Trichoepitheliomas (TE) are benign tumours but occasionally can undergo transformation to malignant neoplasms more commonly as Basal Cell Carcinoma (BCC). The correct diagnosis between these tumours is very important because basal cell carcinoma is locally aggressive neoplasm and requires total surgical excision with wide healthy margins while trichoepithelioma needs simple excision. We describe three patients who developed basal cell carcinoma with facial trichoepitheliomas. The only clinical feature that distinguished the carcinomas from the trichoepitheliomas was their larger size, in all three patients, one patient with recurrent, hyper pigmented swelling with surface ulceration and in another patient there are multiple trichoepitheliomas, and other family members are also affected. The history, clinical features and histopathological findings were suggestive of the evolution of basal cell carcinoma directly from trichoepithelioma in our first two cases, but in the third case TE and BCC were separate lesions on face and we are uncertain about whether the BCC developed independently or by transformation from a trichoepithelioma. Based on our clinicopathological observations in the three patients and reports in the recent literature, BCC with follicular differentiation and trichoepithelioma are considered to be highly related.
Case Report
Case 1
A 75-year-old female, with a swelling over the right side of the forehead for the last 9 years. It has been growing rapidly for the last three months, extended to right eye brow and upper eyelid producing partial ptosis of right upper eye lid. On examination there was a single skin coloured erythematous plaque studded with papules & nodules of varying size with central atrophy, soft to firm in consistency with ulceration and edge showed beading and pigmentation. Swelling was not fixed to the underlying bone except at the eye brow region. Loss of hair over the lateral aspect of eye brow on right side was noted [Table/Fig-1a]. Rest of the skin was normal. There was no enlargement of regional lymph nodes. No other similar swellings elsewhere over the body.
(a) Case 1-Preoperative photograph. (b) Case 1-Photomicrograph of solitary giant trichoepithelioma (H&EX40): A well circumscribed dermal tumour composed of islands of basaloid cells. (c) Case 1-Photomicrograph of Mixed nodular and infiltrative BCC (H&E 100X): There is an admixture of rounded and irregularly contoured tumour cell nests with peripheral palisading embedded in a fibrous stroma with slit-like retraction. (d) Case 1-Postoperative photograph after 3 weeks.
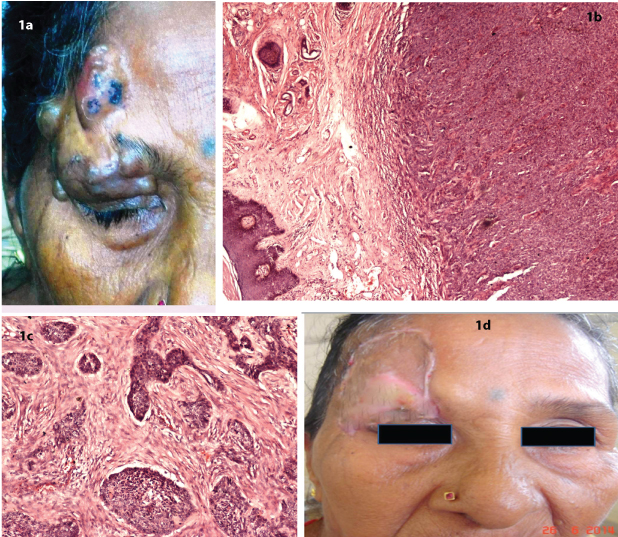
CT scan findings showed a well-defined round mixed density lesion measuring 3x2.6 cm with fluid level noted in supero-lateral aspect of right orbit causing minimal compression, displacement of right eye ball inferomedially and mild erosion of adjacent right frontal bone.
Complete excision and repair of the defect was done by temporalis fascia and split skin grafting. Operative findings showed tumour involving the right forehead, extending into the orbit displacing the eye ball inferomedially. Histopathology revealed Solitary giant trichoepithelioma transformed into a Basal cell carcinoma [Table/Fig-1b,c]. Follow up after 3 weeks showed good healing and the patient is quite comfortable [Table/Fig-1d]. She is doing well without any recurrence after 1 year as per telephonic follow up.
Case 2
A 56-year-old female was referred to plastic surgery consultation, she was having multiple, asymptomatic skin lesions over the face since she was 10-year-old. The lesions were more predominant over the forehead, nose and nasolabial region of the face. She also had a rapidly progressing ulcerative nodular lesion over dorsum of the nose towards left side since 2months which was itchy and painful [Table/Fig-2a]. She had 7 children, and amongst them, simlar type of lesions are present in 3 sons and 2 daughters. Second son had two male children; the elder one also got affected. The involved family members are depicted in the pedigree chart along with the photographs [Table/Fig-2d].
(a) Case 2-Preoperative photograph. (b) Case 2- Photomicrograph of Trichoblastic carcinoma (H&EX40):Showing tumour component composed of atypical basaloid cells arranged in the form of cords and nodules with increased mitotic activity. (c) Case 2- Photomicrograph of TE(H&EX100): Showing dermal islands of proliferating basaloid cells with characteristic papillary mesenchymal bodies and tiny horn cysts. (d) Case 2- Pedigree of the patient’s family and photographs. Males and females are indicated by squares and circles, respectively. The patient (grandmother), 3 sons, 2 daughters and one grandson were involved. Daughters were not depicted in photographs. (e) Case 2-Postoperative photograph after 1 year.
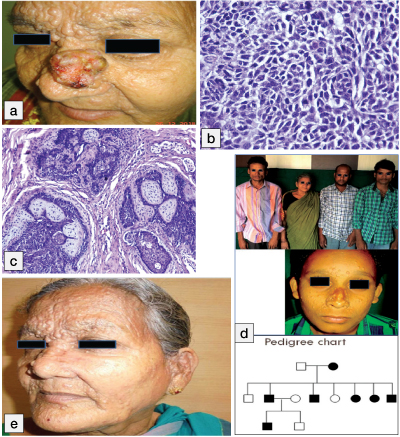
On examination multiple, round, smooth, firm, skin coloured circumscribed papules and nodules of varying sizes predominantly present over central part of face. A single lesion of size 5x5cm, an outgrowth present over nose extends from root of nose to left ala nasi. Surface of lesion showed lobulation, ulceration and haemorrhage and the tumour was not fixed to the underlying structures and there was no enlargement of regional lymph nodes.
Wide excision was done with 6cm margin and the dfect was reconstructed by fashioning an advancement flap from the left cheek. A small nodule was excised from left ala nasi. Histopathology revealed trichoblastic carcinoma from the ulcerated lesion over the nose [Table/Fig-2b] and trichoepithelioma for adjacent tiny nodule [Table/Fig-2c]. She is followed every month, wound healed completely and doing well when she came for follow up after 1 year [Table/Fig-2e].
Case 3
A 68-year-old male, with a recurrent blackish coloured swelling, near the medial canthus of right eye, extending on to the nose since 3 years, he gave history of excision of a tumour at that site 3 years back, but recurred within 3 months. He also had a painless swelling on the left side of the upper lip since childhood, which was gradually increasing in size [Table/Fig-3a].
(a) Case 3-Preoperative photograph of BCC right medial canthus and TE left upper lip (indicated by arrow). (b) Case 3-Photomicrograph of BCC–adenoid type (H & E100X): Tumour is arising from the basal layer of the epidermis and arranged in the form of strands and lace like pattern with peripheral palisading. (c) Case 3-Photomicrograph of TEon left upper lip (H&EX100): Showing basaloid tumour islands, horn cysts filled with keratin and papillary mesenchymal bodies. A focus of calcification is evident. (d) Case 3-Postoperative photograph after 1 year 3 months.
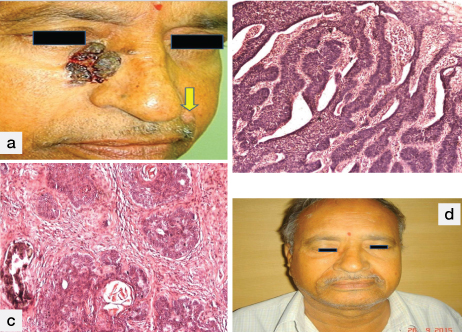
On examination there was a single, irregular, hyper pigmented, mobilecutaneous swelling, near medial canthus of right eye, extending on to lateral wall of the nose measuring 4x3cm. Surface of lesion was crusted along with ulceration and haemorrhage. The nodule on the left upper lip was measuring 1.5x1.5cm and was situated in the skin.
Tridimensional wide excision was done for swelling near the medial canthus of right eye and the defect was repaired by fashioning the cheek advancement flap. The swelling on the left side of the lip was completely excised and primary repair was done. Histopathology revealed basal cell carcinoma-adenoid type for the tumour near the right medial canthus [Table/Fig-3b] and trichoepithelioma for the nodule over the left upper lip [Table/Fig-3c]. Follow up done for 1year 3 months showed complete healing without any recurrence [Table/Fig-3d]. The salient features of all the three cases are tabulated in [Table/Fig-4].
Three cases of trichoepithelioma in association with basal cell carcinoma
| Case | Age | Gender | Location | Surgery performed | Histopathology |
|---|
| 1 | 75 | Female | Right forehead + right eye brow | Complete excision and repair of the defect by temporalis fascia and split skin grafting. | Solitary giant trichoepithelioma with Basal cell carcinoma |
| 2 | 56 | Female | Left side of nose + face | Wide excision and reconstruction with kite flap | Trichoblastic carcinoma and Multiple familial trichoepithelioma |
| 3 | 68 | Male | Right medial canthus + upper lip | Wide excision and reconstruction by cheek advancement flap | Basal cell carcinoma-adenoid type and Trichoepithelioma |
Discussion
Trichoepithelioma (TE) was first described by Brooke HG as Epithelioma Adenoides Cysticum and demonstrated the histogenesis of this tumour from epidermis and epithelium of hair sacs [1]. Trichoepitheliomas (TE) originates from basal cells in the hair follicles and occurs either as solitary non-familial or multiple familial forms [2]. The Multiple Familial Trichoepithelioma (MFT) is an uncommon autosomal dominant disorder, as a result of the loss of heterozygosity in the 9p21 region [3]. It is characterized by multiple facial papules and nodules located around the nasolabial area, nose, forehead, upper lip and occasionally the scalp, neck, upper trunk and perianal region [4]. The distinction of TE from Basal Cell Carcinoma (BCC) is sometimes difficult, clinically and histologically. The lesions are skin coloured, firm papules or nodules of 2-8mm in diameter, slow growing and commonly seen in childhood and adulthood. Females are most commonly affected because of the lessened penetrance [4]. In our cases the only clinical feature that distinguished BCC from the TE was their larger size, in all three patients, one patient with recurrent, hyper pigmented swelling with surface ulceration and in other patient there are multiple familial trichoepitheliomas, and one of which is large and rapidly growing.
Histologically, TE is characterized by a well circumscribed dermal tumour composed of islands, nests and cords of uniform basaloid cells in a cellular fibrous stroma (papillary mesenchymal bodies). The tumour may be associated with epithelial structures resemble hair papillae or abortive hair follicle, small keratocysts (infundibular differentiation) lined by stratified squamous epithelium and foci of calcification [5].
Both tumours are composed of nests of basaloid cells with follicular differentiation. Differences between TE and BCC were TE consists of characteristic papillary mesenchymal bodies and horn cysts whereas BCC consists of basaloid tumour islands with peripheral palisading, stromal retraction artefacts, increased mitotic activity and necrosis [6]. In some cases, histopathologic differentiation between basal cell carcinoma with follicular differentiation and trichoepithelioma may be impossible on the basis of haematoxylin and eosin staining, and such distinction is important for treatment and prognosis [5].
Immunohistochemical staining technique may help to distinguish between basal cell carcinoma and trichoepitheliomas using antibodies against a number of immunomarkers such as bcl-2, CD34, CD10, androgen receptor, transforming growth factor-β, Ki-67 proliferative index and the follicular stem cell marker pleckstrin homology-like domain, family A, member 1(PHLDA1) [6–9].
Trichoepitheliomas can undergo transformation to basal cell carcinoma and usuallyoccurs in the setting of multiple trichoepitheliomas, but there are reported cases of sporadic TE in association with BCC [6,7]. In our first case, it was a giant solitary trichoepithelioma which has transformed into BCC, which is similar to a case reported by sahin MT et al., [10], whereas in the second case multiple familial trichoepitheliomas, one of it transformed into BCC, and in the third case BCC and TE were separate lesions on face. Treatment for multiple TEs include excision, electrodessication, dermabrasion, cryotherapy, radiotherapy, Argon, Carbon dioxide, erbium-YAG lasers. Surgical excision, with or without flap used by most of the authors, is the standard treatment for most of TEs. For lesions over face, radio-surgical ablation helps in accurate removal of the tumour with tumour negative margins and better cosmetic outcome. Follow up at regular intervals has to be done for evaluation of recurrence or transformation into BCC [11]. Malignant transformation into BCC requires wide surgical excision with tumour negative margins and followed by adjuvant radiotherapy [12].
Conclusion
Trichoepithelioma is a benign tumour of follicular origin that presents as solitary or multiple familial trichoepitheliomas. Out of three cases in our study, two are solitary and in one case along with the patient other family members got affected. They can undergo transformation to malignant neoplasms such as basal cell carcinoma. The history, clinical features and histopathological findings were suggestive of the evolution of basal cell carcinoma directly from trichoepithelioma in our first two cases, but in the third case TE and BCC were separate lesions on face and we are uncertain about whether the BCCs developed independently or by transformation from a trichoepithelioma. Careful examination and Follow up is needed for these patients to look for any rapid growth or ulceration in the pre-existing lesions that may indicate malignant transformation.
[1]. Brooke HG, Epithelioma adenoids cysticumBr J Dermatol 1892 4:269 [Google Scholar]
[2]. Calonje E, Tumours of the skin appendages. In: Burns T, Breathnach S, Cox N, Griffiths C, editorsRook’s Textbook of Dermatology 2010 ChichesterWiley-Blackwell [Google Scholar]
[3]. Mosby SP, Naidu MN, Ranpise SG, Magar S, TrichoepitheliomaJ Indian Acad Oral Med Radiol 2011 23:448-50. [Google Scholar]
[4]. Yiltok SJ, Echejoh GO, Mohammad AM, Ituen AM, Igoche MI, Dades OT, Multiple Familial Trichoepithelioma: A case report and Review of literatureNiger J Clin Pract 2010 13:230-32. [Google Scholar]
[5]. Heidarpour M, Rajabi P, Sajadi F, CD10 expression helps to differentiate basal cell carcinoma from trichoepitheliomaJ Res Med Sci 2011 16:938-44. [Google Scholar]
[6]. Mapar MA, Ranjbari N, Afshar N, Karimzadeh I, Karimzadeh A, Severely disfiguring multiple familial trichoepitheliomas with basal cell carcinomaIndian J Dermatol Venereol Leprol 2014 80:349-52. [Google Scholar]
[7]. Sangwaiya A, Sharma J, Sharma S, Munghate A, Samal S, Sen R, Multiple familial trichoepithelioma with an adjacent basal cell carcinoma, transformation or collision – A case report and review of literatureIndian J Dermatol 2015 60:280-83. [Google Scholar]
[8]. Poniecka AW, Alexis JB, An immunohistochemical study of basal cell carcinoma and trichoepitheliomaAm J Dermatopathol 1999 21:332-36. [Google Scholar]
[9]. Lee YF, Chang YT, Liu HN, Differentiating Basal Cell Carcinoma from Trichoepithelioma by Using Androgen Receptor ExpressionDermatol Sinica 2009 27:154-60. [Google Scholar]
[10]. Sahin MT, Demir MA, Inguinal keratotic Basal cell carcinoma mimicking giant solitary trichoepitheliomaJ Dermatol 2003 30:395-99. [Google Scholar]
[11]. Teli B, Thrishuli PB, Santhosh R, Amar DN, Rajpurohit S, Giant solitary trichoepitheliomaSouth Asian J Cancer 2015 4:41-44. [Google Scholar]
[12]. Martinez CA, Priolli DG, Piovesan H, Waisberg J, Nonsolitary giant perianal trichoepithelioma with malignant transformation into basal cell carcinoma: Report of a case and review of the literatureDis Colon Rectum 2004 47:773-77. [Google Scholar]