Multifocal Tumefactive Demyelination Mimicking Intracranial Neoplasm
Tom George1, Soumya Cicilet2, Ravi Hoisala3, Prithilata Rout4
1 Post Graduate Resident, Department of Radio Diagnosis, St. Johns Medical College, Bangalore, India.
2 Assistant Professor, Department of Radio Diagnosis, St. Johns Medical College, Bangalore, India.
3 Professor and Head of the Department, Department of Radio Diagnosis, St. Johns Medical College, Bangalore, India.
4 Professor and Head of the Department, Department of Pathology, St. Johns Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tom George, Post Graduate Resident, Department of Radio Diagnosis, St. Johns Medical College, Sarjapur Road, Bangalore - 560034, India.
E-mail: mail2dr.tomgeorge@gmail.com
Demyelinating disease presenting with clinical and radiologic features similar to a brain tumour is referred to as tumefactive demyelination. These lesions pose considerable diagnostic uncertainty. This is partly due to the atypical neurologic symptoms that the patient can present with as a consequence of the size, location, and potential for associated mass effect and oedema. The MRI appearance of these lesions can aid in preoperative diagnosis and assist with the final pathologic interpretation. We report a case of tumefactive demyelination where MRI played a vital role in arriving at a diagnosis. The diagnosis was confirmed histopathologically.
Differential diagnosis, MRI, Ring enhancing
Case Report
A 34-year-old male patient had complaints of left sided headache and periorbital pain followed by left lower limb weakness and urinary retention. The next day, the patient developed right upper limb weakness and loss of sensation below the chest. The patient was taken to a local hospital. His condition worsened over the course of few days and he developed inability to speak. So he was referred to our hospital. After detailed neurological examination, he was referred for MRI Brain & Spine.
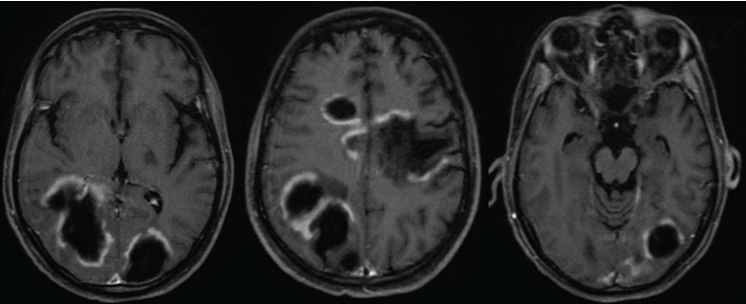
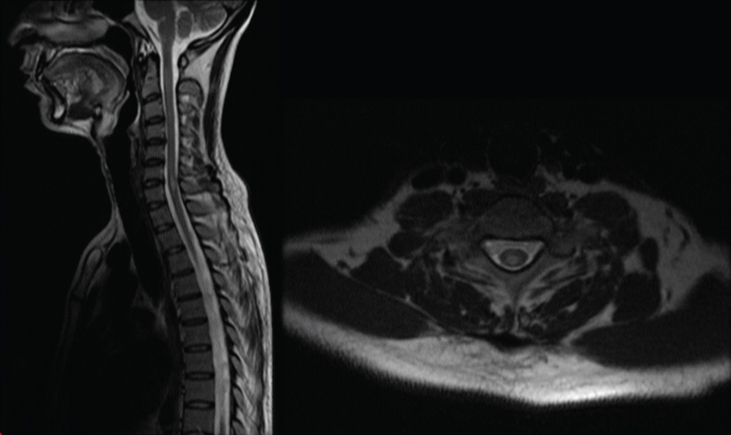
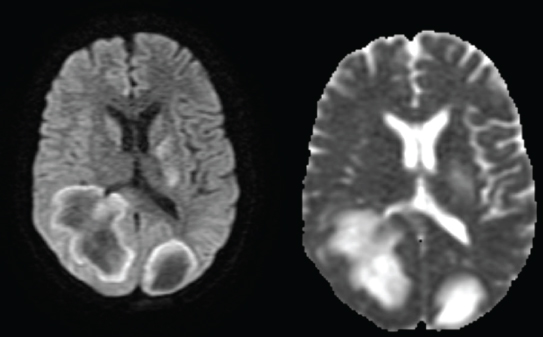
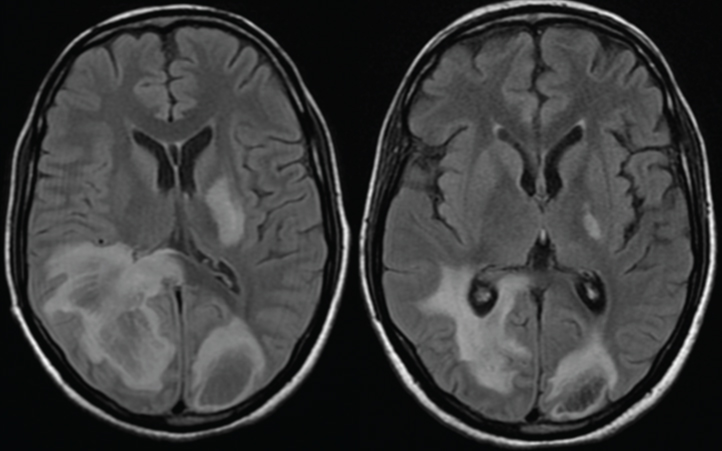
MRI showed evidence of large, multiple incomplete ring enhancing lesions in periventricular, deep white matter and subcortical white matter [Table/Fig-1]. Few signal intensity changes were also noted in the multiple spinal cord levels [Table/Fig-2]. DWI showed low signal changes with high signal on ADC [Table/Fig-3].
MRI- Multiple large incomplete ring enhancing lesions in the white matter with the discontinuous part of the ring towards the grey matter.
T2 hyperintense cord signal change at C6-C7 level.
DWI showing predominantly low signal changes with high signal on ADC.
Based on these imaging features, a diagnosis of tumefactive demyelination was made. Lymphoma was given as a differential diagnosis. Based on the diagnosis, the patient was treated with a 5 day course of i.v. methyl prednisolone and then shifted to oral steroids (T.Prednisolone 10 mg 1-1/2-0). Following this, the patient had recovered from his right upper limb weakness.
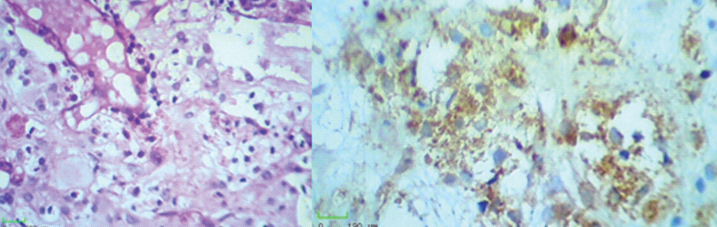
Brain biopsy done confirmed the MRI diagnosis of tumefactive demyelination [Table/Fig-4]. Anti-NMO antibodies, ANA levels and acetyl choline levels were all negative for the patient. HIV-ELIZA test was negative. Repeat MRI after 6 weeks of treatment showed reduction of white matter lesions [Table/Fig-5]. Tab Azathioprine was started at 50 mg 1-0-0 for two weeks and dose was increased to 50mg 1-0-1. The patient was discharged on T.Azathioprine and oral steroids. The patient was advised to slowly taper Prednisolone after 6 weeks by 5 mg every week and to maintain 10 mg 1-0-0.
a) H & E showing sheets of foamy macrophages, 400x magnification; b) IHC (CD 68) stains cytoplasm of macrophages.
T2 FLAIR images a) Before and b) After steroid therapy showing reduction of white matter changes post treatment.
Discussion
Tumefactive demyelinating lesions (TDLs) are defined as single or multiple large (usually >/= 2 cm) lesions mimicking brain tumours with characteristic post contrast appearance on MRI [1–3]. These lesions more commonly occur in women at an average age of 37 years [4]. The typical appearance of demyelinating lesions on MRI is preferential involvement of the major white matter tracts in a periventricular distribution. However, if the lesion is seen as solitary large lesion, a biopsy is usually needed for confirmation [5].
In patients with multiple sclerosis (MS), one of the variant form is tumefactive demyelination which presents with atypical clinical and radiological manifestations [6]. The differential diagnosis usually considered are brain tumours (such as multi focal glioma, metastasis, CNS lymphoma), brain abscess, tuberculoma and other inflammatory entities such as sarcoidosis and sjogren’s syndrome [6,7]. Patient can present with different clinical features such as focal neurologic deficit, seizures or aphasia unlike that would be usually seen in MS [8].
Tumefactive demyelinating lesions commonly involve the supratentorial compartment and are centered within the white matter [1]. Commonly the enhancement pattern will be in the form of an open ring, with the continuous portion of the ring towards the ventricular portion and discontinuous portion towards the gray matter side of the lesion [9]. Other enhancement patterns described are diffuse, homogeneous, punctate, or concentric enhancement [10]. On DWI, the ADC values may be increased thus proving to be a useful tool in differentiating ring-enhancing tumefactive demyelinating lesions from cerebral abscesses, the latter being associated with restricted diffusion centrally within the lesion. Most tumefactive demyelinating lesions will show an excellent response to corticosteroid and immune suppressive therapy. On follow up imaging, a substantial decrease in size or disappearance of the lesions is seen [4].
Conclusion
Tumefactive demyelinating lesions are usually a diagnostic dilemma to neurosurgeons, radiologists, and pathologists. The MRI appearance of these lesions can aid in preoperative diagnosis and assist with the final pathologic interpretation.
[1]. Dagher AP, Smirniotopoulos J, Tumefactive demyelinating lesionsNeuroradiology 1996 38:560-65. [Google Scholar]
[2]. Lucchinetti CF, Gavrilova RH, Metz I, Parisi JE, Scheithauer BW, Weigand S, Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosisBrain 2008 131:1759-75. [Google Scholar]
[3]. Butteriss DJ, Ismail A, Ellison DW, Birchall D, Use of serial proton magnetic resonance spectroscopy to differentiate low grade glioma from tumefactive plaque in a patient with multiple sclerosisBr J Radiol 2003 76:662-725. [Google Scholar]
[4]. Kepes JJ, Large focal tumour-like demyelinating lesions of the brain: intermediate entity between multiple sclerosis and acute disseminated encephalomyelitis? A study of 31 patientsAnn Neurol 1993 33:18-27. [Google Scholar]
[5]. Given CA, Stevens BS, Lee C, The MRI Appearance of Tumefactive Demyelinating LesionsAJR 2004 182:195-99. [Google Scholar]
[6]. Hamed SA, Variant of multiple sclerosis with dementia and tumefactive demyelinating brain lesionsWorld J Clin Cases 2015 3(6):525-32. [Google Scholar]
[7]. Sanahuja J, Ordonez-Palau S, Beque R, Brieva L, Boquet D, Primary Sjogren syndrome with tumefactive central nervous system involvementAm J Neuroradiol 2008 29(10):1878-79. [Google Scholar]
[8]. Paley RJ, Persing JA, Doctor A, Multiple sclerosis and brain tumour: a diagnostic challengeJ Emerg Med 1989 7:241-44. [Google Scholar]
[9]. Masdeu JC, Moreira J, Trasi S, Visintainer P, Cavaliere R, Grundman M, The open ring: a new imaging signs in demyelinating diseaseJ Neuroimaging 1996 6:104-07. [Google Scholar]
[10]. Lucchinetti CF, Gavrilova RH, Metz I, Parisi JE, Scheithauer BW, Weigand S, Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosisBrain 2008 131:1759-75. [Google Scholar]