(4):929-32.doi: 10.1097/01.ta.0000215372.65464.56 [Google Scholar]
[6]. Russo A, Francia C, Zaottini A, Pagliei M, Giant splenic artery aneurysm, incidentally diagnosedAnn Ital Chir 2008 79(5):371-75. [Google Scholar]
[7]. Kim MJ, Kim KW, Diffuse splenic lesions. In Sahani DV, Samir AEAbdominal imaging 2010 1st edSaunders:968-997. [Google Scholar]
[8]. Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literatureJ Vasc Surg 2003 38(5):969-74. [Google Scholar]
[9]. de Perrot M, Buhler L, Schneider PA, Mentha G, Do aneurysms and pseudoaneurysms of the splenic artery require different surgical strategy?Hepatogastroenterology 1999 46(27):2028-32. [Google Scholar]
[10]. Parikh M, Shah A, Abdellatif A. Splenic artery pseudoaneurysm complicating pancreatitisJ Gen Intern Med 2011 26(3):343-44.doi: 10.1007/s11606-010-1538-z. Epub 2010 Oct 22 [Google Scholar]
[11]. Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, The endovascular management of visceral artery aneurysms and pseudoaneurysmsJ Vasc Surg 2007 45(2):276-83.discussion 283 [Google Scholar]
[12]. Lakin RO, Kashyap VS, Splanchnic artery aneurysms. In Cronenwett JL, Johnston KWRutherford’s Vascular Surgery 2014 8th edSaunders:2220-235. [Google Scholar]
[13]. Messina LM, Shanley CJ, Visceral artery aneurysmsSurg Clin North Am 1997 77(2):425-42. [Google Scholar]