Bilateral Painful Ophthalmoplegia: A Case of Assumed Tolosa-Hunt Syndrome
Ilko Kastirr1, Peter Kamusella2, Reimer Andresen3
1 Medical Assistant, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
2 Medical Specialist, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
3 Head of Department, Institute of Diagnostic and Interventional Radiology/Neuroradiology, Westküstenklinikum Heide, Academic Teaching Hospital of the Universities of Kiel, Lübeck and Hamburg, Germany.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ilko Kastirr, WKK Heide Radiologie, Esmarchstraβe 50, 25746 Heide, Germany.
E-mail: ikastirr@wkk-hei.de
We present the case of a man of 47 years with vertical and horizontal paresis of view combined with periorbital pain that developed initially on the right side but extended after 3-4 days to the left. Gadolinum uptaking tissue in the cavernous sinus was shown by MRI of the orbital region in the T1 spin echo sequence with fat saturation (SEfs) with a slice thickness of 2 mm. As no other abnormalities were found and the pain resolved within 72 hours of treatment with cortison a bilateral Tolosa-Hunt Syndrome (THS) was assumed. THS is an uncommon cause for Painful Ophthalmoglegia (PO) and only few cases of bilateral appearance have been reported. Even though the diagnostic criteria for THS oblige unilateral symptoms we suggest that in patients with bilateral PO THS should not be excluded as a differential diagnosis. Further more when using MRI to detect granulomatous tissue in the orbital region the chosen sequence should be T1 SEfs and slice thickness should possibly be as low as 2 mm, as granulomas are often no larger than 1-2 mm.
Brain-MRI, Cavernous sinus granuloma, Cranial nerve paralysis, Headache, Ophthalmoplegia dolorosa
Case Report
A 47-year-old caucasian man was admitted to the emergency room after presenting himself to the ophthalmologists practice with first appearance of diplopia and right periorbital pain as well as impaired stereopsis that had started 2-3 days earlier.
During the neurological examination he presented diplopia of the right eye without explicit eye muscle paralysis. Other than that he was fully oriented and responded adequately without signs of meningitis or deficit of sensibility, coordination or muscle movement. Babinsky signs were negative. While in the emergeny room he showed normal vital parameters. The blood analysis showed normal erythrocyte sedimentation rates, levels of CRP and TSH were normal. The rheumatoid factor (22.2 IU/ml) and ANA (1:20) were slightly elevated while ACE, AMA, ANCA, PR3 and antibodies against MPO were negative. Searching for specific infections the analysis was negative for antibodies against aspergillus, listeria and coxsacie virus. The liquor analysis was without pathological findings with 5 cells /3, total protein of 32 mg/dl, glucose concentration of 62 mg/dl and lactate level of 1.4 mmol/l. The medical history of the patient included hypertension, obesity and penicillin allergy.
An initial head CT showed no signs of intracerebral bleeding and the patient was admitted to the Stroke Unit with suspected anaemic brain stem infarction. MRI of the head with and without contrast agent with a slice thickness of 4 mm in the T1 SE sequence without fat saturation was negative for signs of ischaemia, space-consuming lesions or a focus of infection, no granulomas in the cavernous sinus were detected. The doppler-sonograph of the extracerebral vessels showed no wall abnormalities and chest x-rays were normal. Aneurysm and dissection were excluded by an CT angiography.
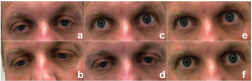
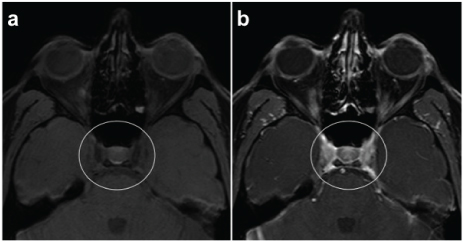
During the following 24 hours the patient rapidly developed strong retroorbital pain accompanied by vertical and horizontal paresis of view and convergence on both sides as well as ptosis of the right eye [Table/Fig-1]. The following MRI of the orbita with 2 mm slice thickness showed in the T1 SEfs sequence a tissue proliferation in the sinus cavernosus that showed strong Gadolinum DTPA uptake in the enhanced sequence [Table/Fig-2]. Suspecting a bilateral Tolosa-Hunt Syndrome the patient was treated with 100mg of cortison per day.
Clinical examination of eye movement and convergence: a) relaxed eye position; The patient was asked to b) focus on the close fingertip of the examiner; c) look up; d) look down; e) look to the right; and f) look to the left.
T1SEfs of the orbital region in 2 mm slice thickness: a) without and; b) after application of Gadolinum DTPA contrast agent showing an enhancement of a perivascular granulomatous tissue.
On the third day of treatment the periorbital pain had stopped, paresis of vertical view and convergence had resolved, while an unchanged horizontal paresis of view remained.
The patient was treated with this regimen for 14 days following an episode of slowly decreasing the dosage. During the follow-up after 5 months the neurological examination showed no abnormality, no paralysis with a normal crainial nerve status. The patient complained about occasional diplopia of the right eye. MRI of the orbita in 2 mm slice thickness showed in the T1 SEfs sequence the same sized gadolinum uptaking tissue in the sinus cavernosus. The patient is in therapy with 25mg of cortison per day to be reduced to a permanent dose of 5 mg per day and 15 mg of MTX s.c. per week permanently.
Discussion
Physicians of patients with painful ophtalmoplegia, the combination of retroorbital or cranial pain and diplopia, have to consider a variety of differential diagnoses like trauma, diabetes mellitus, ophtalmoplegic migraine and THS. Other causes might be of vascular origin like vasculitis or intracarotid aneurysm and carotid-cavernous fistula, or the rare location of a hemangioma. Meningitis, sarcoidosis and tumours like lymphoma or epidermoid cysts, rare solitary fibrous tumours or even metastases of the cavernous sinus could be the cause for the symptoms [1–7].
The Tolosa-Hunt Syndrome (THS), a rather rare cause for PO [2], is characterized by recuring orbital pain acompanied by the paralysis of one or more of the cranial nerves III, IV and VI, that will respond well to corticosteroids or persist for weeks at a time if untreated [1,3].
As the etiology of the THS is still unknown, in the few cases where biopsy or surgery has been performed, granulomatous tissue consisting of proliferating fibroblasts and infiltration of lymphocytes and plasmacells in the walls of the cavernous sinus have been observed and it has been suggested that the increased pressure on penetrating nerves may be the cause for paralysis [1,8].
For many years the diagnosis of THS was one of excluding all other causes. With the introduction of high resolution MRI the identification of granulomatous tissue in the cavernous sinus or the superior orbital fissour has made it possible to narrow the range of differential diagnosis around THS. A clinical follow-up is still essential to rule out causes that have not been detectable or distinguishable inicially [8–10]. For example rare infections of the cavernous sinus that show similar MRI charactaristics and initial response to corticosteroids can wear on and worsen upon dose reduction with an increase in size of lesions [11].
The diagnostic criteria of the International Classification of Headache Disorders (ICHD)-III for THS [12] include:
Unilateral orbital pain that has preceded or coincided
Paresis of the III, IV and/or VI cranial nerve
Presentation of granulomatous tissue in the cavernous sinus, the superior orbital fissure or the orbita by MRI or biopsy
Exclusion of any other cause listed in the ICHD-III list.
In the case presented here, all other causes for the patients PO were excluded. The elevation of rheumtoid factor and ANA alone is non specific and since no other signs were found we had to rule out autoimmune disease. Our patient fulfilled all criteria for diagnosing THS with one exception, which is that the symptoms and signs even though starting on one side spread to the other side after a period of 3-4 days. There are other reported cases of bilateral manifestation that met all other criteria of THS and it has been documented that relapses can occur on the opposite side [1,10].
The last revision of the ICHD criteria does not include the disappearance of all signs within 72 hours of treatment [12], as it has been shown that granulomas could be seen for weeks to months even when pain has resolved within 72 hours after the beginning of treatment, and even ophthalmoplegia can last for several weeks [3,9]. While the pain of our patient resolved within 72 hours of treatment a partial view paresis remained for weeks and the granulomas were still evident even after 5 months. As no definite dose recommendation has been confirmed yet the persisting granulomas and occasional diplopia could be a prognostic sign for the necessity of treatment continuation.
Even though large granuloma lesions of up to 27 mm have been observed [9] usually the lesion size is between 1-2 mm [8]. During the diagnostic process of our patient characteristic lesions could only be found on MRI with 2 mm of slice thickness in an T1 SEfs sequence while the T1 SE sequence with 4 mm slice exam did not reveal the latter.
Conclusion
We present the rare case of a patient with bilateral PO that met all the diagnostic criteria of THS including granulomatous tissue in the cavernous sinus and pain that resolved under corticoid treatment within 72 hours. We therefore propose that THS as a differential diagnosis for bilateral PO should not be excluded. Furthermore our observations show that it is important to perform MRI of the orbital region in 2 mm slices with fat saturation in the T1 SE sequence to avoid overseeing granulomas that often do not excide a size of 1-2 mm. Further research is needed to answer the question if the persistence of granuloma after treatment is a prognostic factor for recrudescence and might be a reason to continue treatment even after pain and paralysis have resolved.
Consent
The Patient gave his written and informed consent for the publication of his case and the included images. A copy of this document has been made available for review by the editors of this journal.
[1]. Kline LB, The Tolosa-Hunt SyndromeSurv Ophthalmol 1982 27(2):79-95. [Google Scholar]
[2]. Anagnostou E, Kouzi I, Kararizou E, Painful ophthalmoplegia: The role of imaging and steroid response in the acute and subacute settingJ Neurol Sci 2013 331:145-49. [Google Scholar]
[3]. Colnaghi S, Versino M, Marchioni E, Pichiecchio A, Bstianello S, Cosi V, ICHD-II diagnostic criteria for Tolosa-Hunt syndrome in the idiopathic inflammatory syndromes of the orbit and/ or the carvernous sinusCephalgia 2008 28:577-84. [Google Scholar]
[4]. Mathew NT, Chandy J, Painful OphthalmoplegiaJ Neurol Sci 1970 11:243-56. [Google Scholar]
[5]. Tatagiba M, Laconetta G, Samii M, Epidermoid cyst of the cavernous sinus: clinical features, pathogenesis and treatmentBr J Neurosurg 2000 14(6):571-75. [Google Scholar]
[6]. Demirkaya M, Sevinir B, Ozdemir O, Nazlioglue HO, Okan M, Lymphoma of the cavernous sinus mimicking Tolosa-Hunt syndrome in a childPediatr Neurol 2010 42(5):351-54. [Google Scholar]
[7]. Korchi AM, Cuvinciuc V, Caetano J, Becker M, Lovblad KO, Vargas MI, Imaging of the cavernous sinus lesionsDiagn Interv Imaging 2014 95(9):849-59. [Google Scholar]
[8]. Hung CH, Chang KH, Wu YM, Chen YL, Lyu RK, Chang HS, A comparison of benign and inflammatory manifestations of Tolosa-Hunt syndromeCephalgia 2013 33(10):842-52. [Google Scholar]
[9]. Jain R, Sawhney S, Koul RL, Chand P, Tolosa-Hunt syndrome: MRI appearancesJ Med Imaging Radiat Oncol 2008 52:447-51. [Google Scholar]
[10]. Guedes BVS, da Rocha AJ, Zuppani HB, da Silva CJ, Sanvito WL, A case review of the MRI features in alternating Tolosa-Hunt syndromeCephalgia 2010 30(9):1133-36. [Google Scholar]
[11]. Mandrioli J, Frank G, Sola P, Leone ME, Guaraldi G, Guaraldi P, Tolosa-Hunt syndrome due to actinomycosis of the cavernous sinus: the infectious hypothesis revisitedHeadache 2004 44(8):806-11. [Google Scholar]
[12]. The International Headache SocietyThe International Classification of Headache Disorders, 3rd edition (beta version)Cephalgia 2013 33(9):629-808. [Google Scholar]