Concurrent Infections of Conidiobolus Coronatus with Disseminated Tuberculosis Presenting as Bilateral Orbital Cellulitis
Deepa John1, Aparna Irodi2, Joy Sarojini Michael3
1 Associate Surgeon, Department of Ophthalmology, Christian Medical College, Vellore, Tamil Nadu, India.
2 Associate Professor, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India.
3 Professor, Department of Microbiology, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepa John, Associate Surgeon, Department of Ophthalmology, Schell Eye Hospital, Arni Road, Christian Medical College, Vellore – 632001, Tamil Nadu, India.
E-mail: deeparebeccajohn@gmail.com
Zygomycetes species contains two orders of organisms that infect humans, namely Mucorales and Entomophthorales. Entomophthorales cause chronic infection in immunocompetent patients, invading subcutaneous tissues but are non-angioinvasive. This includes Basidiobolus ranarum, Conidiobolus incongruus and Conidiobolus coronatus. We report a case of disseminated tuberculosis with Conidiobolus coronatus infection presenting as orbital cellulitis in an adolescent.
Basal meningitis, Bilateral proptosis, Maxillary sinusitis, Rhinofacial mycosis
Case Report
An 18-year-old girl presented to the ophthalmology department of a tertiary care hospital with decreased vision in both eyes for three days, associated with bilateral pain and swelling of the upper and lower eyelids for two weeks. This was preceded by intermittent episodes of fever for three weeks. On examination, visual acuity in both eyes was perception of light with inaccurate projection of light in all four quadrants. The upper and lower eyelids of both eyes were oedematous, erythematous and indurated [Table/Fig-1]. Extraocular movements were restricted in all quadrants with left eye fixed in adducted position. Bilateral proptosis was present, but there was no conjunctival congestion or chemosis. Pupillary reaction was sluggish and relative afferent pupillary defect was absent. Posterior segment examination showed a normal optic disc. There was no pallor or blurring of the neuroretinal rim. Rest of the fundus including macula and vessels were normal. Exophthalmometry could not be performed due to eyelid oedema.
Photograph showing bilateral oedema, erythema and induration of the eyelids.

She was diagnosed to have bilateral orbital cellulitis and was started on intravenous antibiotics (gentamicin, ceftazidime and metronidazole). Systemic examination revealed palpable cervical lymph nodes and bilateral rhonchi on auscultation.
Investigations: Hb – 10.8 g/dL; Total Count – 15.1 x109/L; DC – N-79, L-11, E-4, M-6; Platelets – 597 x109/L; ESR – 55 mm/hr; PT- 15.3 secs; APTT – 27.5 secs; Creatinine – 0.8μmol/L; VDRL, HIV, HBsAg, anti-HCV–negative.
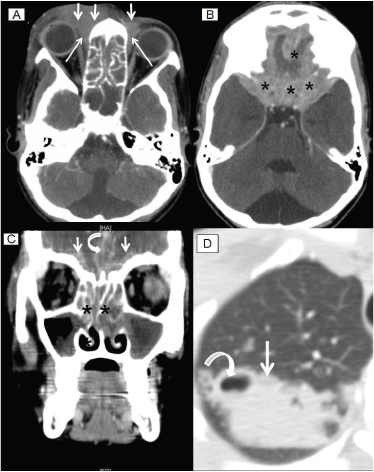
Computerized tomography (CT) showed enhancing hyperdense soft tissue involving the orbits and maxillary sinuses [Table/Fig-2a&b]; extensive basal meningitis in the anterior and middle cranial fossa (CT brain; [Table/Fig-2c]), consolidation with cavitations (CT lungs; [Table/Fig-2d]).
Contrast enhanced axial CT sections through paranasal sinuses and orbits, at level of ethmoid air cells (A) showing sheet like soft tissue thickening along medial canthus, more on right side (short arrows in A) and extending posteriorly into the orbit in the medial extraconal space (long thin arrows in A). Contrast enhanced axial CT sections at level of anterior and middle cranial fossa (B), showing sheet-like meningeal and extradural enhancement in anterior and middle cranial fossa on both sides (* in B). Coronal CT through paranasal sinuses and orbits, at level of ethmoid air cells (C), showing mucosal thickening in nasal cavity and opacifying ethmoid air cells cavity (**). Sheet-like meningeal and extradural enhancement in anterior cranial fossa on both sides (white arrows), also extending along interhemispheric fissure (curved arrow). Axial CT sections through right lung apex (D) showing subsegmental area of consolidation (white arrow) with small areas of cavitation (curved arrow).
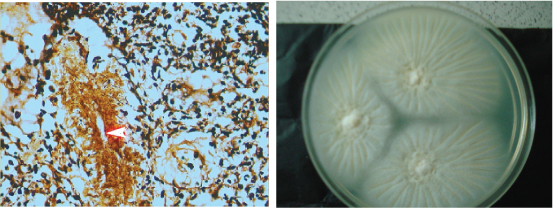
She underwent sinus debridement and tissue from the maxillary sinus was taken by Functional Endoscopic Sinus Surgery (FESS). Histopathological analysis of the sinus tissue showed granulomatous inflammation with hyphal elements. Hyphal elements were sparse, thin-walled and poorly stained surrounded by Splendore-Hoeppli material [Table/Fig-3a] that was intensely eosinophilic. Microbiological culture in Sabouraud dextrose agar showed colonies that were cream-coloured, covered with white powdery mycelium surrounded by satellite colonies consistent with Conidiobolus coronatus, Zygomycosis species [Table/Fig-3b]. There were numerous Acid Fast Bacilli (AFB) of Mycobacterium tuberculosis on sputum examination which was positive in culture as well. Patient was diagnosed to have disseminated tuberculosis with Conidiobolus infection of the maxillary sinuses and orbit. She had open pulmonary tuberculosis hence she was isolated from other patients in the ward.
Microscopy with Gomori Methehamine silver (A) stain and eosin and haematoxilin stain showing hyphal elements that are sparse, thin-walled and poorly stained surrounded by intensely eosinophilic Splendore-Hoeppli material. Culture grew rapidly within 24 hrs on Sabouraud Dextrose agar. At 48 hours they were flat, cream-coloured, glabrous and radially folded. The reverse was colourless. There were satellite lesion consistent with Conidiobolus coronatus, Zygomycosis species both on the plate and lid of the Petridish.
Treatment was commenced with the recommended regimen of isoniazid, pyrazinamide and rifampicin for tuberculosis. In addition, to treat the Conidiobolus infection a single dose of oral fluconazole 400mg was given followed by a recommendation of fluconazole 300mg once daily for three months. Within a week of starting antifungal and antituberculous treatment (ATT) treatment, lid swelling had minimally reduced, however extraocular movements and vision had not improved. She was then discharged and advised directly observed treatment, short-course (DOTS) treatment for tuberculosis, and review in the tuberculosis clinic. She did not return for reassessment. In order to ensure continuation of treatment, repeated attempts were made to trace her and the family including sending personnel to the given address. However, these efforts were unsuccessful as she could not be located and was lost to follow up.
Discussion
Zygomycetes class contains two orders of organisms that infect humans, namely Mucorales and Entomophthorales [1,2]. Mucorales cause acute infection in immunocompromised patients, while Entomophthorales cause chronic infection in immunocompetent patients. Mucorales are angioinvasive, while Entomophthorales invade subcutaneous tissue and are not angioinvasive [1]. Mucorales include Rhizopus and Mucor while Entomophthorales include Basidiobolus ranarum, Conidiobolus incongruus and Conidiobolus coronatus.
Conidiobolus coronatus has a tropical and universal distribution. On decaying vegetation and in soil, it is a saprophyte. On culture it produces villous conidia giving a lace-like appearance. It can invade paranasal sinuses, causing granulomatous lesions, mimicking a sinonasal tumour [3]. C. coronatus can invade adjacent skin as well as subcutaneous tissue of the face and nose, resulting in deformity, hence is also known as rhinofacial mycosis [3,4]. It infects healthy adults, especially males [3]. In humans, mycologically proven cases were first reported in 1965 [5]. It can extend to the nasal dorsum, lips and face with a nodular or infiltrative appearance. The lesions have an erythematous and hard skin overlying [5]. The index patient had the classical indurated, erythematous skin overlying both upper and lower lids [Table/Fig-1]. She presented with acute bilateral lid swelling and loss of vision in both eyes. The rapid spread of the conidiobolus infection from the sinus into the orbit would have resulted in lid swelling and proptosis. Ocular motility restriction in this patient could be due to multiple intracranial nerve involvement secondary to basal meningitis. In the presence of a normal optic disc, rapid loss of vision could be attributed to retrobulbar optic nerve involvement from tuberculous meningitis. Though systemic work up and management was done without delay, her ocular morbidity could not be reversed due to the late presentation. Conidiobolus is non-angioinvasive, hence intracerebral involvement is rare. However cases of cerebral involvement due to spread via adjacent tissues has been reported, caused by Conidiobolus coronatus [3] and Conidiobolus incongruous [6]. In the index patient due to the co-existent pulmonary infection, intracranial involvement resulting in basal meningitis was considered as extra-pulmonary tuberculosis.
Though Entomophthorales are known to cause chronic infection in immunocompetent patients [1], the index patient had a unique acute presentation. The immunocompetent status also was questionable in the presence of concurrent disseminated tuberculosis. However, her blood investigations did not reveal any immunocompromised status. Poor nutrition and low socioeconomic status could have contributed to these multiple infections. Unlike the index patient, Conidiobolus is reported to be common among adult males [4]. Also, Conidiobolus usually presents with nasal obstruction and discharge [1,3], while the index patient presented with ocular symptoms. Immunocompromised patients have presented with lid swelling [6] suggesting a rapid progression into the orbital cavity.
Conidiobolus coronatus orbital involvement has been reported in children [7,8], however this is the first report of concurrent orbital infection of Conidiobolus coronatus with tuberculosis in an adolescent.
Conclusion
In children with fungal sinus and orbital infections, a thorough evaluation is needed to assess their immune status and concurrent infections. Imaging should be done without delay to initiate appropriate treatment quickly and prevent residual morbidity.
[1]. Prabhu RM, Patel R, Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatmentClin Microbiol Infect 2004 10(Suppl1):31-47. [Google Scholar]
[2]. Michael RC, Michael JS, Mathews MS, Rupa V, Unusual presentation of entomophthoromycosisIndian J Med Microbiol 2009 27:156-58. [Google Scholar]
[3]. Jayawickrama MMA, Gamage HUP, Perera PD, Conidiobolus coranatus infection of the para-nasal sinuses masquerading as a sino-nasal tumourCeylon Med J 2012 57:87-88. [Google Scholar]
[4]. Nayak DR, Pillai S, Rao L, Rhinofacial zygomycosis caused by Conidiobolus coronatusIndian J Otolaryngol Head Neck Surg 2004 56:225-27. [Google Scholar]
[5]. Valle ACF, Wanke B, Lazéra MA, Monteiro PCF, Viegas ML, Entomophthoramycosis by Conidiobolus coronatus. Report of a case successfully treated with the combination of itraconazole and fluconazoleRev Inst Med Trop S. Paulo 2001 43:233-36. [Google Scholar]
[6]. Wuppenhorst N, Lee MK, Rappold E, Kayser G, Beckervordersandforth J, With K, Serr A, Rhino-orbitocerebral zygomycosis caused by Conidiobolus incongruus in an immunocompromised patient in GermanyJ Clin Microbiology 2010 48:4322-25. [Google Scholar]
[7]. Lithander J, Louon A, Euan Scrimgeour, Worthing E, Ganesh A, Yaseen M, Orbital entomophthoramycosis in an infant: recovery following surgical debridement, combination antifungal therapy and use of hyperbaric oxygenBr J Ophthalmol 2001 85:374-75. [Google Scholar]
[8]. Al-Hajjar S, Perfect J, Hashem F, Tufenkeji H, Kayes S, Orbitofascial conidiobolomycosis in a childPediatr Infect Dis J 1996 15:1130-32. [Google Scholar]