Low back pain affects every population and is one of world’s foremost debilitating conditions. Low back pain is common musculoskeletal disorder and a global burden. Approximately 70% to 80% people have experienced low back pain at some point in their life. The annual prevalence of low back pain ranges from 15% to 45% but is largely dependent on population being studied and surveillance methods [1].
Major cause of low back pain leading to severe morbidity throughout the world affecting mainly the young working class population is lumbar disc prolapse. Authors have mentioned lifetime incidence of low back pain in range of 50-70% including sciatica among 40%, but clinically significant sciatica requiring special attention accounts for only 4-6% cases. Degeneration of disc due to various factors leads to prolapse of intervertebral disc into intervertebral foramina especially into L4-L5 and L5-S1 level. The L3-L4 & L2-L3 account for the majority of remaining prolapse. Since outcome of surgery depends on many factors, such as careful selection of patients, detailed clinical history, physical examination supported by relevant radiological investigations helps to differentiate disc prolpase from other causes of low back pain and sciatica [2].
Surgical removal of offending disc offers a simple and effective solution in management of severe sciatic pain and this method has established its position as reasonably safe procedure with satisfactory results in most of patients. Technique of fenestration for removal of offending disc has been used extensively for years since it is has certain advantages over commonly employed laminectomy technique. The traditional extensive laminectomy and discectomy went into disrepute because of extensive disruption of posterior stabilising structures of spine and its later complications [3].
Technique of fenestration discectomy is reputed to be less time consuming, with lesser blood loss, with few postoperative complications and it does not compromise stability of spine compared to laminectomy due to inherent minimally invasive nature of surgery [4].
Present study was conducted to determine extent of functional recovery (i.e. pain relief and return to work) and neurological recovery in patients with lumbar disc prolapse treated by fenestration technique and to determine significance of preoperative symptoms and neurological signs as determinants of outcome of fenestration technique.
Materials and Methods
From October 2010 to March 2012, 50 patients with signs and symptoms of prolapsed lumbar intervertebral disc who failed to respond to conservative treatment of minimum 6 weeks duration were studied prospectively. Patients with clinically and radiologically diagnosed lumbar disc prolapse with progressive neurological deficits or sensory or/and motor deficits or sciatica (unilateral or bilateral sciatica) failed to respond to conservative treatments were included in study. While patients with recurrent disc herniations, lumbar disc prolapse with discitis, evidence of lumbar canal stenosis, presence of any other associated spine pathology, previous history of any spine surgery, central disc prolapse or far lateral disc prolapse compressing nerve root in neural foramina as proved by MRI or other imaging modality were excluded from our study.
A detailed history with thorough clinical examination was done at time of admissions and all patients were subjected to Magnetic resonance imaging (MRI) [Table/Fig-1]. The results of imaging were correlated with physical findings and symptomatology of the patients. All clinicoradiologically proven cases were subjected to surgery. For preoperative analysis of employment status, light or sedentary work included lifting, pulling or pushing weight up to 8-10 kg, occasional lifting and/or carrying objects within weight limit, walking or standing for 2 hours in an 8 hour workday, retirement activities and household work while strenuous work was defined as lifting, pushing or pulling weight of 30-40 kg or greater and frequent lifting and carrying weight up to 20 kg during 8 hour work day.
Sagittal and axial T2W MRI images of L4-L5 disc prolapse.

All patients were operated in either knee chest position (n=25) or prone position (n=25) on bolsters under controlled general anaesthesia. A surgical procedure was carried out with standard prodedure of Fenestration technique at surgeon’s discretion. No disc space curettage was done.
Postoperatively patients were allowed up on first postoperative day. Gradual walking was encouraged but lifting weights, bending and stooping was prohibited for 6 weeks. Patients who were heavy labourers or long distance drivers were advised to modify their duties for 6 weeks. All patients were advised a regular postoperative back exercise program after 3 weeks. All patients were followed at regular intervals of 3 weeks, 6 weeks, 3 months and 6 months by either OPD visit or visit to their residence.
In our study preoperative semiquantative analysis of symptoms was done using ‘Back Pain Functional Score (BPFS)’ by Strafford et al., [5]. PROLO rating scale [6] was used to determine preoperative functional and economical status and outcome at final follow up. In PROLO scale [6], total score represents the sum of functional and economic scores. In order to identify physical signs from non organic signs and its impact on functional outcome, Wadell’s score [7] system was used. Result of surgery was evaluated with help of McNab’s criteria [8]. Statistical analysis was performed with statistical software (version 12.0 for windows, Chicago, Illinois) and data were evaluated by paired student t-test.
Results
In our study, out of 50 patients 28 (56%) were males and 22 (44%) were females. The average age was 37.96 years ranging from 24 -60 years. In clinical history, events which evoked low back pain were analysed and found out that 36 (72%) patients had insidious onset, history of lifting heavy weights in 12 (24%) patients and 2 (4%) patients had fall on back. Out of all cases, 22 (44%) cases were heavy duty labourers while remaining 28 patients had light work.
Most of cases i.e. 34 (68%) cases had history of low back pain preceding sciatica while remaining cases i.e. 16 (32%) cases had low back pain and sciatica started simultaneously. No patient had only sciatica as only symptom. Mean duration of low back pain was 6.5 months with range from 20 days to 18 months while radicular pain was present on average for 2.5 months. Major cases had unilateral radicular pain either on left or right side. Out of all patients, 23 (46%) cases had left sided sciatica while remaining had right sided sciatica. Low back ache and radicular pain were most common symptoms of patients with prolapsed disc. Other important neurological symptoms include parasthesia in dermatomal region (n= 34, 68%), weakness in myotomal region (n=26, 52%) and reduced sensation over dermatomal region (n=18, 36%).
Thorough clinical examination revealed that Straight leg raising test (SLRT) was found to be positive in all patients in range of 30° to 60° while Cross SLRT which is highly sensitive to diagnose root tension was positive in 16 (32%) cases. Most of cases i.e. 44 (88%) cases had telltale sign of disc prolapse in form of loss of lumbar lordosis. Out of 50 cases, 8 (16%) patients had functional scoliosis (sciatic list) due to nerve root irritation [Table/Fig-2]. Lasegue’s test which was a progression of SLRT was positive in all cases. During clinical examinations, deep tendon reflexes were unaltered in 42 (84%) cases with L4-L5 disc prolpase while it was hypo ankle reflex, present in all cases having L5-S1 (n=7, 14%) presentation and hypo knee reflex in 1 (2%) case [Table/Fig-3]. Preoperative motor deficits were present in 26 cases (52%), which had some form of muscle weakness according nerve root involvement as graded by Medical Research Council (MRC) scale. Progressive neurological involvement is one of criteria for surgical management in cases with lumbar disc prolapsed [Table/Fig-4].
Preoperative sciatic list (Functional scoliosis) in a lumbar disc prolapse case and Postoperative relief of sciatic list.

Frequency of preoperative clinical findings of lumbar disc prolapsed.
| Preoperative Signs | Frequency (n= 50) | Percentage |
|---|
| Positive SLR test | 50 | 100% |
| Crossed SLR test | 16 | 32% |
| Paraspinal Muscle Spasm with Obliterated Lumbar Lordosis | 44 | 88% |
| Sciatic List | 08 | 16% |
| Restricted Spinal movements | 36 | 72% |
| Sensory Deficits | 18 | 36% |
| Motor Deficits | 26 | 52% |
| Deep Tendon Reflex abnormalities- Ankle Jerk | 08 | 16% |
| Hypo responsive Knee jerk | 01 | 02% |
Preoperative motor deficits in patients studied.
| Motor Deficits | Frequency (n) | Percentage |
|---|
| Nil Deficits | 24 | 48% |
| Present | 26 | 52% |
| Left sided deficits | 12 | |
| Peroneals Grade - 4/5 | 04 | |
| EHL Grade - 4/5 | 04 | |
| EHL & FHL Grade – 4/5 | 02 | |
| EHL – 3/5 | 02 | |
| Right sided deficits | 14 | |
| EHL Grade -4/5 | 08 | |
| EHL and EDL – 4/5 | 03 | |
| EHL – 3/5 | 02 | |
| Quadriceps/Hip adductors – 4/5 | 01 | |
*EHL- extensor halluscis longus, EDL – Extensor Digitorum longus, FHL – Flexor Halluscis Longus
According to our inclusion criteria, all cases in our study were unilateral posterolateral herniartions. On MRI, most of cases were L4-L5 prolapse i.e. 42(84%) patients, 7 (14%) patients had L5-S1 prolpase and 1(2%) had L3-4 prolapse. At time of surgery, inspection of herniation of disc was done and classified accordingly into protrusion, extrusion and sequestrated [Table/Fig-5].
Type of a prolapse of lumbar intervertebral disc in present study.
| Type of Prolapse | Frequency (n = 50) | Percentage |
|---|
| Protrusion | 12 | 24% |
| Extrusion | 36 | 72% |
| Sequestration | 02 | 04% |
Average duration of surgery was approximately 75 minutes with average blood loss of 150 mL ranging from 100 mL to 250 mL. Average duration of hospital stay for patients was 3 days postoperatively. We experienced complications in 4 (08%) cases, among them 1 had dural tear which was primarily repaired at a time of surgery while 3 (6%) cases had superficial wound infection which was treated well with debridement and intravenous antibiotics.
In our study, 42 (84%) cases abandoned or left their job temporarily while remaining 8 (16%) cases were women who continued their job as they required doing daily household chores. Duration of unemployment varied from 20 days to 9 months with mean period of unemployment was around 3.7 months.
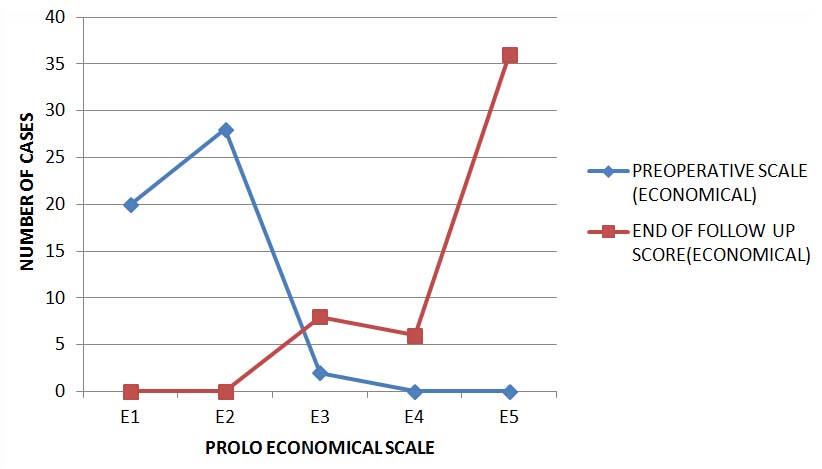
According to Back Pain Functional Scale by Strafford et al., which is a semi-quantitative scale of functional status of patients by asking multiple questions, good results were found in 42 (84%) cases, fair result in 8 cases (16%) and none with poor results at follow up of six months [Table/Fig-6]. Total outcome score for PROLO scale after 6 months was derived for every patient according to their individual economical (E) and functional (F) PROLO score in which E1 reveals worst economic score and E5 best economic score as well F1 worst functional score and F5 best functional score {For example, total PROLO score for a patient with Economical score E4 and Functional Score F5 will be E4+F5 =9 (4+5=9)}. So according to PROLO scale, it was found that 42 (84%) patients had good results while fair result was consistent with 8(16%) cases without any poor results [Table/Fig-7&8] Even McNab’s criteria showed good results in 84% (n=42) cases and fair result in 16% (n=8) cases.
Back pain functional scale outcome in patients studied.
| Back Pain functional scale Outcome(Strafford et al) | Frequency | Percentage |
|---|
| Good (Mean score 0-10) | 42 | 84% |
| Fair (Mean score -11-20) | 08 | 16% |
| Poor (Mean score 21 & >21) | 00 | 00 |
Comparison between preoperative and end of follow up (economical) PROLO scale.
| PreoperativePROLO scale(Economic) | End of Follow up PROLO scale (Economic) | Percentage |
|---|
| E 1(n = 00) | E2(n= 00) | E3(n= 08) | E4 (n=06) | E5(n= 36) | % |
|---|
| E 1 (n = 20) | 00 | 00 | 06 | 04 | 10 | 40% |
| E2 (n= 28) | 00 | 00 | 02 | 02 | 24 | 56% |
| E3 (n= 02) | 00 | 00 | 00 | 00 | 02 | 04% |
| % | 00 | 00 | 16% | 12% | 72% | 100% |
*E1 – Completely Invalid, E2- No gainful occupation including ability to do house chores or retirement activities, E3 – Able to work but not at previous vocation, E4- Working at previous occupation with part time or limited status, E5- Able to work at occupation with no restriction.** Data is tabulated as economical scale followed by number (n) of cases belonging to that scale
Comparison between preoperative and end of follow up (Functional) PROLO scale.
| PreoperativePROLO scale(Functional | End of Follow up PROLO scale (Functional) | Percentage |
|---|
| F 1(n = 00) | F2(n= 00) | F 3(n= 06) | F4 (n=06) | F5(n= 38) | % |
|---|
| F1 (n=14) | 00 | 00 | 06 | 02 | 06 | 28% |
| F2 (n=32) | 00 | 00 | 00 | 02 | 30 | 64% |
| F3 (n=04) | 00 | 00 | 00 | 02 | 02 | 08% |
| % | 00 | 00 | 12% | 12% | 76% | 100% |
*F1- Total incapacity, F2- mild to moderate level back pain or sciatica (or pain same as before operation and able to perform all daily chores), F3 – low level of pain and able to perform all activities except sports where applicable), F4- No pain but patient had one or more recurrences of low back pain or sciatica, F5- Complete recovery, no recurrent episodes of low back pain, able to perform all previous activities, including sports where applicable. ** Data is tabulated as Functional scale followed by number (n) of cases belonging to that scale.
Comparison of preoperative and end of follow up PROLO score revealed improvement in functional and economical outcome [Table/Fig-9&10]. According to PROLO economical scale, 36 (72%) cases were able to work at their previous job without any recurrences while 6 (12%) were able to work at previous occupation but part time or limited status while 8 (16%) cases were able to work but had to abandon their previous occupation.
Graphical presentation of progressive improvement of preoperative PROLO scale (economical).
Graphical presentation of progressive improvement of preoperative PROLO scale (Functional).
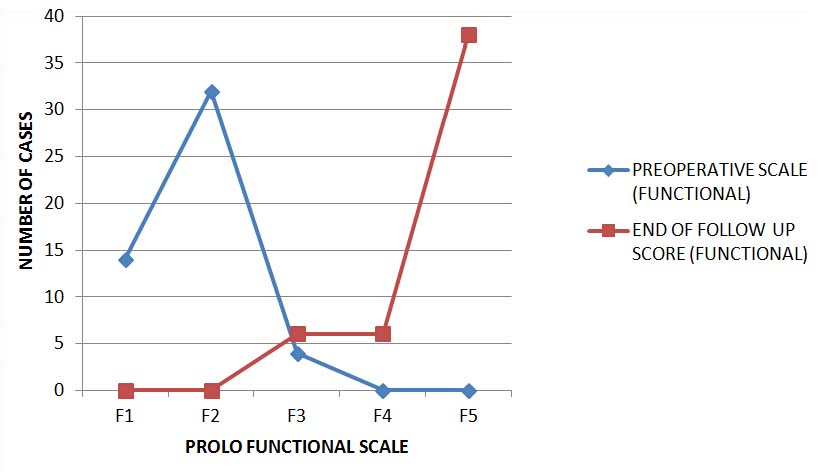
Thus, 84% cases were able to join their previous occupation at end of six months. Similarly, according to PROLO functional scale, 38 (76%) cases had complete relief of back/radicular pain while 6 (12%) had no continuous pain but experienced one or two episodes of recurrence of back/radicular pain while remaining 6 (12%) cases had low level of pain but were able to perform all day to day activities except sports/strenuous activities. Thus, in around 76% cases of lumbar disc prolapse operated by fenestration technique had complete relief of pain.
To assess psychoanalysis of a patient for low back pain Wadell’s non organic signs were analysed to separate physical signs from non organic signs. In our study 7 (14%) out of 8 patients with high Wadell’s score (i.e. 3 or more signs) were women. While correlating Wadell’s non organic signs with overall results of patients studied, it was seen that fair results were more common with Wadell’s non organic score of >3 signs than that of good results, suggesting Wadell’s non organic score >3 is associated with less satisfactory results (p= 0.016) as multiple psychosomatic factors plays role in functional outcome of surgery.
Correlation of outcomes among patients with and without motor and sensory deficits respectively were not significant with p-values of 0.593 and 0.776 respectively, confirming that preoperative motor or sensory deficit does not affect postoperative functional outcome. However, correlation between age and functional outcome revealed that age is statistically associated with outcome (p= 0.089), showing more good results among patients with age less than 30 years. Even correlation of duration of symptoms with overall outcome of patients studied showed moderately significant p-value (p =0.098+) thus it can be inferred that patients having duration of symptoms less than 6 months showed better functional outcome than those patients which presented after span of 6 months. The variables like sex, duration of unemployment, level of disc prolapse, pattern of work had no correlation with functional outcome.
Discussion
Back pain due to lumbar intervertebral disc prolapse contributes to chunk of problems related to back pain. The lumbar disc disease though not contribute to mortality, it contributes to morbidity and economic loss due to number of work hours lost. Prolapsed intervertebral disc occurs in about 5-10% of all backache patients and is a common cause of sciatica. Even a small prolapsed disc in the presence of a narrow spinal canal can lead to compression of cauda equina and its roots. Mainstay treatment of lumbar disc prolapse has been removal of disc i.e. discectomy, though methods of discectomy differs. Authors have reviewed that traditional wide laminectomy produced increased morbidity compared to less extensive procedures like inter-laminar fenestration [9]. The end point of assessment of any therapeutic modality is functional outcome, because that is what matters to the patients. Lumbar disc disease being a benign condition and pain is predominant factor limiting the activities of the patient, it is anticipated that after the therapy, the patient should have good functional outcome and go back to premorbid state. However, the fact is that the good outcome varies from 49-90% in different studies. This only implies that there should be many factors which influence the outcome [7].
It is therefore clinician’s task to properly select the patients for surgery with appropriate indications, who are expected to have symptomatic relief, with limited risk and least possible expense. According to Manohara B et al., functional outcome of fenestration discectomy results were as good in 90% patients, fair in 6.2% patients and poor in 3.8% cases while our study showed good results in 84% cases while fair results in 16% cases without any poor results [8]. Similarly, Nahar et al., showed good to excellent results in 80.42% cases, fair results in 17.2% and poor results in 2.17% cases [10]. While Garg et al., observed good results among 86% cases while fair results in 12% and poor results in 2% cases [11]. This variation in studies may be due to different selection criteria of patients.
Various authors have suggested 66.67% to 90% [2,3,8–12] cases have returned to their original vocation which agrees well with our study with 84% cases returning to their own vocation without any limitations at end of 6 month follow up. Whereas, multiple authors [2,3,9,10] have quoted 64% to 92% cases had complete relief of pain after fenestration discectomy, while our study observed 76% cases had complete leg and back pain relief.
According to Schoenfeld, increasing age was an important negative predictor which agrees well with our study too. As reported elsewhere, preoperative occupational workload is known to influence surgical outcome and residual symptoms significantly, with patients engaged in heavy manual work having significantly more functional disability compared with those engaged in light or medium-strenuous work [13]. General consensus has been that heavy work caused flexion–extension and torsional movements at lumbar spine, increasing load and shear forces on the spine leading to facet joint injury and disc degeneration. However, few studies mentioned no obvious relationship between occupational workload and clinical outcome; may be due to different methods to classify workload and quantify outcome [14].
Several factors like age < 41-year-old; male-sex; duration of sciatica < 7 months; no previous lumbar surgery have been reported as predictive of a successful outcome following lumbar discectomy. While unsatisfactory surgical outcome is seen in patients with preoperative leg pain associated with lumbar disc herniation for > 8 months due to the fact that patients were unable to return to their previous work status. Authors have noted that duration of severe preoperative symptoms in the their study had a significant impact on clinical outcome as long duration of symptoms resulted in more severe nerve root lesions and poorer outcomes than a short duration of symptoms [14]. Our prospective study seems to agree with above mentioned findings.
On comparing fenestration with laminectomy, as described by Nahar et al., and Nagi et al., fenestration had the added advantages of less surgical time and intraoperative blood loss, rapid convalescence, minimal risk of instability and they seldom landed up to post- operative complications like adhesions and arachnoiditis [11,15].
According to Sangwan et al., microdiscectomy exposure differs from fenestration approach only in its extent. The disc removal per se in both is limited. When a protruded disc herniation was identified incision in annulus fibrosus is essential. Fenestration technique has the advantage of correcting lateral recess stenosis also due to additional exposure. If surgeon thinks that the nerve root remains tight even after disc excision, he/she must be prepared to perform foraminotomy or undercutting of upper or lower lamina in addition to lumbar discectomy [9].
Thus, results of this study states that the lumbar discectomy performed with a limited disc excision by fenestration is a safe, effective and reliable method for treating selected patients with herniated lumbar discs.
Limitation
However, this study has limitations. Our study had short term follow up so we were not in position to comment on long term follow-up of same patients. Moreover, our study did not compare its results with latest technique of microdiscectomy which is a promising less invasive technique to treat same condition. Also, our study did not provide in depth insight into psychological factors affecting functional outcome of surgery.
Conclusion
Our study concludes that fenestration technique of lumbar discectomy is a simple and reliable method for treatment of meticulously selected lumbar disc prolapse patients having advantages of less morbidity, low blood loss, inexpensive and devoid of spinal instability. Functional outcome of fenestration technique in terms of return to work and complete pain relief at end of six months had been satisfactory in our study. Moreover, significance of preoperative pain and neurological signs were important for diagnosis of lumbar disc prolapse but they play none role as determinants of functional outcome. Moreover, old age, long duration of symptoms and presence of multiple psychological issues are negative predictors of functional outcome. In addition to that, motor deficits were recovered early in our study than sensory and reflex conversions.
*EHL- extensor halluscis longus, EDL – Extensor Digitorum longus, FHL – Flexor Halluscis Longus
*E1 – Completely Invalid, E2- No gainful occupation including ability to do house chores or retirement activities, E3 – Able to work but not at previous vocation, E4- Working at previous occupation with part time or limited status, E5- Able to work at occupation with no restriction.** Data is tabulated as economical scale followed by number (n) of cases belonging to that scale
*F1- Total incapacity, F2- mild to moderate level back pain or sciatica (or pain same as before operation and able to perform all daily chores), F3 – low level of pain and able to perform all activities except sports where applicable), F4- No pain but patient had one or more recurrences of low back pain or sciatica, F5- Complete recovery, no recurrent episodes of low back pain, able to perform all previous activities, including sports where applicable. ** Data is tabulated as Functional scale followed by number (n) of cases belonging to that scale.