Binge Eating Leading to Acute Gastric Dilatation, Ischemic Necrosis and Rupture –A Case Report
Manish Dewangan1, Manish Kumar Khare2, Sumanta Mishra3, Jogesh Chandra Marhual4
1 Surgical Specialist, Department of General Surgery, JLN Hospital & Research Centre, Bhilai (CG), India.
2 Assistant Professor, Department of Surgery, CM Medical College, Durg (CG), India.
3 Joint Director, Department of General Surgery, JLN Hospital & Research Centre, Bhilai (CG), India.
4 Joint Director, Department of General Surgery, JLN Hospital & Research Centre, Bhilai (CG), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Dewangan, Street-16,14/A, Hospital Sector, Bhilai (CG)-490009, India. E-mail : drmanishd78@gmail.com
Acute gastric dilatation is a rarely encountered clinical scenario in our day to day practice. This is very rapidly progressing condition and can lead to ischemic necrosis and perforation/rupture of the stomach. It could be fatal if not timely intervened. We report such a case of a 17-year-old, otherwise healthy boy, who presented with pain and distension of abdomen following binge eating episode after 24 hours of prolonged fasting. On exploration, stomach was dilated with necrosis and perforation at fundus near greater curvature. He was managed with excision of all the devitalized area and primary repair with feeding jejunostomy. The case is presented due to its rarity. Acute gastric dilatation (AGD) leading to ischemic necrosis and perforation because of binge eating episode in an otherwise healthy person is an exceptional occurrence with only few cases reported in literature. The clinician should be aware of this condition for prompt and appropriate management.
Gastric ischemia, Gastric ischemic necrosis, Spontaneous gastric rupture, Spontaneous gastric perforation
Case Report
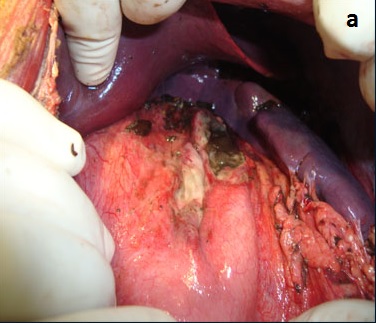
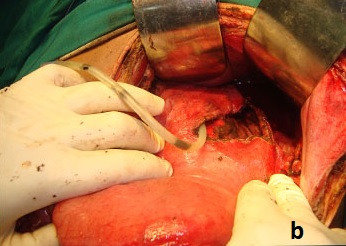
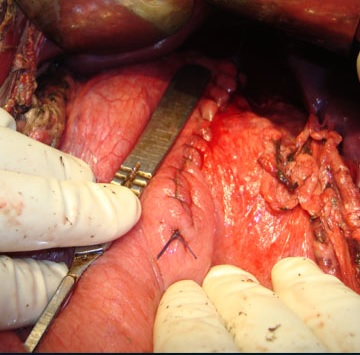
A 17-year-old boy presented to emergency in the night with severe pain and distension of abdomen after dinner of previous night. Total duration of pain was almost 24 hours. On the previous day, patient has kept fast due to some religious reasons for the whole day. Total duration of fasting was prolonged to almost 24 hours (including overnight fasting). He has taken heavy meals in the night on the day of fast. The amount of meal was more than what he normally used to consume. He felt abdominal discomfort after sometimes and went to bed. He developed abdominal fullness and retching but he was unable to vomit. In the morning, his distension was not relieved and pain started. He consulted general practitioner and was given Proton pump inhibitor and analgesic but his symptoms persisted and pain got aggravated with time. In the night he was referred to us for further management. The boy and his parents did not reveal any history of eating disorder or psychiatric illness. There was no history of drug abuse, corrosive intake, trauma or any previous abdominal surgery. On examination, his vitals were stable with no fever. His abdomen was distended and there was generalized tenderness and guarding. Plain X-ray abdomen demonstrated pneumoperitoneum. Blood investigations revealed haemoglobin of 15.7 grams per deciliter, total leucocytes 19700 per cubic millimeter with 88% neutrophils. His blood sugar, renal profile and electrolytes were unremarkable. Patient was kept Nil per orals and nasogastric tube (14 Fr) was inserted. Exploratory Laparotomy was performed. On exploration, there was about 5 litres of free fluid and undigested food particles in the abdominal cavity. Stomach was hugely dilated with a perforation on the anterior wall of stomach at fundus near greater curvature. There was a necrotic patch surrounding perforation [Table/Fig-1a]. Whole of the necrotic tissue was excised [Table/Fig-1b]. Primary repair of the defect was performed in single layer absorbable suture [Table/Fig-2]. Feeding jejunostomy (FJ) was done. Feeding started through FJ tube after 24 hours and oral feeds resumed on 7th postoperative day. Recovery was uneventful.
Intraoperative view of stomach showing necrosis and perforation at fundus.
Intraoperative view of dilated stomach with debridement of all necrotic area showing nasogastric tube in the stomach.
Stomach after primary repair.
Discussion
Ischemic necrosis of the stomach with perforation due to acute gastric dilatation (AGD) is a very rare clinical condition. The reported causes of gastric necrosis include intrathoracic herniation, volvulus, acute necrotizing gastritis, corrosive ingestion, vascular compromise, and AGD. About half of the cases seem to be related to large meals and/or acute gastric dilatation due to Prader-Willi syndrome, bulimic episodes in anorexia nervosa, and psychogenic polyphagia [1]. Binge eating leading to AGD, stomach necrosis and perforation without any preexisting eating or psychological disorder is an exceptional occurrence with only few cases in literature.
Stomach is very resistant to ischemia due to its abundant blood supply and rich vascular collaterals. Both arterial and venous circulation of the stomach must be interrupted before ischemia and necrosis can occur [2]. When intragastric pressure from gastric distention exceeds 30cm water, intramural blood flow is impaired, resulting in ischemia and necrosis of stomach wall [3]. In pathological eating disorders such as psychogenic polyphagia and bulimia, gastric volumes as high as 15 litres have been recorded [4].
Many theories have been postulated for the pathogenesis of AGD although the exact pathogenesis is unclear. Anaesthesia and debilitation can cause relaxation of the upper oesophageal sphincter with aerophagia leading to gastric distension [5]. AGD may also be a functional entity secondary to regional diseases such as pancreatitis, peptic ulcer, gall bladder disease, appendicitis, etc [5]. Atonic theory and mechanical theory, commonly known as superior mesenteric artery syndrome (SMAS) were also proposed [6,7].
In our case, 24 hours starvation induced atony of the stomach which was overtaxed by the rapidly eating of large quantity of food, leading to AGD. The elevated intragastric pressure from gastric distension impaired the intramural blood flow, resulting in ischemia and necrosis of stomach wall. Lunca S et al., described a case of AGD due to binge eating in a 22-year-old normal male [5]. Mishima T et al., reported gastric necrosis and rupture in anterior part of stomach in a 12-year-old boy without any underlying disorders [8]. In the same year, Sung-Ui J et al., reported a case with rupture in the fundus in a 23-year-old-lady [9]. In 2013, Sahoo MR et al., described a case of ischemic necrosis on fundus and lesser curvature in 36-year-old man [10]. There was no underlying disease in all these cases. Our case is the sixth one and second from India till the paper is written in modern English literature.
An accurate history and physical examination is very important in the diagnosis of AGD because delay can lead to ischemic necrosis and rupture. This catastrophic event is more common in females (67%) and usually occurs along the lesser curvature (63%). It is uniformly fatal without operative intervention, while overall mortality is 73% [4]. Emesis is present in more than 90% of cases of AGD [5]. Another sign in the literature is inability to vomit which was present in our case. It has been suggested that this may be due to the occlusion of the GE junction by the distended fundus, which angulates the oesophagus against the right crus of the diaphragm, producing a one way valve [11]. Diffuse abdominal pain and distension is common. Plain X ray abdomen can demonstrate not only free gas in case of rupture but also the distended stomach with a fluid level. CT scan is a very important radiological tool and can clearly demonstrate gastric distension [6]. In present case, plain X-ray abdomen demonstrated pneumoperitoneum and decision for exploratory laparotomy was made straight forward with a preoperative diagnosis of hollow viscus perforation. CT scan is a very useful tool if plain X-ray does not show pneumoperitoneum and there is a strong clinical suspicion of acute gastric dilatation.
Once the diagnosis of AGD is made, urgent nasogastric decompression and appropriate fluid resustication is required. Normal size NG tube may prove to be inefficient. A wide caliber tube can be used [5]. If total decompression is not possible partial decompression may help because it can decrease the intagastric pressure and reduce the risk of necrosis and perforation. It may also allow vomiting as it may free the GE junction obstruction. If conservative management fails or gastric necrosis with or without perforation is suspected, urgent surgical intervention is required [6]. Adequate resection of the gangrenous portion is essential and gastrointestinal continuity is established depending upon resection. Total gastrectomy with oesophagojejunostomy, partial gastrectomy as well as wedge resection all have been described [10].
Conclusion
The clinicians should be aware of this extremely rare entity. High index of suspicion is required in any patient coming to us with abdominal manifestation following binge eating even without prior eating disorder or psychological disease to diagnose this rapidly progressive and fatal condition. Early diagnosis and prompt management is critical for better outcome.
[1]. Turan M, Sen M, Canbay E, Karadayi K, Yildiz E, Gastric necrosis and perforation caused by acute gastric dilatation: Report of a CaseSurg Today 2003 33(4):302-04. [Google Scholar]
[2]. Babkin BP, Armour JA, Webster DR, Restoration of the functional capacity of the stomach when deprived of its arterial blood supplyCan Med Assoc J 1943 48:1-10. [Google Scholar]
[3]. Edlich RF, Borner JW, Kuphal J, Wangensteen OH, Gastric blood flow. Its distribution during gastric distentionAm J Surg 1970 120:35-37. [Google Scholar]
[4]. Kerstein MD, Goldberg B, Panter B, Tilson MD, Spiro H, Gastric infarctionGastroenterology 1974 67(6):1238-39. [Google Scholar]
[5]. Lunca S, Rikkers A, Stanescu A, Acute massive gastric dilatation: severe ischemia and gastric necrosis without perforationRom J Gastroenterol 2005 14(3):279-83. [Google Scholar]
[6]. Abdu RA, Garritano D, Culver O, Acute gastric necrosis in anorexia nervosa and bulimia. Two case reportsArch Surg 1987 122(7):830-32. [Google Scholar]
[7]. Adson DE, Mitchell JE, Trenkner SW, The superior mesenteric artery syndrome and acute gastric dilatation in eating disorders: a case report of two cases and a review of the literatureInt J Eat Disord 1997 21(2):103-14. [Google Scholar]
[8]. Mishima T, Kohara N, Tajima Y, Maeda J, Inoue K, Ohno T, Gastric rupture with necrosis following acute gastric dilatation: report of a caseSurg Today 2012 42(10):997-1000. [Google Scholar]
[9]. Sung-Ui J, Seung-Hyun L, Byung-Kwon A, Sung-Uhn B, Gastric perforation caused by acute massive gastric dilatation: report of a caseJournal of Medical Cases 2012 3(5):286-89. [Google Scholar]
[10]. Sahoo MR, Kumar AT, Jaiswal S, Bhujbal SN, Acute dilatation, Ischemia and Necrosis of stomach without perforationCase Reports in Surgery 2013 2013:984594(4 pages). Available from: http://www.hindawi.com/crim/surgery/2013/984594 [Google Scholar]
[11]. Breslow M, Yates A, Shisslak C, Spontaneous rupture of the stomach: A complication of bulimiaInt J Eat Disord 1986 5(1):137-42. [Google Scholar]