Unusual and Unique Variant Branches of Lateral Cord of Brachial Plexus and its Clinical Implications- A Cadaveric Study
Ashwini Aithal Padur1, Naveen Kumar2, Swamy Ravindra Shanthakumar3, Surekha Devadas Shetty4, Gayathri Sharath Prabhu5, Jyothsna Patil6
1 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
2 Assistant Professor, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
3 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
4 Senior Grade Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
5 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
6 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Manipal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naveen Kumar, Assistant Professor, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus) Manipal University, Manipal, Karnataka – 576104. India.
E-mail: naveentonse@gmail.com
Introduction
Adequate knowledge on variant morphology of brachial plexus and its branches are important in clinical applications pertaining to trauma and surgical procedures of the upper extremity.
Aim
Current study was aimed to report variations of the branches of the lateral cord of brachial plexus in the axilla and their possible clinical complications.
Materials and Methods
Total number of 82 upper limbs from 41 formalin embalmed cadavers was dissected. Careful observation was made to note the formation and branching pattern of lateral cord. Meticulous inspection for absence of branches, presence of additional or variant branches and presence of abnormal communications between its branches or with branches of other cords was carried out.
Results
In the present study, we noted varied branching pattern of lateral cord in 6 out of 82 limbs (7%). In one of the limb, the median nerve was formed by three roots; two from lateral cord and one from medial cord. Two limbs had absence of lateral pectoral nerve supplemented by medial pectoral nerves. One of which had an atypical ansa pectoralis. In 2 upper limbs, musculocutaneous nerve was absent and in both cases it was supplemented by median nerve. In one of the limb, coracobrachialis had dual nerve supply by musculocutaneous nerve and by an additional branch from the lateral cord.
Conclusion
Variations of brachial plexus and its branches could pose both intraoperative and postoperative complications which eventually affect the normal sensory and motor functions of the upper limb.
Ansa pectoralis, Median nerve, Musculocutaneous nerve, Pectoral nerves
Introduction
The brachial plexus supplies the upper limb and consists of roots, trunks, divisions and cords. Lateral cord of the brachial plexus is formed in the axilla by the union of anterior divisions of upper and middle trunks and it lies on the lateral side of the second part of the axillary artery. It gives 3 named branches; lateral pectoral nerve (C5, C6, C7) that pierces the clavipectoral fascia before supplying the pectoralis major muscle, musculocutaneous nerve (C5, C6, C7) which pierces the coracobrachialis muscle, supplies the muscles in the front of the arm and then continues as lateral cutaneous nerve of the forearm, and a third branch known as lateral root of median nerve (C6, C7) which joins with the medial root of median nerve arising from medial cord to form the trunk of the median nerve [1].
Anomalies in the formation or persistence of an abnormal communication between the branches are considered as common variations of lateral cord [2]. However, variation in its branching pattern is rare and it should be kept in mind while performing surgical approaches of axilla and arm region to avoid post surgical complications posed by its iatrogenic injury. Prior anatomical knowledge of any variations is thus very important to avoid such nerve injuries.
Aim
Therefore, this study was aimed to report variations of the branches arising from the lateral cord of brachial plexus in the axilla and their possible clinical implications.
Materials and Methods
Present study involved the examination of 82 upper limbs of 41 formalin embalmed human cadavers (40 males and one female) in the past four years, which were obtained from the Department of Anatomy. The axillary region of all the limbs were dissected cautiously and attached fascia was cleared from the cords of brachial plexus. All three cords of brachial plexus were exposed carefully. Meticulous observation was made to note the formation and branching pattern of lateral cord. The observations included absence of branches, presence of additional or variant branches and presence of abnormal communications between its branches or with branches of other cords if any, etc. The dissection was further continued towards the anterior compartment of the arm to note any alternative nerve supply to the structures to be supplied by the branches of lateral cord when they are absent and to investigate further course and distribution of the variant or additional branches when persisted. Variations of other cords and branches of brachial plexus were not included in the study. One photograph from each of the variations was taken for documentation.
Results
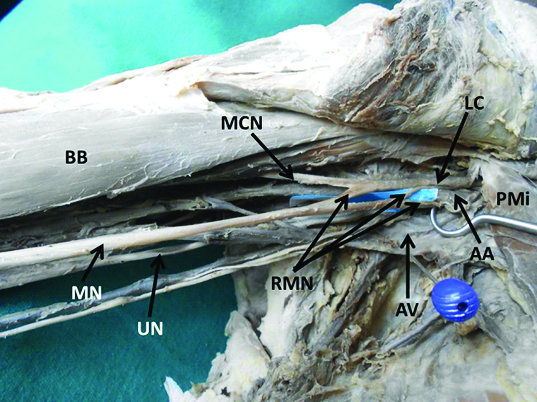
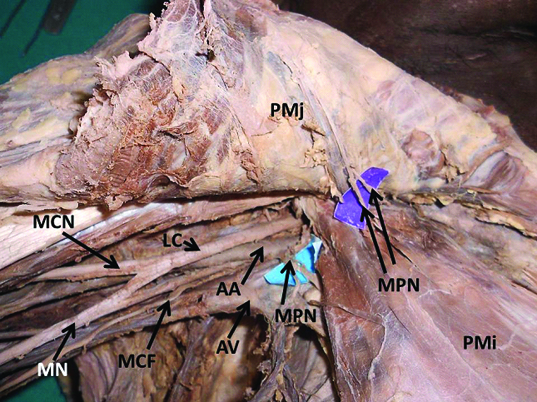
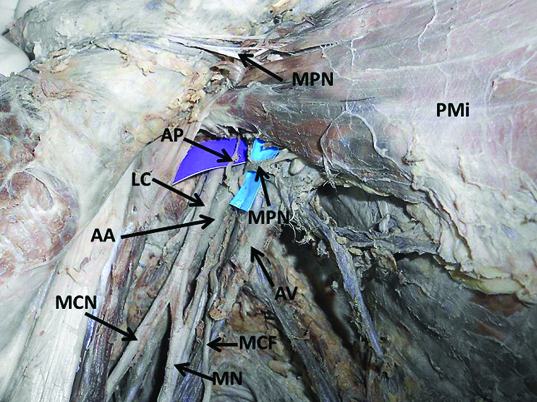
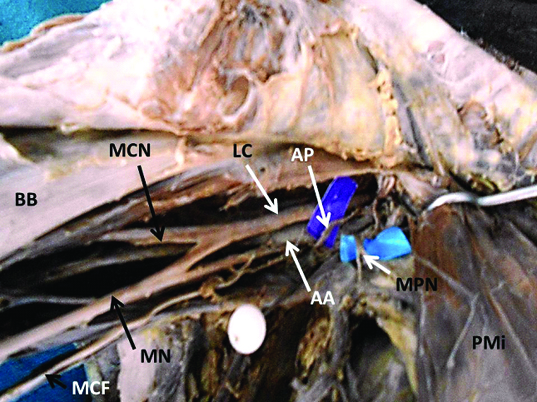
In the present study, we noted 4 different varied branching pattern of lateral cord of the brachial plexus in 6 out of 82 upper limbs (7%). In one limb of right side, the median nerve was formed by three roots than the usual two roots. Out of the three roots two roots (upper and lower) arose directly from the medial side of lateral cord and one root from the medial cord [Table/Fig-1]. The upper root arising from the lateral cord was thinner in caliber when compared to the lower root. These three roots encircled the axillary artery between them and formed the trunk of median nerve. In two upper limbs, lateral cord was deprived of lateral pectoral nerve. In both the cases, it was supplemented by multiple medial pectoral nerves which pierced the pectoralis minor muscle and then supplied the pectoralis major muscle from its deeper plane [Table/Fig-2]. In one of above 2 limbs, very rare variation wherein the ansa pectoralis which is usually seen connecting the medial and lateral pectoral nerve; arose as a twig directly from the medial side of lateral cord, looped around the third part of axillary artery and then joined with the medial pectoral nerve in deeper plane [Table/Fig-3,4]. In two limbs, one right and another left we found that musculocutaneous nerve was absent. In its absence, the muscles of anterior compartment of arm were supplied by branches from the median nerve. In both the cases, the lateral cutaneous nerve of the forearm was represented by a separate branch arising from median nerve [Table/Fig-5]. In another right upper limb we found a very rare variation wherein the coracobrachialis muscle was supplied by an additional branch coming from the lateral side of the lateral cord [Table/Fig-6]. Thus the coracobrachialis had dual nerve supply by musculocutaneous nerve and by an additional branch from the lateral cord. All the above seen variations were unilateral.
Showing unusual formation of the median nerve (MN) by three roots (RMN). Two roots from the lateral cord (LC) and one root from the medial cord. Other structures seen are: MCN- Musculocutaneous nerve, UN- Ulnar nerve, AA- Axillary artery, AV- Axillary vein, PMi- Pectoralis minor muscle, BB- Biceps Brachii.
Showing the absence of lateral pectoral nerve supplemented by multiple branches of the medial pectoral nerve (MPN) which supplied the pectoralis minor (PMi) and pectoralis major (PMj) muscle. MCN- Musculocutaneous nerve, LC- Lateral cord, AA- Axillary artery, AV- Axillary vein, MN- Median nerve, MCF- medial cutaneous nerve of forearm.
Showing the presence of atypical ansa pectoralis (AP) arising from the lateral cord (LC), which looped around the axillary artery (AA) and joined with the medial pectoral nerve (MPN). PMi- Pectoralis minor, AV-Axillary vein, MCN- Musculocutaneous nerve, MN- Median nerve, MCF- Medial cutaneous nerve of forearm.
Showing the closer view of ansa pectoralis (AP) arising directly from the lateral cord (LC) and looping around the axillary artery (AA). MPN- Medial pectoral nerve, MCN- Musculocutaneous nerve, MN- Median nerve, MCF- Medial cutaneous nerve of forearm, PMi- Pectoralis minor, BB- Biceps Brachii.
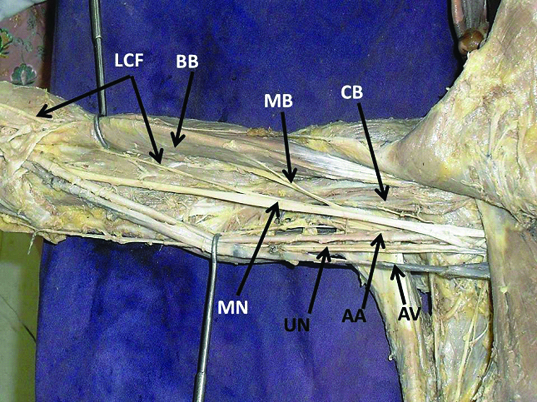
Showing the absence of musculocutaneous nerve, supplemented by Median nerve (MN) that also gave lateral cutaneous nerve of forearm (LCF). Biceps Brachii (BB) and coracobrachialis (CB) were supplied by muscular branches of median nerve (MB). AA- Axillary artery, AV- Axillary vein, UN- Ulnar nerve.
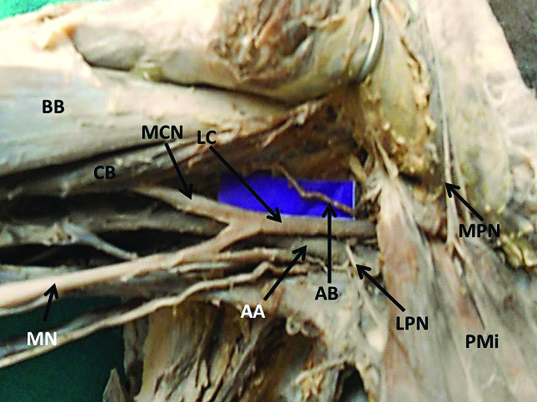
Showing the presence of an additional branch (AB) from the lateral cord (LC) and supplying the coracobrachialis muscle (CB) which was also supplied by musculocutaneous nerve (MCN). BB- Biceps brachii, MN- Median nerve, AA- Axillary artery, LPN- Lateral pectoral nerve, MPN – Medial pectoral nerve. PMi- Pectoralis minor.
Discussion
Variations of the brachial plexus have been reported by many researchers in the past. But, in the present study we are reporting unique findings related to the lateral cord. Our study was aimed to provide additional knowledge on lateral cord variations to clinicians and surgeons. This might help to avoid damage during surgical procedures involving the nerves of the upper limb as in plastic and reconstructive surgery.
Median nerve is associated with many variations. In the present study we found that median nerve was formed by three roots. Such type of variation has been observed in the past [3–5]. Sharmila et al., have reported a case wherein the median nerve was directly coming from the lateral cord without any contribution from the medial cord through medial root [6]. It has been opined by many researchers that the presence of such a variation in formation of median nerve may be of immense clinical interest to neurologists diagnosing nerve lesions and surgeons who deal with the topographical anatomy of the neural structures during radical neck dissection. Also, the additional branch of the lateral cord may compress upon the axillary artery which may cause vascular insufficiency [7].
The musculocutaneous nerve (MCN) is a major branch of lateral cord. There is ample number of reports about the absence of MCN [8–12]. It has been opined that absence of MCN may not lead to paralysis of the flexor compartment of the arm since the motor and sensitive fibres can arise from the other nerve. In the present study, in two limbs, the MCN was absent and the above muscles were supplied by branches from the median nerve. The structural abnormalities and variations of MCN have recently become significant and very important while performing neurotization of brachial plexus lesions, shoulder arthroscopy and shoulder reconstructive surgery [13].
Anatomical knowledge of the pectoral nerves is of clinical importance during mastectomy, neurotization or other surgical procedures in the axilla. In the present study we have noted the absence of lateral pectoral nerve (LPN) in two limbs. Absence of LPN is regarded as a rare variation and in our literature review we did not find any study reporting such type of variation. Rajalakshmi et al., have reported a case where three pectoral nerves were arising from the lateral cord of brachial plexus [14]. Gupta et al., have reported the presence of two lateral pectoral nerves which arose from upper and middle trunks of the brachial plexus [15].
We found that in the absence of LPN, pectorails major and minor muscles were supplied by medial pectoral nerves (MPN). Such a variation should be in the mind of a surgeon performing relevant surgical procedures involving these muscles and the pectoral region. The pectoralis major myocutaneous flap provides a simple, reliable, and versatile method of primary reconstruction of various head and neck defects [16–18]. Hence such variations are very important during breast surgeries using pectoral muscle flaps and pectoral nerve transfers [19]. Multiple MPN as seen in our case can be at high risk during mastectomy or breast reconstruction procedures [20].
A peculiar type of variation that we came across during our study was unusual persistence and communication of ansa pectoralis (AP). Although the term “ansa pectoralis” has been used previously [21] to describe the communication between the MPN and LPN, no reports exist in the literature, which specifically define or describe the AP.
Loukas et al., have studied the anatomy of ansa pectoralis (AP) and their various communications [22]. They have classified AP based on its origin. According to them, the most common type, AP-1 (42%) arose from the deep branch of the LPN; AP-2 (28%) arose directly from the LPN and AP-3 (25%) it arose from the lower rootlets of the LPN. Rarely, the AP arose from the upper rootlet of the LPN (AP-4; 5%). But the AP found in our study does not fall into any of the above classification as it originated directly from the lateral cord. This is a rare and unique variation and such cases hardly ever reported in the anatomical literature. Textbooks of anatomy report that the loop between the LPN and MPN crossed the first portion of the axillary artery. The peculiar AP loop that we have observed in our study crossed the 3rd part of axillary artery which is very unusual. Although very small, the AP is potentially an important nervous structure. Atypical persistence of AP looping around the axillary artery may lead to the compression of the vessel, and may lessen the blood supply to the upper extremity.
Musculocutaneous nerve is the sole nerve supply to coracobrachialis muscle. Very rarely, the coracobrachilais receives additional nerve supply. In the current study, we have noted an additional branch, arising directly from lateral cord which was supplying the coracobrachialis muscle. Thus, it was found that coracobrachialis muscle was supplied by two nerves. In our literature survey we found just one case reporting such type of variation. Ravikumar et al., have reported a case were two accessory nerve twigs arising from lateral cord of brachial plexus supplied the coracobrachialis muscle [23]. Surgeons operating on this region should be aware of such type of anomalous presence of additional branches.
Variations in the formation and branching pattern of brachial plexus can be explained through neuronal growth cones [24]. Alterations in signalling between mesenchymal cells and neuronal growth cones can lead to significant variations of which once formed would persist postnatally [25]. Multiple variations in the branching pattern of lateral cord of brachial plexus as we documented through this study, might be a result from bilateral alterations in mesenchymal cells and growth cones signalling.
Clinically, the presence of these variations makes the nerves vulnerable during routine neural repair and other surgical interventions in the pectoral and axillary region. Injury to any of such variant nerves in the proximal arm may lead to manifestations including sensory, motor, vasomotor changes. It is also important to be aware of these variations during brachial plexus blockade and in nerve entrapment syndromes [26]. We believe that reports regarding these variations will be illuminating for surgical procedures of the axilla and the shoulder. Knowledge of such anomalies is also important during treatment of fractures. Better understanding and correct interpretation of clinical neurophysiology can only be possible with prior knowledge of possible anatomical variations [27].
Conclusion
The axillary region is commonly approached for many surgical interventions by anaesthesiologists, orthopaedicians, radiologists and plastic surgeons. Lack of knowledge regarding such variations of the nerves of the lateral cord of brachial plexus may lead to intraoperative and postoperative complications.
[1]. Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, J., Ferguson MWJ, Gray’s Anatomy In: Nervous system 1995 38th EdnEdinburghChurchill Livingston:1266-74. [Google Scholar]
[2]. Abhaya A, Khanna J, Prakash R, Variation of the lateral cord of Brachial plexus piercing coracobrachialis muscleJ Anat Soc India 2003 52(2):168-70. [Google Scholar]
[3]. Sontakke BR, Tarnekar AM, Waghmare JE, Ingole IV, An unusual case of an asymmetrical formation and distribution of median nerveInternational Journal of Anatomical Variations 2011 4:57-60. [Google Scholar]
[4]. Pais D, Casal D, Santos A, O’neill JG, A variation in the origin of median nerve associated with unusual origin of the deep brachial arteryJournal of Morphological Sciences 2010 27:35-38. [Google Scholar]
[5]. Budhiraja V, Rastogi R, Asthana AK, Anatomical variations of median nerve formation: embryological and clinical correlationJ. Morphol. Sci 2011 28(4):283-86. [Google Scholar]
[6]. Sharmila Bhanu P, Devi Sankar K, Susan PJ, Formation of median nerve without the medial root of medial cord and associated variations of the brachial plexusInternational Journal of Anatomical Variations 2010 13:27-29. [Google Scholar]
[7]. Das S, Paul S, Anomalous Branching Pattern of Lateral Cord of Brachial PlexusInt J Morphol 2005 23(4):289-92. [Google Scholar]
[8]. Le Minor JM, A rare variation of the median and musculocutaneus nerve in manArch Anat histol Embryol 1990 73:33-42. [Google Scholar]
[9]. Gumsburun E, Adiguzel E, A variation of the brachial plexus characterised by the absence of the musculocutaneous nerve: a case reportSurg Radiol Anat 2000 22:63-65. [Google Scholar]
[10]. Sud M, Absence of the musculocutaneous nerve and innervation of corachobrachialis, biceps brachii and brachialis from the median nerveJ Anat Soc India 2000 49:176-77. [Google Scholar]
[11]. Song WC, Jung HS, Shin C, Lee BY, Koh KS, A variation of the musculocutaneous nerve absentYonsei Med J 2003 44:1110-13. [Google Scholar]
[12]. Nakatini T, Shigenori T, Mizukami S, Absence of the musculocutaneous nerve with innervations of corachobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexusJ Anat 1997 191:459-60. [Google Scholar]
[13]. Arvind KP, Ramesh Babu CS, Archana R, Anita R, Jyoti C, Rakesh KV, Absence Of Musculocutaneous Nerve: Embryogical BasisAsian Journal of Medical Sciences 2012 3:21-24. [Google Scholar]
[14]. Rajalakshmi R, Anu Ranade V, Latha Prabhu V, Mangala Pai M, Nayak SR, Accessory lateral pectoral nerves supplying the pectoralis majorRomanian Journal of Morphology and Embryology 2008 49(4):577-79. [Google Scholar]
[15]. Gupta M, Goyal N, Harjeet Anomalous communications in the branches of brachial plexusJ Anat Soc India 2005 54(1):22-25. [Google Scholar]
[16]. Baek SM, Lawson W, Biller HF, An analysis of 133 pectoralis major myocutaneous flapsPlast Reconstr Surg 1982 69(3):460-69. [Google Scholar]
[17]. Freedlander E, Lee K, Vandervord JG, Reconstruction of the axilla with a pectoralis major myocutaneous island flapBr J Plast Surg 1982 35(2):144-46. [Google Scholar]
[18]. Mehrhof AI, Rosenstock A, Neifeld JP, Merritt WH, Theogaraj SD, Cohen IK, The pectoralis major myocutaneous flap in head and neck reconstruction. Analysis of complicationsAm J Surg 1983 146(4):478-82. [Google Scholar]
[19]. Samardzic M, Rasulic LG, Grujicic DM, Bacetic DT, Milicic BR, Nerve transfers using collateral branches of the brachial plexus as donors in patients with upper palsy: thirty years’ experienceActa Neurochir (Wien) 2011 153:2009-19. [Google Scholar]
[20]. Litts CS, Hennigan SP, Williams GR, Medial and lateral pectoral nerve injury resulting in recurrent scapular winging after pectoralis major transfer: A case reportJ Shoulder Elbow Surg 2000 9:347-49. [Google Scholar]
[21]. Bergman RA, Thompson SA, Afifi AK, Saadah FA, Compendium of human anatomic variation 1988 BaltimoreUrban and Schwarzenberg:140 [Google Scholar]
[22]. Loukas M, Robert G, Louis Jr, John F, Gene C, The Surgical Anatomy of the Ansa PectoralisClinical Anatomy 2006 19:685-93. [Google Scholar]
[23]. Ravikumar V, Siri AM, Sadashivana Gowd H, Acharya A, Variation in the nerve Supply to Coracobrachialis Muscle - A Case StudyInternational Journal of Contemporary Medicine 2013 1(1):48-50. [Google Scholar]
[24]. Dent EW, Tang F, Kalil K, Axon guidance by growth cones and branches: Common cytoskeletal and signaling mechanismsNeuroscientist 2003 9(5):343-53. [Google Scholar]
[25]. Brown MC, Hopkins WG, Keyness RJ, Axon guidance and target recognitionIn: Essentials of Neuro Development 1991 Cambridge University Press:46-66. [Google Scholar]
[26]. Manicka Vasuki AK, Jamuna M, Kalyana Sundaram K, Nirmala Devi M, Bilateral Variations of Infraclavicular Part Of Brachial PlexusInnovative Journal of Medical and Health Science 2015 5(2):70-72. [Google Scholar]
[27]. Saeed M, Rufai A, Median and musculocutaneous nerves: variant formation and distributionClin Anat 2003 16(5):453-57. [Google Scholar]