Increase in blood pressure is a grave risk factor considering the population health. It not only increases the risk of coronary heart disease and ischaemic and haemorrhagic stroke, but is also associated with numerous complications like heart failure, peripheral vascular disease, renal impairment, retinal haemorrhage and visual impairment. Moreover, literatures suggest that interventions targeted to reduce the blood pressure below the level of 140/90 mm of Hg reduce such risk substantially [1]. In recent years, there has been a sharp rise in the magnitude of the problem of hypertension across the world. Globally 7.5 million deaths are attributable to hypertension which constitutes about 12.8 % of all deaths, which in turn accounts for more than fifty million disability adjusted life years (DALYS) or 3.7% of total DALYS [1]. Regarding the burden of the disease, the overall prevalence among adults aged 25 years or above was around 40% globally, while in India it was more than one fifth of the total population of that age group [2].
It has been estimated that a rise in systolic BP by only 5 mm of Hg would result in approximately 25% increase in the chances of fatal stroke and fatal myocardial infarction [3]. While such findings substantiate the catastrophic consequences of underestimating blood pressure in an individual, it has been estimated that overestimation of true blood pressure by same level would result in inappropriate treatment with anti-hypertension medications in almost 30 million Americans. They would also be exposed to adverse drug effects, psychological effects of misdiagnosis, and unnecessary cost [4]. Therefore, accurate estimation of blood pressure up to the error level as low as 5 mm of Hg is of supreme importance at the age of growing enigma of hypertensive disorders.
For correct estimation of BP in non-invasive setting Mercury sphygmomanometers are considered as gold standard for long [5]. But the fear of percious effect of potential mercury toxicity and the problems associated with disposal of mercury, has led to decrease use of mercury instruments worldwide. For the same reason European Union directed phasing out of Mercury instruments recently [6]. Non-mercury sphygmomanometers like aneroid and more recently, digital ones have replaced the use of traditional Mercury instruments in many settings. Additional advantage of anaeroid instrument is the portability [7], while that of digital instruments are ease of use in view of the obvious fact that the latter obviates the need of auscultation skill of the examiner. In a large study at this outset in UK examined the comparability of measurement accuracy of all the three categories of sphygmomanometer and found that digital instruments are almost as accurate as mercury instruments, while higher failure rate existed with the aneroid ones and therefore the authors recommended the use of inexpensive and easy to use digital instruments by general practitioner during home visit [7]. However, such evidences are scanty in Indian context, where there is an obvious need of more feasible and inexpensive instruments because of large population size, increased poverty and decreased tendency to seek institution based medical care.
In this context we conducted this study to compare the accuracy of readings of aneroid and digital sphygmomanometers in reference to mercury sphygmomanometers and determine the hypertensive classification agreement between the mercury and non-mercury devices.
Materials and Methods
This was a clinic-based cross-sectional analytical study to conduct diagnostic accuracy of two instruments: aneroid sphygmomanometer and digital sphygmomanometer. In an OPD of the primary health centre under the purview of our institute, we examined all the subjects above the age of 25 years, in two days per week, selected randomly from five working days per week in a period of one month (January, 2015-February, 2015). The age criteria was selected so, because we experienced 0% hypertension in the OPD among individual aged 25 years or less, who reported in the OPD in the previous one month. The total number of participants was found to be 218. For the measurement of blood pressure in each individual we used 3 types of sphygmomanometers: The readings of Aneroid sphygmomanometer (MDF808B) and Digital sphygmomanometer (Omron Hem-7111) were compared to that of a mercury sphygmomanometer (NOVAPHON). All the instruments were checked, standardized and calibratedby experts. Approval of the Institutional Ethics Committee and informed consent from the study participants were taken.
Measurement of Blood Pressure: Standard operating procedure for measuring blood pressure was followed [5]. It was ensured that the study participants were relaxed at-least for 10–15 min before measurements and were seated with legs uncrossed and back supported and arm was supported at heart level before the measurements. Cuffs of appropriate sizes were used [5]. Blood pressure of each participant was measured twice by each instrument and average of the two readings was noted down in a data entry form. All the individual blood pressure measurements of the study participants were repeated at 30 second intervals.
Statistical Analysis
To find out the mean difference of estimated blood pressures among all individuals by the three instruments, paired t-tests were performed. Agreement of measurement between aneroid and gold standard (mercury instrument) and between digital and gold standard (mercury instrument) was analysed using kappa coefficient and sensitivity and specificity were estimated. Receiver Operating Characteristics (ROC) curve analyses were performed to find out the accuracy of estimate of the test instruments (aneroid and digital) in reference to mercury instrument and respective cut-off values were determined by calculating Youden index.
Results
Mean age of the 218 individuals studied was 54.9 years. (±12.9). The blood pressure measured by each non mercury device was compared with respect to the measurements done by the mercury instrument (gold standard).
1. Comparing the readings of blood pressure measured: [Table/Fig-1] shows the percent distribution of absolute differences of the readings between the mercury and non- mercury devices separately within 0-3, 4-5, 6-10, 11-15 and 16+ mm Hg. categories. Absolute agreements within 5 mm Hg. is considered the accepted threshold for acceptance of the accuracy of the equipment with respect to the gold standard equipment (mercury device) [8]. In our study the absolute difference within 5 mm Hg. between mercury and aneroid for systolic and diastolic blood pressure were 89.4% and 91.7% of the readings respectively. While the absolute difference of within 5 mm Hg. between mercury and digital for systolic and diastolic blood pressure were 25.2% and 43.6% of the readings respectively.
Bar graph showing the percentage distribution of the absolute differences of readings between the mercury and aneroid and between mercury and digital devices for measuring systolic and diastolic blood pressure
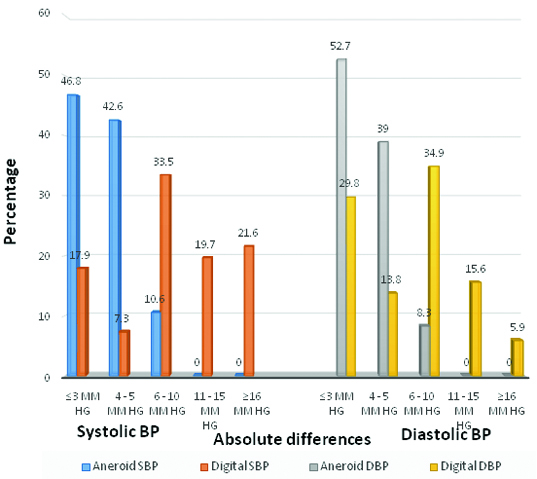
For systolic and diastolic blood pressure treated separately the mean difference between the test device and the mercury sphygmomanometer should be ±5 mm Hg or less, with a standard deviation of 8 mm Hg or less [8]. The correlation between the mercury readings and the aneroid device (r=0.98 systolic, r=0.84 diastolic: p<0.001 for both) and between mercury and digital device (r=0.95 systolic, r=0.67 diastolic: p < 0.001 for both) were statistically significant. The paired sample t-test [Table/Fig-2] showed the mean difference between mercury and aneroid readings to be 1.5 (SD 3.2) and 1.8 (SD 2.9) for systolic and diastolic blood pressure respectively, while the mean difference between mercury and digital device was – 7.2 (SD 10.1) and -2.0 (SD 8.3) for systolic and diastolic blood pressure respectively.
Means & Mean Difference of Blood Pressure (Systolic and Diastolic): Mercury Sphygmomanometer verses aneroid sphygmomanometer and Mercury sphygmomanometer verses digital sphygmomanometer (n=218).
| Blood Pressure | Mercury:Mean (SD) | Aneroid:Mean (SD) | Digital:Mean (SD) | Mercury vs aneroid:Mean difference (SD) | Mercury vs digital:Mean difference (SD) |
|---|
| Systolic | 139.7 (17.9) | 138.2(17.6) | 146.9(18.4) | 1.5(3.2)* | -7.2(10.1)* |
| Diastolic | 77.9 (9.4) | 76.1 (9.1) | 79.9(10.7) | 1.8(2.9)* | -2.0(8.3)* |
Test of significance with paired t test.; * p < 0.001
2. Comparison of devices on hypertension classification agreement: [Table/Fig-3] shows the agreement between the test device with the mercury device while classifying the patients as hypertensives and non-hypetensives. Individuals having blood pressure more than 140/90 mm Hg detected by mercury sphygmomanometer were considered to be hypertensives. The kappa agreement were 0.88 and 0.39 for the aneroid and digital devices respectively (both were statistically significant). The aneroid device has correctly diagnosed 86.7% of hypertensives and 98.7% of normotensives whereas the digital device has correctly diagnosed 80.0% and 67.7% of normotensives.
Diagnosis of hypertensive, by mercury and non-mercury (aneroid & digital) devices. (n=218)
| Device and agreement | | | Mercury | | | Mercury |
|---|
| Hypertension | Hypertension |
|---|
| Yes | No | Yes | No |
|---|
| Device | Aneroid | Yes | 52 | 2 | Digital | Yes | 48 | 51 |
| No | 8 | 156 | No | 12 | 107 |
| Agreement statistics |
| Aneroid Device | Digital Device |
| Kappa | 0.881 | 0.397 |
| Sensitivity | 86.7 % | 80.0 % |
| Specificity | 98.7 % | 67.7 % |
| Positive predictive value | 96.3% | 88.9 % |
| Negative predictive value | 95.1% | 65.24 % |
| Likelihood ratio of positive test (LR+) | 66.7 | 247.7 |
| Likelihood ratio of negative test (LR-) | 0.13 | 0.3 |
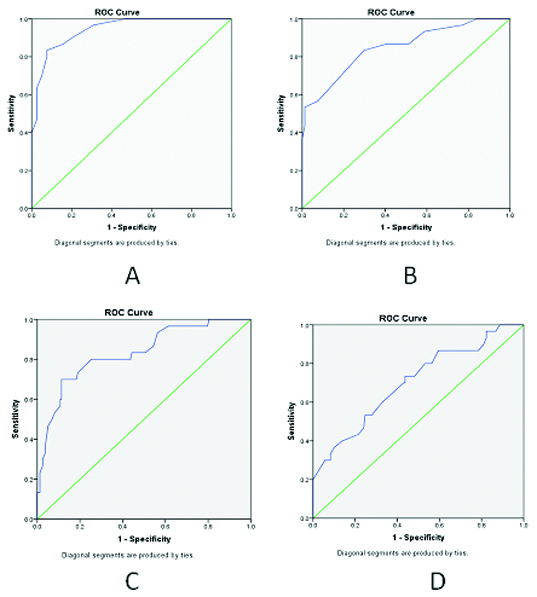
[Table/Fig-4] shows the analysis of Receiver Operating Characteristic (ROC) curve (shown in [Table/Fig-5]) which showed the area under the curve for systolic blood pressure in aneroid and digital device was 0.94 (95% CI 0.91-0.97), 0.83 (95% CI 0.77-0.89) respectively whereas for diastolic blood pressure measured by aneroid and digital device was 0.85 (95% CI 0.79-0.91) and 0.7 (95% CI 0.62-0.78) respectively. In ROC curve analysis more the area under the curve, more is the diagnostic accuracy of the test. The results showed that the area under the curve for both systolic and diastolic blood pressures measured by aneroid devices was more than that of the measurements done by digital device and it clearly depicts that, the diagnostic accuracy of aneroid sphygmomanometer was better than digital sphygmomanometer for measuring both systolic and diastolic blood pressures. The Youden index (sensitivity + specificity -1) which is calculated to detect the optimal threshold to detect a disease from the data analysis of ROC curve was done. It showed (not shown in the table) that the optimal cut off of the readings of non-mercury sphygmomanometers to detect hypertension (with reference to the gold standard mercury sphygmomanometers) was different. In case of the aneroid devices if the blood pressure readings are more than 143/79 mm Hg then the patient should be called to have hypertension while in case of measurement by a digital device, a blood pressure reading above 149.5/84.5 mm Hg should considered as the benchmark to classify the patient as hypertensive.
Comparison of the result of Receiver operating characteristic curve (ROC) curves.
| Type of device | Blood Pressure | Area under the curve (95% CI) | Optimal cut-off to detect Hypertension (Youden Index) |
|---|
| Aneroid | Systolic | 0.94 (0.91-0.97) | 143 mm Hg. |
| Diastolic | 0.85 (0.79-0.91) | 79 mm Hg. |
| Digital | Systolic | 0.83 (0.77-0.89) | 149.5 mm Hg. |
| Diastolic | 0.70 (0.62-0.78) | 84.5 mm Hg. |
Receiver operating characteristic curve (ROC) curves for Aneroid and Digital Systolic and Diastolic blood pressure measurements
A: Receiver operating characteristic curve (ROC) for systolic blood pressure measured by aneroid device.
B: ROC for diastolic blood pressure measured by aneroid device.
C: ROC for systolic blood pressure measured by digital device.
D: ROC for diastolic blood pressure measured by digital device.
Discussion
The study was conducted to determine and compare the accuracy of non-mercury instruments and their ability to correctly diagnose hypertension. An aneroid and a digital instrument were selected for the purpose and were judged with respect to a properly calibrated mercury sphygmomanometer (Gold standard).
The mean difference and standard deviation of the aneroid device is within the accepted threshold (±5 mm Hg or less, with a standard deviation of 8 mm Hg or less) recommended by the Association for the Advancement of Medical Instrumentation guidelines (AAMI, 2008) [8] but the digital device failed to achieve that. This suggested the superiority of aneroid devices with respect to digital instruments in accurately measuring blood pressure in primary care setting.
We also found that the agreement between the mercury and aneroid device in classifying hypertension was very high (kappa= 0.881, p<0.001). However, only moderate agreement was found between digital and mercury device (kappa= 0.397, p<0.001) in this respect. This suggested the greater ability of the aneroid instruments in classifying an individual as hypertensive or normotensive. This is particularly important because such classification needs to be very accurate so that all the diseased get the opportunity in receiving treatment and the non-diseased are not exposed to hazards related to cost and adverse effects of drugs and mental agony because of wrong diagnosis.
In the validity analysis we studied whether the aneroid and digital devices produced accurate results (one that lacked systematic error) by calculating sensitivity, specificity, positive and negative predictive value; the mercury device being considered as a gold standard. All the indicators showed better results for aneroid device in comparison to the digital device. The area under the ROC curve for both systolic and diastolic blood pressure was much larger for aneroid than digital devices suggesting that aneroid device was better detector of hypertension than the digital device. When we estimated the Youden index from the sensitivity and specifity of cut-offs, we also found that for the detection of hypertension, the optimal cut off should be different for aneroid and digital device as in comparison to the standard 140/90 mm Hg. as measured by a mercury sphygmomanometer. This is important in the current context because we presently have same criterion for detecting hypertension measured by all the devices.
The findings of our study were in contradiction to the findings of following studies conducted previously with similar objectives:
In a study done by NHANES the mean difference of SBP and DBP in the digital device compared to mercury device is -1.6 (SD 6.8) and -1.6 (SD 7.8) and the Kappa for digital device is 0.72 [9]. However, such contradiction in findings may be attributed to the use of different model of the digital instrument.
In another study among more than 8000 patients researchers used 604 sphygmomanometers (53% digital, 32% aneroid, 13% mercury and 2% hybrid devices). They found that only 78% of the aneroid models were able to give accurate measures, while 88% digital devices were accurate, considering acceptable error of 3 mm of Hg [7]. In our study, we examined the accuracy of single instrument of each type and found the aneroid device to be superior than the digital device. This may be attributed to the stringent acceptable error criteria of the former study, which accepted only errors within 3 mm oh Hg which was much narrower than our criteria of 5 mm of Hg. This explanation can be substantiated with the findings of another study, in which researchers aimed to measure the accuracy of 283 aneroid devices and found that 100% of the aneroid devices were accurate in estimating blood pressure within the range recommended by the Association for the Advancement of Medical Instrumentation [10]. In our study we used the same criteria of acceptability. Another potential reason of difference in finding may be that aneroid devices needed yearly maintenance. A yearly calibration with a standard of 2 mm of Hg error has been found to improve accuracy of the aneroid instrument [11]. In our study we used new, out-of-box instruments for measurement, which might have resulted in greater accuracy of aneroid device.
However, in a similar study like that of ours, but with a randomized single visit cross-over design, among 95 individuals, researchers found the aneroid device performing much better than digital device. With same error criteria of 5 mm of Hg as that of our study, they found that aneroid monitor could correctly estimate 54% of the systolic and 58% of the diastolic blood pressures in comparison to only 34% of the correct systolic and 48% of the correct diastolic measurement by digital instrument [12]. In another study, with smaller sample size than that of our study, the researchers also observed that aneroid instruments were significantly more accurate than digital instruments of both arm and wrist type. The systolic blood pressure was particularly overestimated in case of arm type digital instruments [13]. The implication that the aneroid devices are more accurate would also add to the evidence substantiated in a review that measurement of blood pressure using aneroid devices are accurate provided the device maintenance and handling are conducted properly [14].
Use of more advanced statistical techniques using ROC curve estimation, and Youden Index calculation, furthermore substantiated the evidence gathered from our study and we additionally found the evidence that aneroid devices were superior to digital devices in classifying hypertensive and non-hypertensive individuals apart from the findings of agreement of mean and kappa statistic.
The major strength of this study was conducting research in primary care OPD setting, which has been set as the first opportunity of contact between people of the country and the doctor in government system. Additionally blood pressure of each individual by all the three instruments was measured by a single examiner, who was a doctor. This obviated the chance inter-rater difference in measurement of blood pressure. Thirdly, we analysed the blood pressure of the individuals measured by three separate instruments by both norm reference and criterion reference analyses. Therefore, we were able to find out the accuracy of exact measurement of the value of blood pressure as well as classify individuals between hypertensive and normotensive category. Fourthly, we estimated appropriate cut-off values for both aneroid and digital instrument and this was never performed before while comparing the two instruments.
Limitation
The major limitation of the study was that it was conducted within the OPD climate, which carried with itself the chances of bias due to studying individuals seeking health service only, and the result cannot be generalised to all individuals of the community. Secondly, we used only one instrument of each type and therefore from this study it is impossible to conclude the overall effectiveness of aneroid and digital instruments, when batches of instruments are used in institution. Thirdly, we performed the study in only one health centre, in one season only. Considering possible error of aneroid BP in changing temperature and climate, larger study will be needed encompassing multiple sites with different climate and in different time of the year to conclusively compare the effectiveness of the two instruments; aneroid and digital.
Conclusion
Our study revealed the greater effectiveness of aneroid device in comparison to digital device in measuring blood pressure among individuals aged 25 years or more in the setting of primary health centre on out-patient basis. The findings implicated that the digital devices should be used with caution, doubt and suspicion. If they are at all used, we suggest that different cut-off level of hypertension should be used for making correct diagnosis of hypertension.
Finally, from our study we conclude that the sensitivity and specificity of digital sphygmomanometers, though is easy to use, requiring no expertise at all, are not up to standard. If used in the community for screening there will be many people who either will be wrongly or misdiagnosed of hypertension. The field staff and the community itself are often attracted to use digital sphygmomanometer because of its easy to use features requiring no expertise at all. If this instrument is taken up for use by the health personnel for detection of hypertension it may prove disastrous as far as detection, management and treatment of hypertension are concerned.
Test of significance with paired t test.; * p < 0.001