Morphometric Study of Anterior Clinoid Process and Optic Strut and the Ossification of Carotico-Clinoid Ligament with their Clinical Importance
Anne D Souza1, Vrinda Hari Ankolekar2, Nivedita Nayak3, Mamatha Hosapatna4, Antony Sylvan D Souza5
1 Assistant Professor, Department of Anatomy, Kasturba Medical College, Manipal University, India.
2 Associate Professor, Department of Anatomy, Kasturba Medical College, Manipal University, India.
3 Postgraduate Student, Department of Anatomy, Kasturba Medical College, Manipal University, India.
4 Associate Professor, Kasturba Medical College, Manipal University, India.
5 Associate Dean and Professor, Department of Anatomy, Kasturba Medical College, Manipal University, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mamatha Hosapatna, Associate Professor, Department of Anatomy, Kasturba Medical College, Manipal University-576104, India.
E-mail: mamatha2010@yahoo.com
Introduction
Knowledge about the ossification of the Carotico-Clinoid Foramen (CCF), as it forms a potential site for compression of the internal carotid artery may be beneficial for neurosurgeons and radiologists.
Aim
To obtain a detailed knowledge of morphometry of Anterior Clinoid Process (ACP) and Optic Strot (OS) and the type of ossification of CCF which would be necessary to increase the success of surgeries related to the cavernous sinus and internal carotid artery.
Materials and Methods
Parameters such as the length of ACP from its base to the tip, the width at its base and the distance between the tip of ACP to optic strut were measured in mm using digital calipers. SPSS version 17 was used for the statistical analysis. Paired t-test was applied to compare between right and left sides. Presence of carotico-clinoid foramen was observed and was classified as incomplete, contact form or complete.
Results
The average length of ACP ranged from 12 to 15mm on right side and 11 to 16mm on the left side. Paired t-test was applied to compare the means between the right and left sides. The width of ACP varied between right and left sides and this difference was statistically significant (p<0.05). Out of 12 CCF observed, the commonest type was incomplete (N=7) followed by complete (N=3) and contact form (N=2).
Conclusion
Considering the immense anatomical surgical and radiological importance of morphology of ACP, OS and CCF, this study highlighted the detailed morphometry of these structures. The study also has explained the sexual dimorphism in their morphology.
Cavernous sinus, Morphometry, Foramina
Introduction
Anterior Clinoid Process (ACP) is located on the medial end of the lesser wing of the sphenoid bone. The Carotico-Clinoid Ligament (CCL), joins ACP to the middle clinoid process (MCP) which is sometimes ossified. Adural fold extending between the anterior and middle clinoid processes or ossification of the CCL may result in the formation of the Carotico Clinoid Foramen (CCF) [1].
The optic strut (OS) is a bony structure that is closely related to the significant structures such as the cavernous sinus, the internal carotid artery, the optic nerve and the pituitary gland [2].
In neurosurgical operations, the ACP is usually accessed to gain entry into the clinoid space. Intracranial course of internal carotid artery is related medially to the ACP. The presence of an ossified CCL may form a potential site for compression of the internal carotid artery. Variations in the ACP may pose a risk while it is being removed in regional surgical procedures [3].
Knowledge about the ossification of the CCL would be essential for neurosurgeons and radiologists in day-to-day clinical practice [4]. During the surgical interventions on tumors and aneurysms in the sellar region, mobilization of the ACP and the OS would provide a better approach to the internal carotid artery and the optic nerve. A massive ACP would pose difficulty during such approach, which by removing can cause injury to optic nerve and internal carotid artery [5,6].
According to Lang, CCF is formed by the ossification of the carotico clinoid ligament during early childhood. The presence of this foramen is of great importance to neurosurgeons since it intervenes in the mobilization of the cavernous segment of the internal carotid artery. A preoperative detection of CCF, by CT imaging, has a huge clinical significance in surgical procedures involving the cavernous segment of internal carotid artery [7].
Aim
Therefore, the present study was aimed to obtain a detailed knowledge morphometry of ACP and OS and the type of ossification of CCF which would be necessary to increase the success of surgeries related to the cavernous sinus and internal carotid artery.
Materials and Methods
The present cross-sectional observational study was done in the Department of Anatomy, Kasturba Medical College, Manipal during the year 2014. A total of 27 skulls were included in the study. Sexual dimorphism of the skulls was noted based on the criteria given by Walrath et al., [8]. The skulls with damaged ACPs were excluded from the study. Required parameters were measured in mm using digital calipers.
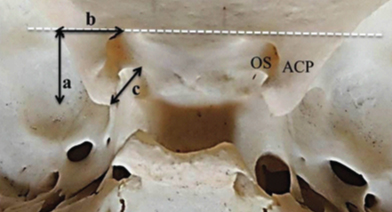
The length of ACP was measured from its base to the tip and the width at its base was noted. The distance between the tip of ACP to optic strut (OS) was also measured. The measured parameters are shown in [Table/Fig-1].
The parameters measured.
ACP- Anterior clinoid process, OS- Optic strut
a- Length of ACP, b- Basal width of ACP and c- Distance from the tip of ACP to OS
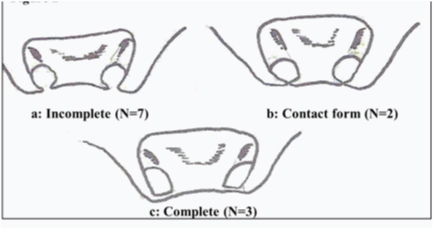
Presence of carotico-clinoid foramen was observed. If present, its type was classified as incomplete, contact form or complete according to the criteria given by Keyes, 1935 [9]. [Table/Fig-1,2].
Types of carotico-clinoid foramina.
a-Incomplete, b- Contact form and c- Complete
Statistical Analysis
SPSS version 17 was used for the statistical analysis. Paired t-test was applied to compare between right and left sides.
Results
Out of 27 skulls included, 13 were males and 14 were females. The average length of ACP ranged from 12 to 15mm on right side and 11 to 16mm on the left side. Paired t-test was applied to compare the means between the right and left sides. The width of ACP varied between right and left sides and this difference was statistically significant (p<0.05). The other dimensions did not show any difference between two sides.
The parameters of ACP were compared between males and females. The mean and standard deviations of these parameters are shown in [Table/Fig-3].
Descriptive statistics of the sample studied.
| Parametersmeasured (in mm) | Male (N=13) | Female (N=14) |
|---|
| Right | Left | Right | Left |
|---|
| Length of ACP | 12.07±1.77 | 12.46±1.39 | 12.21±1.69 | 12.28±1.62 |
| Width of ACP | 10.30±1.93 | 11.23±1.57 | 10.64±1.79 | 11.35±1.34 |
| ACP-OS | 13.46±1.21 | 13.84±1.29 | 13.28±0.95 | 12.85±1.30 |
Presence of bilateral carotico-clinoid foramina was observed in 5 skulls (3 males and 2 females). In one female and in one male skull the carotico-clinoid foramen was observed only on left side. Therefore a total of 12 carotico-clinod foramina were observed. Out of these, the most common type was incomplete (N=7) followed by complete (N=3) and contact form (N=2) [Table/Fig-4]. The frequency distribution of carotico-clinod foramina is given in [Table/Fig-4].
Frequency distribution of presence of carotico-clinoid foramina.
| Type of carotico-clinoid foramen | Male (N=13) | Female (N=14) |
|---|
| Right | Left | Right | Left |
|---|
| Incomplete | 2 | 1 | 1 | 3 |
| Contact form | 0 | 2 | 0 | 0 |
| Complete | 1 | 1 | 0 | 1 |
Discussion
The sella turcica is an important area, due to its anatomical relations with the cavernous sinus and its contents, sphenoid sinus and pituitary gland. In the superior approach to the cavernous sinus, radical removal of tumours amd paraclinoid aneurysms, complete or partial removal of the ACP is an important step. Removing the ACP in the presence of any abnormality in the anatomical structure of ACP combined with a completely ossified CCF, may have high risk. The major risk is injury to the ICA. Therefore, understanding the complex morphometric anatomy of ACP and knowledge of the type of ossifications of the carotico-clinoid ligament can be necessary to increase the success of surgery [8–10].
In a study done by Gupta et al., [11] the mean length of ACP on right and left side were 11.1±1.49mm & 11.61±2.07mm. A study done by Lee et al., [12] on Korean population, reported the average length as 9.26±1.43 and 9.09±1.67mm & a study by Gupta et al., [11] on Nepalese population reported 10.74±2.37mm, 9.91± 1.50mm on right and left side. A study by Kapur et al., [2] repored the average length of the ACP in males 9.9±1.6mm on right and 9.3±1.4mm on left. The length in females was 9.3±1.6mm right side and 8.9±2mm on left side. The present study reported higher values when compared to the values in the literature.
Study done by Kapur et al., [2] reported the mean value of ACP width in males on the right and left side as 9.4±1.4 and 9.1±1.7mm respectively. In females it was 8.7±1.5mm on right and 8.3±2.1mm on left. Gupta et al., [11] reported the basal width of ACP 9.62±2.36 and 9.66±1.27mm on right and left side respectively. In a Korean study by Lee et al., [12] the width of ACP was 9.97±1.58 and 9.29±1.39mm on right and left side respectively. The present study reported higher values when compared to the values in the literature. In the literature there are studies in which the thickness of ACP was measured (Kapur et al., Gupta et al., [2,11]. But in the present study the thickness was not considered.
The CCF is the result of ossification of caroticoclinoid ligament or of a dural fold extending between anterior and middle clinoid processes and ICA passes through it [1,13]. A study done by Gupta et al., [11] out of total 50 sides in 25 skulls examined, CCF was observed in 11 sides. Out of which complete foramen was observed in 6%and incomplete in 16%. In one skull bilateral complete CCF was observed. It was absent in 78% cases. In previous studies in the literature, occurrence of unilateral and incomplete CCF is relatively more common (8 to 35%) than bilateral and complete foramina (0.2 to 4%) [12,13]. The frequency of CCF has been observed as 9.9% in Japanese,15.7% in Koreans, 17% in Alaskan Eskimos, 23.4% in Sardinians, 34.84% in Caucasian Americans and 35.67% in Turks [14]. These morphometric documentation is helpful when dealing with vascular neoplastic or traumatic lesions of the sellaturcica or skull base regions [11].
In a study by Ozdogmus et al., [15] out of 100 CCF examined, in 27 sides, the carotico-clinoid ligament was completely ossified in 18 sides, and was incompletely ossified and in 55 sides it was a ligamentous structure. Deopujari et al., [3] studied 54 skulls, in which ossification between clenoid processes were observed in 16 skulls. Complete CCF was seen in 15.74% and incomplete in10.18%. Bilateral carotido-clenoid foramen was observed in 5 skulls (9.2%) and bilateral presence of osseous interclenoid ligament was seen in single skull only.
Hochstetter [16] and Kier [17] postulated that an osseous CCF was a developmental anomaly and showed its existence in the fetal and infant skulls. Further, of 120 adult and 45 prepubescent skulls examined by Lang [7], 12 had the completely ossified type of CCF, of which 9 were adult and 3 were juvenile. In one female and in one male skull the carotico-clinoid foramen was observed only on left side. Therefore a total of 12 carotico-clinod foramina were observed. Presence of bony CCF may cause compression, tightening or stretching of ICA. Surgical procedures involving cavernous sinus, ACP and optic canal become difficult in such cases. Therefore anatomical knowledge about the CCF is important for radiologist and surgeons.
Kapur et al., found that the optic strut was attached to the anterior fifth of ACP in 11.6% cases on the right side, and in 14.5% on the left. Its attachment to the anterior two fifths of the process was observed in 42% on the right side and 47.8% on the left side [2]. In the present study the distance was measured between the tip of ACP and medial end of OS which did not vary significantly between the sides and also did not show any significant gender differences. These parameters would be of surgical importance in preventing injury to ICA during the surgical procedures on cavernous sinus and suprasellar region.
Limitation
The sample size of the study was too small, that would be a hindering factor to generalize the hypothesis.
Conclusion
Considering the immense anatomical surgical and radiological importance of morphology of ACP, OS and CCF, this study highlighted the detailed morphometry of these structures. The study also has explained the sexual dimorphism in their morphology.
[1]. Soames RW, Skeletal System. Williams PL, Bannister LH, Martin MM et alGray’s Anatomy 1995 (38th ed)LondonChurchill Livingstone:547-84. [Google Scholar]
[2]. Kapur E, Mehi A, Anatomical variations and morphometric study of the optic strut and the anterior clinoid processBosn J Basic Med Sci 2012 12(2):88-93. [Google Scholar]
[3]. Deopujari R, Mangalgiri A, Kishore SD, Lata SK, Study of Ossification of carotido-clenoid ligament and interclenoid ligament in skulls of central India and its clinical implicationsIndian Journal of Forensic Medicine & Toxicology 2014 8(2):143-45. [Google Scholar]
[4]. Dutta AK, Essentials of Human Anatomy part-II 1999 (3rd ed)CalcuttaCurrent Books International:1-6. [Google Scholar]
[5]. Dolenc V, Direct microsurgical repair of intracavernous vascular lesionsJ Neurosurg 1983 58:824-31. [Google Scholar]
[6]. Yonekawa Y, Ogata N, Imhof HG, Selective extradural anterior clinoidectomy for supra-and parasellar processes: Tehnical noteJournal of Neurosurgery 1997 87:636-42. [Google Scholar]
[7]. Lang J, Structure and postnatal organization of heretofore uninvestigatedand infrequent ossification of the sellaturcica regionActa Anat 1977 99:121-39. [Google Scholar]
[8]. Walrath PT, Dana E, Jaroslav B, Reliability Test of the visual assessment of cranial traits for sex determinationAmerican Journal of Physical Anthropology 2004 125:132-37. [Google Scholar]
[9]. Keyes JEL, Observations on four thousand optic foramina in human skulls of known originArch Ophthalmology 1935 13:538-68. [Google Scholar]
[10]. Hunnargi S, Ray B, Pai SR, Metrical and non-metrical study of anterior clinoid process in South Indian adult skullsSurg Radiol Anat 2008 30:423-28. [Google Scholar]
[11]. Gupta N, Ray B, Ghosh S, A study on anterior clinoid process and optic strut with emphasis on variations of caroticoclinoid foramenNepal Med Coll J 2005 7:141-44. [Google Scholar]
[12]. Lee HY, Chung IH, Cnoi BY, Lee KS, Anterior clinoid process and optic strut in KoreansYonsei Med J 1997 38:151-54. [Google Scholar]
[13]. Rai AL, Gupta N, Anatomical variations of anterior clinoid process with its surgical importanceInnovative Journal of Medical and Health Science 2015 5:28-30. [Google Scholar]
[14]. Donald PJ, Surgery of the skull base 1998 PhiladelphiaLippincott-Raven:19-27. [Google Scholar]
[15]. Ozdogmus O, Saka E, Tulay C, Gurdal E, Uzun I, Cavdar S, The anatomy of caroticoclinoid foramen and its relation with the internal carotid arterySurg Radiol Anat 2003 25:241-46. [Google Scholar]
[16]. Hochstetter F, Über die Taeniainterclinoidea, di Commissuraalicochlearis und die Cartilago supracochlearis des menschlichen PrimordialkraniumsGegenbaurs Morph Jahrb 1940 84:220-43. [Google Scholar]
[17]. Kier EL, Embryology of the normal optic canal and its anomalies. An anatomic and roentgenographic studyInvest Radiol 1966 1:346-62. [Google Scholar]