Infra-cardiac Total Anomalous Venous Connection to Portal Vein – Unusual Dynamic Hepatic Flow Phenomenon Demonstrated with MRI
Venkatraman S. Bhat1
1 Director of Imaging Services, Department of Radiology, 1 Narayana Health, Bangalore, Bommasandra, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Venkatraman S. Bhat, 309, Greenwoods Apt, Royal Gardenia, Bommasandra, Bangalore-560099, Karnataka, India.
E-mail: bvenkatraman@gmail.com
Functional information regarding fluid movement within the body can be derived by magnetic resonance methods. Some of the observations were overlooked in early days of magnetic resonance imaging (MRI) application. This presentation illustrates an unique, intra-hepatic haemodynamic phenomenon, demonstrated by magnetic resonance imaging, in a case of infra-cardiac Total Anomalous Pulmonary Venous Connection (TAPVC) Demonstration of such phenomena is unreported even after widespread use of cardiac MRI, although patho-physiology of such a phenomenon is expected in TAPVC. Brief explanation and possible basis of such observation in the context of current knowledge is discussed.
CHD, MRI, Portal flow, TAPVC
Case Report
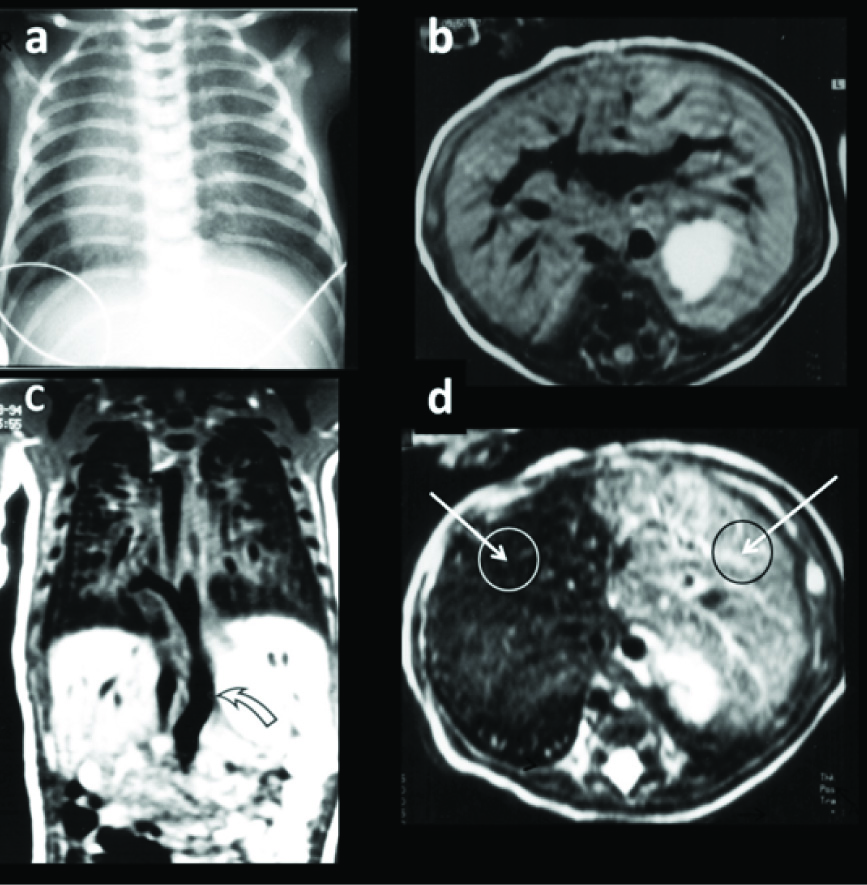
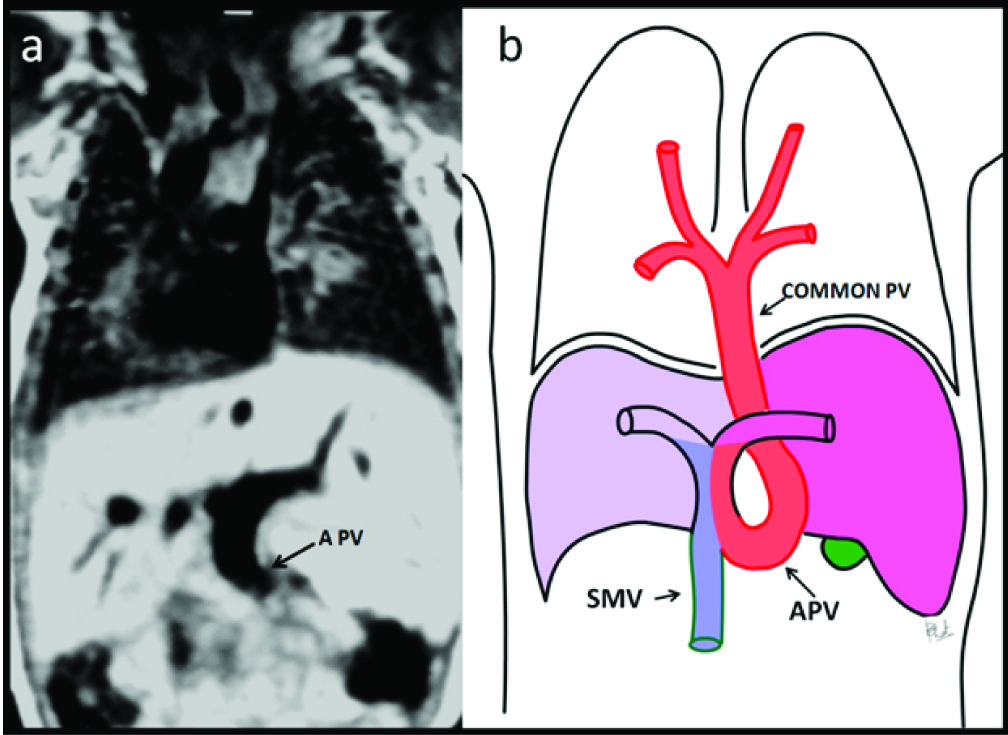
A Term newborn, one-day-old, was admitted to ICU for respiratory distress and grunting. The Infant was dusky, tachypneic, had laboured breathing. Baby was cyanotic. Heart rate was irregular, 95/min. APGAR scores at one and five minute was 3 and 4 respectively. Infant needed artificial respiratory support. Clinical examination revealed reduced chest wall movement on left side. Auscultation of heart revealed muffled heart sounds. Abdominal examination was unremarkable. Blood examination revealed arterial desaturation. Chest radiography demonstrated dextrocardia & a small left pneumothorax [Table/Fig-1a]. Echo-cardiography confirmed dextrocardia showed in addition, a large ASD with right to left shunt. Pulmonary-veins were not visualized. Abdominal sonography showed left-sided stomach, symmetrical liver, and absence of spleen. An anomalous vein was noted in midline behind left lobe of liver, joining the portal-vein (PV). On MR examination all pulmonary-veins were seen constituting a common channel [Table/Fig-1c], traversing the diaphragm taking a curved path with convexity to the right, to reach PV [Table/Fig-2a&b]. Axial proton density-TR-2000, TE-15 and T2 images-TR-2000, TE-90msc [Table/Fig-1b&d] showed temporal evolution of relatively mild hyperintensity of left-lobe in PD sequence to gross T2-hyperintensity in T2W images, a phenomena not documented in TAPVC. Dextrocardia, situs inversus, symmetrical liver with larger left lobe and absence of spleen were confirmed on MRI examination. The Infant continued to have persistent desaturation not responding to positive pressure ventilation with high FiO2 level, subsequently died on ninth day.
Discussion
Presently available state of the art MRI methods provide wide range of functional information related to vascular flow or cerebro-spinal fluid flow by phase-contrast technique [1,2]. In early application of MRI, more emphasis was made on structural information, with little reference to physiological information. Techniques are further modified to include velocity and spatial orientation of flow in multiple planes in the 4D phase-contrast technique [1]. Earlier to current imaging options, some effects of physiological processes were noted in conventional MR images, but mainly contributed to image degradation or flow artifacts. T2W images (PD and long T2) have some potential to show temporal changes in tissue signals over a period of time.
Our case is an illustrative example of how valuable physiological information can be demonstrated in a patient with anomalous pulmonary connection by ‘early’ MR imaging technique. Infant with suspected cardiac disease was investigated in 1994 after initial evaluation ultrasound demonstrating an anomalous vein joining the portal vein; MRI examination of chest and abdomen was performed with 1.5T Magnetom (Siemens, Erlangen Germany). Conventional spin-echo T1 weighted; proton-density (TR-2000, TE- 15) and T2 weighted (TR-2000, TE-90) (imaging were performed in axial and sagittal planes. T2W axial images initially showing near comparable signals in both lobes of liver, subsequently demonstrating sharp decrease in T2 signals in the right lobe over a period of 75msc was puzzling. As it was in the early days of MRI technique, with minimal data regarding cardiac imaging, no proper explanation could be provided to the unique observation. Some initial work by Ogawa et al., suggested a phenomena of blood oxygen dependent effect (BOLD) and effect of vascular flow in MR signal alteration [3]. Role of de-oxyhaemoglobin in blood or rapid vascular flow leading to magnetic in-homogeneity, are well described by Buxton RB et al., [4]. Most of these explanations are demonstrated on gradient sequences, not on spin-echo, due to lack of sensitivity of the later. Also application and interpretation of the technique was limited to neurological applications. In our patient both mechanisms, gross difference in oxygen level and lamellar portal flow, appear to play an important role. In the context of liver, portal flow dynamics play very important role in distribution of visceral blood flow. It has been recently possible to gather this information by flow-sensitive 4D MR imaging with broad volumetric coverage [5], 4D velocity mapping studies are now performed in clinical situation for cardiovascular system [1,6]. Uribe S et al., have demonstrated the possibility to characterize large scale flow through the cardio-vascular structures from a single free-breathing scan with comparable accuracy to conventional 2D flow measurements [1,6]. 3D streamline calculation allows representation of dynamic velocity directions within heart and great vessels.
Precision localization of emitter planes in both pulmonary veins, left ventricle, ascending aorta, inferior vena, superior vena cava and measuring flow magnitude and direction makes it possible document color coded map of flow traces and flow-path according to anatomic origin [1]. These applications are likely to be of value in documenting abnormal flows in patients with more complex congenital heart disease [6,7]. Techniques are also likely to be useful in follow-up of patients after surgical correction. Extended application of this technique to include liver has potential to demonstrate laminar flow in portal vascular system. In our patient separate streaming of blood from superior mesenteric vein and anomalous pulmonary vein was due to curved path of terminal common pulmonary vein, preferentially directing the oxygen rich blood flow to left side and desaturated venous blood to right [Table/Fig-2b]. Thus evident signal drop was shown in right lobe due to excess de-oxyhaemoglobin. Sharp demarcation between the lobes was evidently due to vascular territory. This illustration is an eye opener, serves to remind us about relentlessly exploring unexplained observations and following-up in the light of developing technology. Newer 4D velocity mapping imaging techniques and BOLD dependant sequences appear to hold future in demonstrating intravascular laminar flow pattern and correlation of effect of oxygen saturations level within the intravascular volume.
(a) Chest radiograph demonstrates dextrocardia; (b) Proton density axial images showing mild hyperintensity of signals of Left lobe of liver; (c) Coronal T1WI demonstrating common pulmonary vein from origin to infra-diaphragmatic course (curved arrow); (d)T2 WI axial images shows gross discrepancy in signals of right and left lobes of liver.
(a) Coronal T1WI image shows terminal path of common vein joining portal vein (black arrow); (b). Diagrammatic illustration of path of common vein, confluence at Portal vein and resultant haemodynamic effect on liver (SMV-superior mesenteric vein, APV- anomalous pulmonary vein).
Conclusion
Unusual hepatic MR imaging appearance is reported in a case of infra cardiac total anomalous pulmonary venous connection. Findings consisted of gross discrepancy of T2 signals in hepatic lobes with long acquisition time. Phenomenon appears to be due to combination of factors which include gross discrepancy in O2 levels in hepatic lobes, streaming of portal blood and intrinsic sensitivity of sequence to above changes in the context of unique patho-physiology.
[1]. Markl M, Kilner PJ, Ebbers T, Comprehensive 4D velocity mapping of the heart and great vessels by cardiovascular magnetic resonanceJ Cardiovasc Magn Reson 2011 13:7doi: 10.1186/1532-429X-13-17 [Google Scholar]
[2]. Naidich TP, Altman NR, Gonzalez-Arias SM, Phase contrast cine magnetic resonance imaging: normal cerebrospinal fluid oscillation and applications to hydrocephalusNeurosurg Clin N Am 1993 4(4):677-705. [Google Scholar]
[3]. Ogawa S, Lee TM, Kay AR, Tank DW, Brain magnetic resonance imaging with contrast dependent on blood oxygenationProc Natl Acad Sci USA 1990 87:9868-72. [Google Scholar]
[4]. Buxton RB, The physics of functional magnetic resonance imaging (fMRI)Rep Prog Phys 2013 76(9):096601 [Google Scholar]
[5]. Stankovic Z, Csatari Z, Deibert P, Euringer W, Blanke P, Kreisel W, Normal and altered three-dimensional portal venous haemodynamics in patients with liver cirrhosisRadiology 2012 262(3):862-73. [Google Scholar]
[6]. Uribe S, Beerbaum P, Sorensen TS, Rasmusson A, Razavi R, Schaeffter T, Four dimensional (4D) flow of the whole heart and great vessels using real-time respiratory selfgatingMagn Reson Med 2009 62(4):984-92. [Google Scholar]
[7]. Frydrychowicz A, Landgraf B, Wieben O, Francois CJ, Images in Cardiovascular Medicine: Scimitar syndrome: added value by isotropic flow-sensitive four-dimensional magnetic resonance imaging with PCVIPR (phase-contrast vastly under sampled isotropic projection reconstruction)Circulation 2010 121(23):434-36.doi: 10.1161/CIRCULATIONAHA.109.931857 [Google Scholar]