Digital Mammography in Young Women: Is a Single View Sufficient?
Johannes Gossner1
1 Faculty, Department of Clinical Radiology, Evangelisches Krankenhaus Göttingen- Weende, An der Lutter 24, 37024 Göttingen, Germany.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Johannes Gossner, Faculty, Department of Clinical Radiology, Evangelisches Krankenhaus Göttingen- Weende, An der Lutter 24, 37024 Göttingen, Germany.
E-mail: johannesgossner@gmx.de
Correction:
This article has been updated on 1 May 2016, to see correction please see link which is given below:
http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2016&volume=10&issue=5&page=ZZ01&issn=0973-709x&id=7970
Introduction
Single view mammography may be a less time consuming, more comfortable and radiation reduced alternative for young women, but there are no studies examining this approach after the implementation of digital mammography into clinical practice.
Materials and Methods
Retrospective analysis of all mammographies performed in women younger than 40 years during a 24 month period. The sample consisted of 109 women with 212 examined breasts. All patients initially received standard two- view mammography. In the study setting the MLO- views were read by a single viewer and compared to a composite reference standard.
Results
In this sample 7 malignant findings were present and the review of the MLO-view detected 6 of them (85%). In patients with dense breasts 4 out of 5 malignant findings were found on the single-view (sensitivity 80%) and all 2 malignant findings were detected in patients with low breast density (sensitivity 100%). There were 7 false positive findings (3.3%). i.e. in total 8 out of 212 examined breasts were therefore misinterpreted (3.8%).
Conclusion
Single view digital mammography detects the vast majority of malignant findings, especially in low density breast tissue and the rate of false-positive findings is within acceptable limits. Therefore this approach may be used in different scenarios (for example in increasing patient throughput, in resource poor settings, reducing radiation burden in the young or in combination with ultrasound to use the strengths of both methods). More research on this topic is needed to establish its potential role in breast imaging.
Breast cancer, Digital mammography, Diagnostic performance
Introduction
Despite exiting new developments in breast imaging (for example tomosynthesis or contrast-enhanced mammography) mammography still is the imaging of choice in suspected breast disease and breast cancer screening [1]. Usually mammography is performed using two views: a mediolateral-oblique (MLO) view and a cranio-caudal (CC) view. Single-view mammography, i.e. using only the MLO-view, has been used in the early days of screening, but this approach has been left because of an inferior sensitivity and a higher recall rate compared to two-view mammography [2]. Theoretically single-view mammography offers three major advantages. With only one view less radiation is applied to the patient, this is especially important in young women, who are known to be more sensitive to radiation [3]. The examination speed is increased. And, as compression is uncomfortable for a large portion of patients, obtaining only one view per side may increase comfort of the examination [4], i.e. single view mammography, if feasible, may be a less time consuming, more comfortable and radiation reduced alternative for young women. This single-view approach has been studied in the 80s and early 90s. To the best of our knowledge, there are no studies examining this approach after implementation of digital mammography into clinical practice. Therefore its usefulness is unclear.
Aim
In this retrospective study the diagnostic performance of a single-view digital mammography (MLO) view is evaluated and possible clinical usefulness is discussed.
Materials and Methods
A retrospective study was performed; this study type is in accordance with the statue of the ethics committee of the affiliated University of Göttingen. All patients gave their written consent, that their data, in anomymized form, can be used for study purposes. All mammographies performed in women younger than 40 years during a 24 month period (April 2013-March 2015) at the Department of Clinical Radiology at Göttingen-Weende Hospital were searched and included in the study. All patients included in the study received a standard two-view mammography (MLO/ CC-view). Patients were imaged because of clinical findings (pain, palpable mass) or were imaged as part of an individualized screening strategy because of a family history of breast cancer. The sample consisted of 109 women with 212 examined breasts. All mammographies were performed by board certified radiographers subspecialized and certified in mammography (mammographers). All women received standard two views (MLO/ CC) using digital radiography (Fuji Profect Plus, Fujifilm Cooperation, Tokyo, Japan) with a standard mammography unit (Siemens Mammomat 3000 Nova, Siemens Healthcare, Erlangen, Germany). Additional views were obtained, if found necessary by the reporting radiologist. Images were initially printed out on hard copies and examined on a standard view box. The mammographies were initially interpreted by two board certified radiologist with experience of 8 and 25 years in breast imaging.
Breast density was determined in accordance to the proposed classification of the ACR (American College of Radiology) into 4 categories (type A: almost entirely fatty/ type B: scattered areas of fibroglandular density/ type C: heterogenously dense/ type D: extremely dense) [5]. For the single view-apporach the MLO-view was chosen, because it usually shows the entire gland including the axillary tail. To test the diagnostic performance of a single-view approach in the study setting the MLO-views of the patients were read again by a single viewer (the author) and pathological findings were noted (architectural distortion, mass, pleomorph calcifications). The reader was blind to the initial results. This second reading was performed on a medical workstation using the departemental PACS (synedra aim 3.4 “Triton”, Synedra Information technologies, Innsbruck, Germany). The findings of this second reading, of the MLO-view only, were compared to the composite reference standard (including the initial report of the two-view mammography and, if available, operative and pathological findings as well as results of other diagnostic tests like ultrasound or follow-up examinations). Initially all findings were reported according to the BIRADS (Breast Imaging Reporting And Data System). For this study the initial findings were dichotomized into no malignancy versus suspect of malignancy. The sensitivity of single-view versus the composite reference standard was calculated. Sensitivity was also compared between women with low breast density (type A/B) and dense breasts (type C/D). A descriptive statistic was performed. Because of the small number of pathological findings only a descriptive statistic was performed.
Results
In this sample 7 malignant findings were present using the reference standard. Single-view mammography, i.e. only the MLO-view, detected 6 of them [Table/Fig-1]. The sensitivity for the single-view approach was therefore 85% for malignancy. In patients with dense breasts 4 out of 5 malignant findings were found on the single-view (sensitivity 80%) and all 2 malignant findings were reported in patients with low breast density (sensitivity 100%). Seven false positive findings were found on the single-view (3.3%). i.e. in total 8 out of 212 examined breasts were therefore misinterpreted (3.8 %).
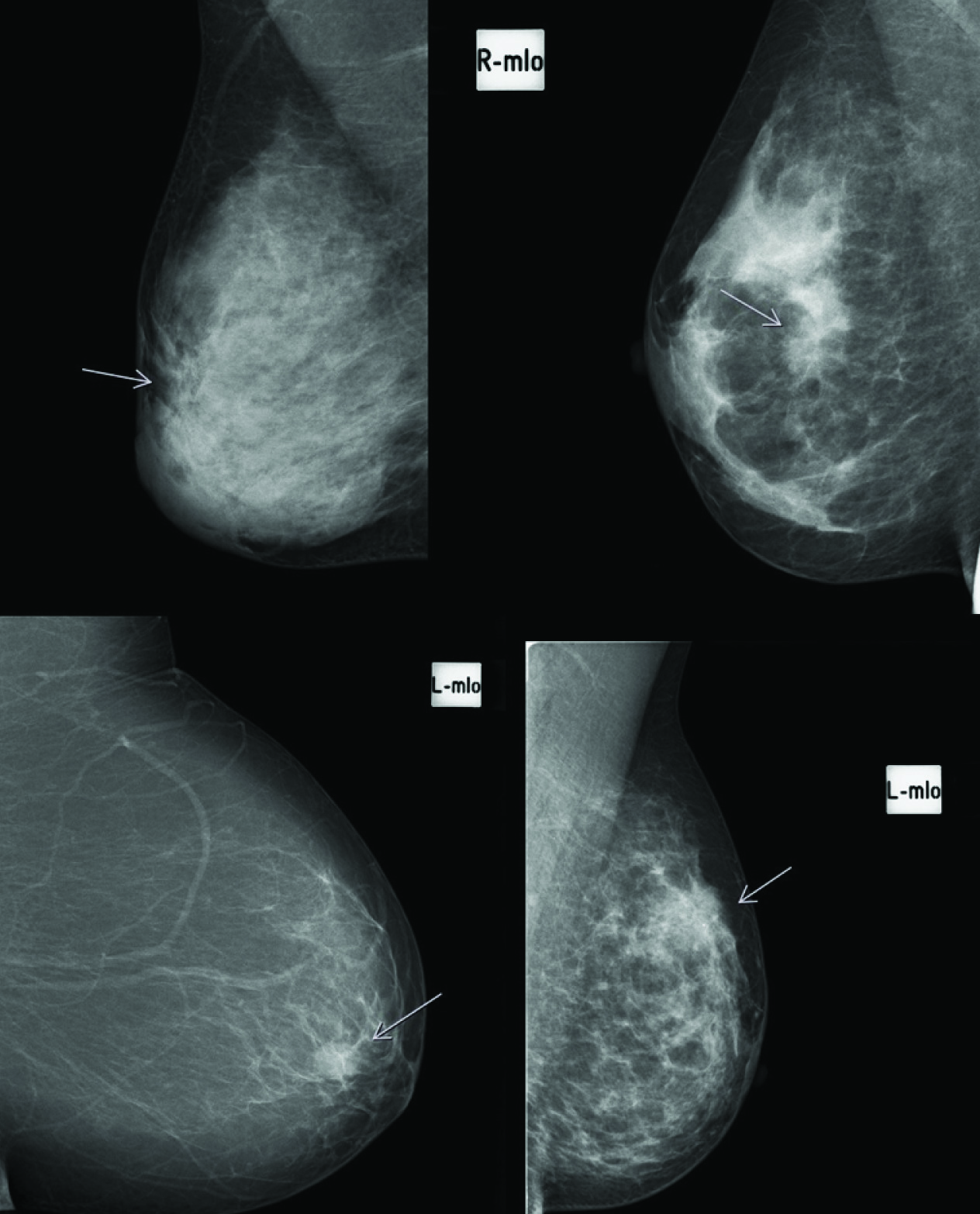
A compilation of mammographic images (MLO-views) of four different patients with breast cancer detectable on the single-view (arrows).
Discussion
In this study single-view mammography (i.e. the MLO-view only) detected all but one of the malignant findings (85%). This is in accordance to the findings of Sickles et al., who detected 25 out of 27 cancers on a large sample of 2500 baseline mammographies using a single view (92.6%) [2]. Taking the small sample size into account sensitivity for this approach seems to be equal for film-screen and digital mammography. But like other studies the single-view approach shows a reduced sensitivity for breast cancer reduction, this has always to be kept in mind in the discussion of possible clinical scenarios [2,6,7]. In the literature digital mammography is usually found to be superior in denser breasts, but the limited number of patients in this feasibility study precludes statistic valuable comparisons [8]. In another analysis of different imaging strategies (single-view vs. two-view mammography) sensitivity of a malignant lesion was 83% using a single-view vs. 84% using standard two-view mammography [9]. Nonetheless every malignant finding is a reason for concern. In our study one cancer may have been missed, if only a single view mammography would have been performed. In the missed case an architectural distortion and asymmetry could be found in the MLO-view, but the cancer was easily detectable on the CC-view and sonography. Clinically there was a clearly palpable lesion. This phenomenon has been reported by Hackshaw et al., [6]. In their detailed analysis of 110 pathological mammographies with breast cancers 87 were detected in the study setting using the MLO-view only, i.e. sensitivity was 79%. Interestingly after consensus only 3 cancers did not show any abnormality on the MLO-view. Undetected cancers on the single-view were usually small or consisted of architectural distortion or soft tissue asymmetry. Cancers showing malignant calcifications or presenting as a mass were usually detectable using one view. In our study sensitivity was better in patients with low breast density (100%) compared to patients with dense breast parenchyma, in our opinion this reflects the inherent weaknesses of mammography in patients with denser tissue. In contrast, Hackshaw et al., did not report any significant correlation between cancer detectability and tissue density [6]. The reduced sensitivity of a single-view approach lead to a change in screening programs in most country, who changed to the use of standard two-view-mammography [6,7].
We also found false positive findings in 3.3% of patients. The higher number of false-positive findings with single-view mammography has been reported in the literature. In the study of Sickles et al., the rate of false-positive findings was as high as 18.5% [2]. This observed reduction of false positive findings with digital mammography compared to film-screen mammography has been reported by Sala et al., [10]. While a false positive-rate of 18.5% is very high and is questioning the value of a single-view approach, we think that the observed small number of false-positive findings with digital mammography is within acceptable limits. In the large UKCCCR study single-view mammography resulted in 15% more women recalled for further views (8.16 % using a single-view vs. 6.97 % using standard two-view mammography) [7]. This shortcoming may be easily solved in daily practice, if all mammographies are instantly reviewed by a radiologist, who decides if further views are necessary.
Given the above mentioned results and keeping the reduced sensitivity in mind there are different potential scenarios for the use of single view mammography. In resource poor settings the inferior sensitivity may be accepted to get more women examined. There are no published evaluations comparing the examination time of a standard two-view mammography in contrast to a single-view mammography. In our department we are planning around 15 minutes per women (5 minutes for explanation and preparation, 5 minutes for the MLO-views, 5 minutes for the CC views including the reading and archiving of the pictures), i.e. in one hour around 4 women can be examined with a standard two-view mammography. In contrast, one might estimate that 6 women may be examined using a single-view mammography, accounting for a 50% increase in examined patients. In this setting the attendance of the reporting radiologist is favourable to decide immediately on additional views to minimize the recall rate. Another possible scenario is to cancel the second (CC-view) in patients with low density parenchyma after having obtained the MLO-view first. To optimize the work-flow in this setting the judgment of breast density and the decision to cancel the second view may be delegated to the radiographer. It has been shown that after a dedicated 6 months training radiographers can interpret mammographies with high sensitivity for cancer detection; therefore it should be feasible to train mammographers for the correct judgment of breast density [11]. Another opportunity is to obtain standard two-view mammography in a screening setting at the first examination followed by a single-view mammography in subsequent examinations. The single-view mammography may be combined with ultrasound to combine the strengths of both examination techniques. This may be an almost perfect solution as in one study the combination of a single view mammography and an ultrasound showed a sensitivity of 97% for the detection of a malignant disease [7].
Limitation
The main limitation of this study is the small sample size and the single reader in the study setting. Therefore, only a small number of malignant findings were evaluable limiting the generalizability of the findings. But this small feasibility study shows the potential value of digital single-view mammography and may renew the research interest on this topic. Larger studies with more than one reader and in women of different ages are needed until the true value of a single-view mammography approach can be finally assessed. Given the findings above in our department we started to skip the second view in young women with a low likelyhood of breast cancer and low density breast tissue undergoing imaging before breast reduction surgery. In patients with fear of radiation we sometimes use a combination of a single MLO-view with ultrasound. But in the patient with a palpable mass we strongly suggest the use of a standard two-view mammography because of the superior senstivity for breast cancer detection.
Conclusion
Digital single-view mammography (MLO-view) detects the majority of malignant findings, especially in low density breast tissue. This single-view approach may have advantages in different scenarios (for example in increasing patient throughput in resource poor settings or in reducing radiation burden in the young) or may be combined with ultrasound to use the strengths of both methods. This small feasibility study shows the potential value of digital single-view mammography and, hopefully, renews the research interest on this topic. More research is needed to establish the potential role of digital single-view mammography in breast imaging.
[1]. Patterson SK, Roubidoux MA, Update on new technologies in digital mammographyInt J Womens Health 2014 6:781-88. [Google Scholar]
[2]. Sickles EA, Weber WN, Galvin HB, Baseline screening mammography: one vs. two views per breastAJR 1986 147:1149-53. [Google Scholar]
[3]. Berrington de Gonzales A, Berg CD, Visvanathan K, Robson M, Estimated risk of radiation-induced breast cancer from mammographic screening for young BRCA mutation carriersJ Natl Cancer Inst 2009 101:205-09. [Google Scholar]
[4]. Clark S, Reves PJ, Women’s experiences of mammography: A thematic evaluation of the literatureRadiography 2015 21:84-88. [Google Scholar]
[5]. Zonderland H, Smithuis R. BI-RADS for mammography and ultrasound 2013. Published October 8, 2014, http://www.radiologyassistant.nl [Google Scholar]
[6]. Hackshaw AK, Wald NJ, Michell MJ, An investigation into why two-view mammography is better than one-view in breast cancer screeningClin Radiology 2000 55:454-58. [Google Scholar]
[7]. Wald NJ, Murphy P, Major P, UKCCR multicenter randomized controlled trial of one and two view mammography in breast cancer screeningBMJ 1995 311:1189-94. [Google Scholar]
[8]. Sala M, Domingo L, Macia F, Does digital mammography suppose an advance in early diagnosis? Trends in performance indicators 6 years after digitalizationEur Radiol 2015 25:850-59. [Google Scholar]
[9]. Weining C, One-view mammography combined with ultrasound-mammography versus two-view mammography for the examination of the female breast. New concept for early detection of breast cancerThesis, University of Tübingen 2004 [Google Scholar]
[10]. Sala M, Salas D, Belvis F, Reduction in false-positive results after introduction of digital mammography: analysis from four population-based breast cancer screening programs in SpainRadiology 2011 258:388-95. [Google Scholar]
[11]. Torres-Meija G, Smith RA, de la Luz Carranza-Flores M, Radiographers supporting radiologists in the interpretation of screening mammography: a viable strategy to meet the shortage in the number of radiologistsBMC Cancer 2015 15:410 [Google Scholar]