Pathogenesis and Management of Hepatolithiasis: A Report of Two Cases
Biswajit Dey1, Gourav Kaushal2, Sajini Elizabeth Jacob3, Adarsh Barwad4, Biju Pottakkat5
1 Senior Resident, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
2 Senior Resident, Department of Surgical Gastroenterology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
3 Associate Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
4 Assistant Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
5 Professor, Department of Surgical Gastroenterology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Biswajit Dey, Senior Resident, Department of Pathology, JIPMER, Pondicherry-605006, India. E-mail : drbish25@rediffmail.com
Hepatolithiasis or primary intrahepatic stones are prevalent in the Far-East countries such as Korea, Japan and Taiwan. It has been associated with helminthiasis, bacterial infections, environmental and dietary factors. Despite high prevalence of helminthiasis like ascariasis, poor environmental condition and low protein diet, India and Middle-East countries have a low incidence of hepatolithiasis. We report two cases of hepatolithiasis associated with bacterial infections and were surgically managed. The first case is a 45-year-old female presenting with upper abdominal pain and fever. She had multiple calculi in intrahepatic biliary radicles, common bile duct, common hepatic duct and gall bladder. She was managed by cholecystectomy, left lateral liver sectionectomy, choledochoscopy assisted stone clearance of the residual liver and Roux-en-Y hepatico-jejunostomy. The second case is a 60-year-old female presenting with epigastric pain and fever and past history of cholecystectomy for cholelithiasis. She had multiple right and left intrahepatic calculi and managed by left lateral liver sectionectomy with excision of CBD and Roux-en-Y hepatico-jejunostomy. Both the cases showed growth of bacteria in the culture of the intraoperatively collected bile.
Case Reports
Case 1
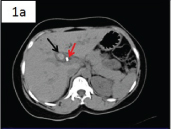
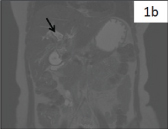
A 45-year-old female presented with intermittent upper abdominal pain for two months and fever for two weeks. On general examination she was icteric. On investigation, haemoglobin was 10.6 gm%, total leucocyte count was 5,700 /cmm and platelet count of 3 lacs /cmm. Biochemical parameters showed serum bilirubin of 3.9 mg/dl, aspartate aminotransferase (AST) of 184 IU/L and alanine aminotransferase (ALT) of 421 IU /L. Serology for hepatitis-B virus and hepatitis-C virus were negative. Ultrasonography (USG) abdomen showed cholelithiasis and right and left intrahepatic calculi. Contrast enhanced computed topography (CECT) showed dilated intrahepatic biliary radicles and multiple stones in both right and left hepatic ducts [Table/Fig-1a]. Magnetic Resonance Cholangio-Pancreaticography (MRCP) showed multiple calculi in intrahepatic biliary radicles, common bile duct (CBD), common hepatic duct and gall bladder, largest at level of cystic duct measuring 1.8x1.4cm [Table/Fig-1b]. She underwent endoscopic retrograde cholangiography (ERC), clearance of few CBD stones and stenting of CBD. However patient continued to have symptoms. Therefore the patient was considered for surgical management.
CECT showing intrahepatic Stones (black arrow) with stent in-situ (red arrow);
MRCP showing stones in right hepatic duct (arrow);
Cholecystectomy, left lateral liver sectionectomy, choledochoscopy assisted stone clearance of the residual liver and Roux-en-Y hepatico-jejunostomy was performed. Intraoperatively, gall bladder was contracted and thick walled and contained multiple stones. Multiple stones were present in both the extra and intra-hepatic bile ducts. Segment 2 and 3 were studded with stones. Intraoperatively collected bile was sent for culture, which showed presence of Klebsiella pneumoniae.
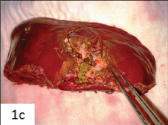
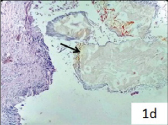
Cut section of the liver specimen showed dilated intrahepatic ducts impacted with yellowish stones [Table/Fig-1c]. Histopathological examination of the liver specimen showed multiple dilated intrahepatic ducts with denuded lining epithelium and containing crystalline stones [Table/Fig-1d]. Adjacent liver parenchyma showed lymphocytic infiltrate. She was discharged eight days after surgery without any complications.
Cut section of the liver showed dilated intrahepatic ducts impacted with yellowish stones;
Histopathology showed multiple dilated intrahepatic ducts with denuded lining epithelium and containing crystalline stones (arrow) (H&E, 100X).
Case 2
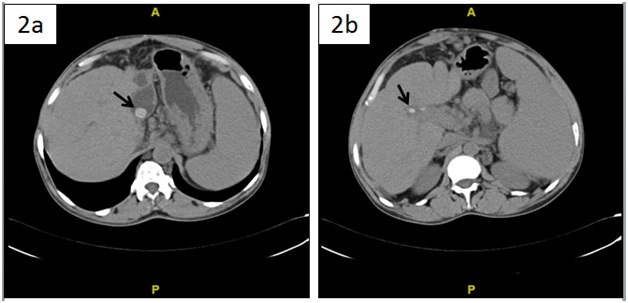
A 60-year-old female presented with dull aching intermittent pain in the epigastric region for one year and fever for four days. There was no history of jaundice. She underwent open cholecystectomy with common bile duct exploration 15 years back for cholelithiasis and choledocholithiasis. She had cerebrovascular accident with left hemiparesis four and a half years back which was treated conservatively and improved. She was icteric. Mild tenderness was present in right hypochondrium and liver was palpable about three cm below the right costal margin. On investigation, haemoglobin was 8.8 gm%, total leucocyte count was 10,700 /cmm and platelet count was 4 lacs/cumm. Liver function tests revealed serum bilirubin of 4.2 mg/dl, alkaline phosphatase of 736 IU /L, AST of 381 IU/L and ALT of 188 IU /L. USG abdomen showed right and left intrahepatic calculi and dilated CBD. CECT showed multiple bilateral intrahepatic calculi with atrophy of segment 2 and 3 of liver [Table/Fig 2a,b]. Similar findings were also noted in MRCP.
CECT showing multiple bilateral intrahepatic calculi (arrow).
A left lateral liver sectionectomy with excision of CBD and Roux-en-Y hepatico-jejunostomy were performed. Intraoperatively liver was smooth and firm with atrophy of segment 2 and 3 of liver. There were large pigment stones in the CBD and large stones were palpated inside the left lateral segment. intraoperative bile was white in color with purulent flakes. Bile culture showed growth of pseudomonas aeruginosa.
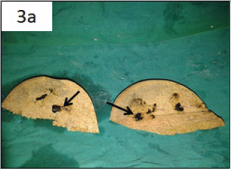
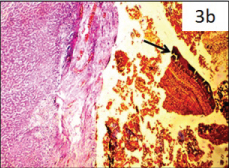
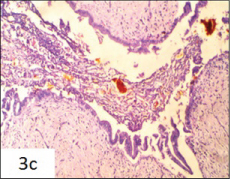
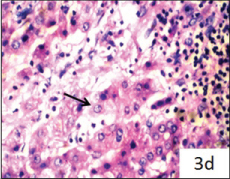
Grossly, the specimen showed focal exudates and dilated intrahepatic ducts impacted with brown pigment stones [Table/Fig-3a]. Histopathological examination of the specimen showed multiple dilated intrahepatic ducts containing brownish stones [Table/Fig-3b]. There was evidence of periductal lymphoplasmacytic infiltrate along with neutrophils [Table/Fig-3c]. Surrounding hepatocytes showed feathery degeneration, focal intrahepatic and canalicular cholestasis [Table/Fig-3d]. Postoperatively patient had transient bile leak which was settled spontaneously. She was discharged 11 days after surgery.
Cut section of the liver showed intrahepatic ducts impacted with brown pigment stones arrow);
Histopathology showed multiple dilated intrahepatic ducts containing brownish stones (arrow) (H&E, 100x);
There was evidence of periductally mphoplasmacytic infiltrate alongwith neutrophils (H&E, 100x);
Hepatocytes showed feathery degeneration (arrow), focal intrahepatic and canalicular cholestasis (H&E, 400x).
Discussion
Hepatolithiasis is endemic to East Asia with prevalence of 30% to 50% [1]. In the west, it is generally thought to be secondary to gall bladder stones or primarily associated with sclerosing cholangitis, benign biliary strictures, choledochal cysts or malignant biliary tumours [2,3]. In the East it is regarded as a separate entity altogether. The majority of cases are associated with recurrent pyogenic cholangitis in regions with parasitic infestations like ‘Ascaris lumbricoides’ and ‘Clonorchis sinesis’ [2–4]. Co-existence of parasitic infestations appears to be incidental rather than causative [4]. Incidence of bacteria in bile of patients with hepatolithiasis is nearly 100% [3,5]. The commonly found bacteria are Klebsiella species, Escherichia Coli, Pseudomonas species, Entercoccous species and Bacteroides species [5]. Most of the bacterial species found in the bile of patients with hepatolithiasis show β-glucoronidase activity, which catalyzes the hydrolysis of direct bilirubin to the indirect unconjugated form. Unconjugated bilirubin is water-insoluble and combines with calcium to form calcium bilirubinate (pigment) stones which comprise the majority of the cases of hepatolithiasis [6]. In the present cases, bile culture showed presence of pseudomonasaeruginosa and Klebsiella pneumoniae. In contrast, hepatolithiasis in the west is composed of cholesterol. Acquired and/congenital metabolic factors have been implicated in the development of cholesterol hepatolithiasis [4].
Diet has also been implicated in the pathogenesis of hepatolithiasis. Asian diet is rich in carbohydrates and low in fat and protein. Low fat causes decreased release of cholecystokinin leading to biliary stasis whereas low protein leads to low level of Glucaro-1,4 lactone which is an inhibitor of β-glucuronidase, potentiating the deconjungation reaction [3].
Clinically the patients of hepatolithiasis may be asymptomatic or present with symptoms like upper abdomen or right upper quadrant pain, fever and jaundice [3,4]. In severe cases, it may progress to formation of hepatic abscess and biliary sepsis [4]. In asymptomatic patients, it is an incidental finding on radiological imaging studies [4]. However, there is no pathognomonic symptom or sign in patients with hepatolithiasis. Association of cholangiocarcinoma with hepatolithiasis is known and its prevalence in hepatolithiasis patients ranges from 2.4% to 10% [4,7]. The causative process for the development of cholangiocarcinoma in hepatolithiasis has been linked to mucosal adenomatous hyperplasia and chronic proliferative cholangitis due to chronic bacterial infection, bile stasis and mechanical irritation of hepatolithiasis [8]. The risk of cancer is higher in calcium bilirubinate hepatolithiasis as compared to cholesterol hepatolithiasis [4].
The different evaluation modalities include USG abdomen for ductal dilatation and calculi, CECT abdomen to discern hepatic architecture and atrophy and MRCP or ERCP for mapping of the biliary tree [2,6].
Several management strategies have been proposed ranging from non-surgical modalities to surgical options. Non-invasive treatments include radiological (percutaneous transhepatic cholangiography with or without lithotripsy) or endoscopic (endoscopic retrograde cholangiopancreatography with or without lithotripsy) guidance [4,6,7,9]. Percutaneous transhepatic cholangioscopic lithotripsy (PTCSL) is done for stone removal and dilation of strictures in right-sided, bilateral or recurrent disease [1]. Extracorporeal shock wave lithotripsy (ESWL) is used for extraction of cholesterol stones and holmium (Ho): YAG laser for calcium bilirubinate stones [1]. However, postoperative residual and recurrent stones occur in 20% of patients treated with non-surgical procedures [9]. Surgical management includes liver lobectomy or segmental resection [6,8,9]. Indications for surgical management include unilobar hepatolithiasis particularly left-sided, atrophy or abscess of a liver segment/lobe, possibility of concomitant cholangiocarcinoma and localized intrahepatic calculi with biliary strictures [1, 4,9]. The advantage of treating hepatolithiasis by liver lobectomy or segmental resection is that all hepatic stones can be removed alongwith the pathologic bile ducts, which reduces the risk of recurrence [1,9]. In the first case, the patient had atrophy of segments 2 and 3 and in the second case, multiple stones were impacted in the peripheral ducts of segment 2 and 3, which were not amenable to choledocoscopic clearance. Hence both patients were managed by left lateral sectionectomy.
Wound infection and bile leakage are the major complications of surgery for hepatolithiasis [10]. These are comparable with or less than those for non-surgical techniques [10]. In the second case, the patient had transient bile leak which was settled spontaneously.
Conclusion
Hepatolithiasis are associated with bacterial infections, helminthiasis and dietary factors. Presence of bacteria in the bile of the patients with hepatolithiasis is found in almost all cases and should be sent for culture. Several management strategies have been proposed ranging from non-surgical to surgical modalities.However, optimal management of hepatolithiasis poses a challenge for hepatobiliary surgeons.
[1]. Feng XB, Zheng SG, Xia F, Ma KS, Wang SG, Bie P, Classification and management of hepatolithiasis: A high volume, single centre’s experienceIntractable Rare Dis Res 2012 1:151-56. [Google Scholar]
[2]. Pilankar KS, Amarapurkar AD, Joshi RM, Shetty TS, Khithani AS, Chemburkar VV, Hepatolithiasis with biliary ascariasis – a case reportBMC Gastroenterol 2003 3:35 [Google Scholar]
[3]. NitinRao AR, Chui AK, Intrahepatic Stones – an aetiological quagmireIndian J Gastroenterol 2004 23:201-02. [Google Scholar]
[4]. Sakpal S, Babel N, Chamberlain R. Surgical management of hepatolithiasisHPB (Oxford) 2009 11:194-202. [Google Scholar]
[5]. Sheen-Chen SM, Chen W, Eng H, Sheen C, Chou F, Cheng Y, Bacteriology & Antimicrobial choices in HepatolithiasisAm J Infect Control 2000 28:298-301. [Google Scholar]
[6]. Nakayama F, Intrahepatic StonesBlumgart’s Surgery of the Liver & Biliary Tract 1994 :765-774. [Google Scholar]
[7]. Kayhan B, Akdoğan M, Parlak E, Ozarslan E, Sahin B, Hepatolithiasis: a Turkey experienceTurk J Gastroenterol 2007 18:28-32. [Google Scholar]
[8]. Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ, Outcomes of hepatectomy for hepatolithiasisWorld J Surg 2007 31:479-82. [Google Scholar]
[9]. Uchiyama K, Onishi H, Tani M, Kinoshita H, Ueno M, Yamaue H, Indication and Procedure for Treatment of HepatolithiasisArch Surg 2002 137:149-53. [Google Scholar]
[10]. Li SQ, Liang LJ, Peng BG, Lai JM, Lu MD, Li DM, Hepatico-jejunostomy for hepatolithiasis: a critical appraisalWorld J Gastroenterol 2006 12:4170-74. [Google Scholar]