The ovaries are deep seated, paired, pelvic female reproductive organs. Lesion are not easily accessible clinically. An ultrasound guided, transabdominal and transvaginal fine needle aspiration cytology solves the problem. Use of Fine Needle Aspiration Cytology (FNAC) for diagnosis of ovarian lesions used to be limited in past, due to the apprehension of rupture of tumour capsule and peritoneal spread of malignant tumour. With the advent of accurate imaging techniques and monoclonal antibody for immunocytochemistry, image guided FNAC from ovarian lesions are being increasingly used for diagnosis of ovarian lesions. FNAC can reliably distinguish between benign and malignant ovarian lesions. Ultrasound guided cytology could be considered as a very valuable investigation for diagnosing abdominal masses in early stage [1]. Thus, it helps surgeons to plan appropriate treatment for their patients and to avoid more radical surgical interventions in cases where minimal surgery can serve the purpose. This helps in preserving fertility and hormonal profile of such patients [2].
Fine needle aspiration cytology helps in arriving at a primary diagnosis of ovarian cancer in patients who are at poor surgical risk. Recently some cases of advanced ovarian cancers are being managed by neo-adjuvant chaemotherapy before surgical intervention. FNAC helps in reaching an early diagnosis in such cases. It also has a definitive role in evaluating patients with suspected recurrence in a known case of ovarian cancer [3,4].
The aim of the study was to find the diagnostic accuracy of the method of ultrasound guided cytological assessment of ovarian lesion.
Materials and Methods
A prospective observational study was conducted at Nilratan Sircar Medical College, Kolkata, on the female patients having suspected ovarian lesions. Ultrasound guided transabdominal or transvaginal fine needle aspiration was done, whichever was feasible, with 22G disposable lumbar puncture needle in 43 cases after obtaining a written consent over a period of one year in 2013.
The following were the criteria used for inclusion and exclusion of cases.
Inclusion Criteria
Patients with ovarian lesions, having suspicious sonographic picture (septate, solid or solid-cystic, etc).
Patients with ovarian lesion measuring 8 cm or more in size on ultrasonography.
Patients with ovarian lesion which either doesn’t regress or increases in size after 8 weeks of follow-up period.
Exclusion Criteria
Pregnant women with ovarian lesion.
Patients with ovarian lesion who are in medical or surgical emergency.
Patients with bleeding diathesis.
The aspirated material was then centrifuged at 1000 rotations per minute (rpm) in a centrifuge machine. The cell button formed was then made into a smear on a clean glass slide. Otherwise, if the aspirate was scanty the smears were made directly. Two of the smears were air dried for MGG stain; two were wet fixed in 95% ethanol for Pap stain and rest was kept for special stains, if required.
A cytological opinion regarding benign/malignant nature and categorization of the lesion were done. Subsequently, the cytological diagnosis was compared with the final histological diagnosis, taking histology as the gold standard.
Results
Among 43 cases, 42 cases were neoplastic and only one case was non-neoplastic. The ovarian surface epithelial tumours were most commonly detected in the age range of 41-60 years (21/31=67.74%) and for germ cell tumours the commonest age group were 21-40 years. Among the benign surface epithelial tumours 60% (6/10) and among malignant surface epithelial tumours 73.68% (14/19) were found to be in the age range of 41-60 years. Mean age of diagnosis of malignant surface epithelial tumour was 49.63 years.
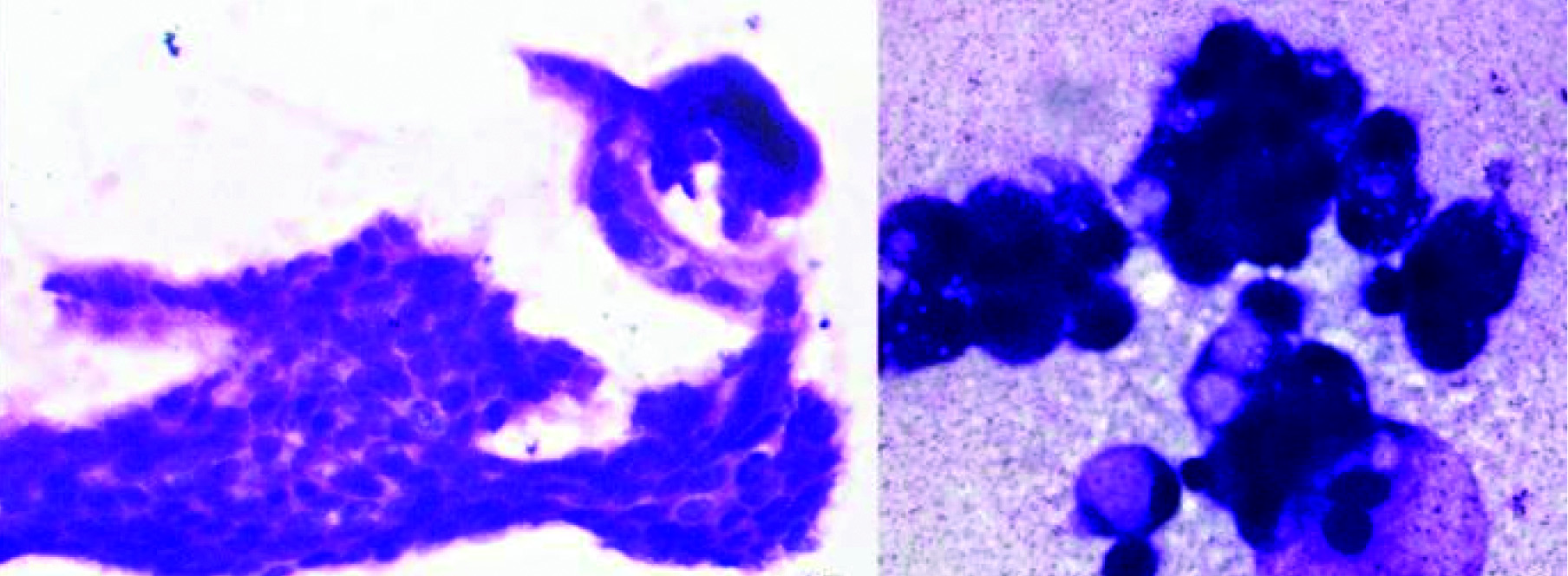
The non neoplastic lesion was diagnosed as chronic ectopic pregnancy on histology, initially reported as a neoplastic lesion on cytology. USG guided FNAC from the apparent right ovarian mass revealed cellular smears with discohesive clusters of moderately pleomorphic cells. The individual cells were of round to oval to polygonal, with large irregular hyperchromatic nuclei and blue-grey cytoplasm. A few papillae, lined by mildly pleomorphic cells with hyperchromatic nuclei were also found. The initial cytological diagnosis of serous cystadenocarcinoma of right ovary was offered [Table/Fig-1]. The patient underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy and infra-colic omentectomy. On subsequent histopathological examination of the right adnexal mass revealed chronic ectopic pregnancy, that resulted from degeneration of products of conception and repeated haemorrhage in the fallopian tube, forming a pelvic mass, mimicking a neoplastic lesion on imaging. The atypical cells found on FNAC were possibly trophoblastic cells aspirated from the chorionic villi. These cells can mimic malignant cells on cytological smear as in cervico-vaginal smear [5]. The papillae found on the smear were probably representing reactive tubal epithelial lining. In this case, atypical clinical presentation, bilaterality, confusing radiological information (right sided tubo-ovarian mass described as ovarian mass on USG), high CA 125 level, combined with the cytological atypia led to a false positive cytological diagnosis.
Chronic ectopic pregnancy: (A) Cytology smear from ovarian mass showing hyperchromatic cells in papillary configuration (MGG x400); (B) Clusters of atypical cells with hyperchromatic irregular nuclei in cytology smears, misinterpreted as serous adenocarcinoma (MGG x1000).

In our study, 5 cases (5/43) were inconclusive due to poor cellularity. These smears were either acellular or contained only cyst macrophages, degenerated cells and inflammatory cells. These cases were included in the study because they satisfied the inclusion criteria of being a suspicious ovarian lesion on imaging. Out of the 42 neoplastic cases, 3 were serous cystadenoma, 1 was mucinous cystadenoma and 1 was serous adenocarcinoma; all were unilocular cystic lesions.
The overall result has been summarized with the cytological and histological concordance [Table/Fig-2]. In our study, cytological typing and subtyping concordance for benign surface epithelial tumour was 50%. Serous cystadenoma showed more inadequate smears (3/6= 50%) than mucinous cystadenoma (1/4=25%). Out of 4 mature cystic teratomas, 3 cases showed concordant cytological diagnoses. One case of mature cystic teratoma was cytologically diagnosed as mucinous cystadenoma due to presence of numerous columnar mucin secreting cells with abundant vacuolar cytoplasm and bland eccentric nuclei.
Concordance between cytological and histological diagnosis.
| Histological Diagnosis | Cytological Diagnosis | Inconclusive Cytology | Concordant Cytological typing | Concordant Cytological Subtyping |
|---|
| Serous Cystadenoma (6) | Serous Cystadenoma (2) | 3 | 3/6 | 3/6 |
| Mucinous Cystadenoma (4) | Mucinous Cystadenoma (3) | 1 | 3/4 | 3/4 |
| Mature Teratoma (4) | Mature Teratoma (3), Mucinous Cystadenoma (1) | 0 | 4/4 | 3/4 |
| Fibroma (1) | Fibroma (1) | | 1/1 | 1/1 |
| Border Line Serous (1) | Serous Adenocarcinoma (1) | | 0/1 | 0/1 |
| Borderline Mucinous (1) | Mucinous Adenocarcinoma (1) | | 0/1 | 0/1 |
| Serous Adenocarcinoma (12) | Serous Adenocar Cinoma (11) | 1 | 11/12 | 11/12 |
| Mucinous Adenocarcinoma (1) | Mucinous Adenocarcinoma (1) | | 1/1 | 1/1 |
| Endometrioid Adenocarcinoma (5) | Endometrioid Adenocarcinoma (3), Serous Adenocarcinoma (2) | | 5/5 | 3/5 |
| Clear Cell Carcinoma (1) | Clear Cell Carcinoma (1) | | 1/1 | 1/1 |
| Dysgerminoma (2) | Dysgerminoma (2) | | 2/2 | 2/2 |
| Yolk Sac Tumour (2) | Yolk Sac Tumour (2) | | 2/2 | 2/2 |
| Metastatic (2) | Metastatic (2) | | 2/2 | 2/2 |
| Chronic Ectopic Pregnancy (1) | Serous Adenocarcinoma (1) | | 0/1 | 0/1 |
Borderline epithelial serous and mucinous tumours couldn’t be diagnosed accurately by cytology. The cases were overcalled as malignant due to increased cellularity and greater degree of atypia evident on cytology smears. We had only one case of fibroma, which was correctly diagnosed benign spindle cell lesion on cytology. Though in almost all cases we were able to do correct cytological typing for malignant surface epithelial tumour, accurate subtyping was not possible for all cases. Concordant subtyping for malignant epithelial tumour was achieved in 84.21% cases. Subtyping was accurate in serous adenocarcinoma [Table/Fig-3a], mucinous adenocarcinoma and clear cell carcinoma, but only 3 out of 5 endometrioid carcinomas were entitled to correct subtype by cytological examination. Two cases of endometrioid carcinoma were diagnosed as serous adenocarcinoma by cytology.
(A) Serous cystadenocarcinoma. Cytology smear showing clusters of hyperchromatic, pleomorphic cells with round to oval to irregular nuclei (MGG x400). (B). Endometrioid adenocarcinoma. Cytology smear showing small clusters and isolated columnar to elongated cells with slightly eccentric oval nuclei with irregular nuclear membrane and squamoid morule (MGG x400). (C) Dysgerminoma. Cytology smear showing poorly cohesive cells with large nuclei and macronucleoli with sprinkling of lymphocytes (MGG x1000).

We got some interesting cytological features in three cases of endometrioid carcinoma. They showed mainly discohesive cells instead of syncytial clusters or papillae. Individual tumour cells were columnar to elongated, with slightly eccentric vesicular oval nuclei, irregular nuclear membrane along with squamoid morules evident in the photomicrograph as having ample amount of eosinophilic cytoplasm and round nuclei with coarse chromatin, towards central from 3’ o clock position [Table/Fig-3b]. In present study subtyping of malignant germ cell tumours were done accurately (100% concordance) by FNAC. Two cases of dysgerminoma [Table/Fig-3c] and two cases of yolk sac tumour were correctly identified.
Our study group included 18 cystic ovarian lesions (10 unilocular cysts and 8 multilocular cysts). In 6 cases cytology were inconclusive and one case was discordant (borderline mucinous tumour was cytologically diagnosed as mucinous adenocarcinoma) [Table/Fig-4a,b]. Therefore, concordance for cystic ovarian lesion was 61.11% (11/18). Concordance for solid ovarian lesions was 100% (8/8). Among 17 solid-cystic ovarian lesion two were discordant (one borderline serous tumour and one chronic ectopic pregnancy were cytologically diagnosed as serous adenocarcinoma) Therefore, concordance for solid-cystic ovarian lesions was 88.24% (15/17). The overall sensitivity, specificity, and accuracy of the method as calculated from true positive, true negative, false positive and false negative cases, were high at 96%, 76.92% and 89.47% respectively [Table/Fig-5].
(A) Borderline Mucinous Tumour. Cytology smear showing cohesive sheet of vauolated cytoplasm appreciated in the periphery, round to oval mildly pleomorphic nuclei with moderate overlapping (MGG x400). (B) Mucinous Carcinoma. Cytology smear showing round to oval moderate to highly pleomorphic cells with eccentric hyperchromatic nuclei and vacuolated cytoplasm (MGG x1000).
Statistical Calculations.
| Test | Disease Positive (Malignant on Histology) | Disease Negative (Non Malignant on Histology) |
|---|
| Test Positive (Cytologically Malignant) | 24 (True Positive) | 3 (False Positive) |
| Test Negative (Cytologically Benign/Inconclusive) | 1 (False Negative) | 10 (True Negative) |
In our study, we identified 2 metastatic ovarian tumours (100% concordance) by observing specific cytological features. One case showed moderately cellular smear with small cluster and isolated signet ring cells and the diagnosis of krukenberg tumour was given. In this case tumour was bilateral, solid on ultrasonography and serum CA 125 was mildly elevated (42.4 U/ml). Further workup showed this tumour metastasized from stomach, though cytologically it was not possible to predict the primary site.
Other metastatic tumour in our series was endometrial stromal sarcoma which was a 6 cm unilateral solid-cystic ovarian mass presented with abdominal pain and mildly elevated (37.1 U/ml) CA 125 level. FNAC smears showed cells in clusters with individual cells closely resembled clusters of round to oval cells resembling endometrial stromal cells and cyst macrophages. Histological examination of uterus identified the primary tumour in the uterine corpus without any foci of endometriosis in involved ovary and a simple cyst.
Discussion
The overall sensitivity, specificity, and accuracy of the present study were high at 96%, 76.92% and 89.47% respectively. The accuracy of cytological diagnosis was greater for frank malignant lesions and for solid-cystic lesions compared to benign and pure cystic ones owing to paucicellularity and sampling errors.
The strength of the present study lies in the ease of the method used and the rapidity of the results obtained thereof, comparable to the frozen section results, where such facilities are unavailable. It can provide a rapid data regarding the neoplastic and non-neoplastic typing as well as the benign and malignant nature of the lesions and proper categorization.
The major limitation has been the borderline tumours where a wide base data regarding the variability of cytological picture of the lesions are missing, thereby giving rise to interpersonal variation and difference in opinion.
Out of 43 cases, no opinion was possible in only 6 cases (13.9%) due to paucity of cells in the smears. The rate of inadequate smears in the present study is comparable with Papathanasiou K et al., and Sood T et al., having inadequate result in 20% and 7% cases respectively [6,7]. Inadequate samples were obtained by both benign and malignant cysts in our study and this fact corresponded with the observation of Pilar Martínez-Onsurbe et al., [8]. Most of the acellular smears in our study were from benign tumours, the same observation that made by Ganjei P et al., [9].
Concordance of cytological typing for malignant surface epithelial tumour was much higher (94.74%) than the overall concordance (79.07%) in present study and this was attributed to the very low number of inconclusive smears in case of malignant surface epithelial tumours (only one unilocular cystic serous adenocarcinoma produced inconclusive result). The accuracy of diagnosing germ cell tumours was similar to Akhtar M et al., [10].
The overall sensitivity, specificity, and accuracy of the present study was high at 96%, 76.92% and 89.47% respectively, which corroborated the cytological findings of Soumit Dey et al., in peroperative imprint cytology of ovarian lesions with a sensitivity of 96.2%, specificity of 75%, positive predictive value of 96.3%, and diagnostic accuracy of 83.3% [11]. The sensitivity, specificity and diagnostic accuracy of intraoperative frozen section, as in the study of Takemoto S et al., was 80%, 99.6% and 80% respectively, with slightly better specificity than the present work [12].
In the current study two borderline epithelial tumours were diagnosed as malignant epithelial tumour (false positive) due to high cellularity of the smears and cytological atypia. This observation is similar to Ganjei P et al., [9]. In a study to evaluate the diagnostic accuracy of intraoperative frozen section in borderline ovarian tumours, done by Basaran D and colleagues [13], found concordance of frozen section with histology in 37 out of 59 cases, with a significant risk of underdiagnosis as opposed to overcalling borderline tumours as malignant in our study using cytology, with increased cellularity and atypia. Hence, the grey zone of borderline lesion could not be done away with either of the methods of cytology or frozen section. It stresses the long tested extensive sampling and examination of histopathological sections from paraffin embedded formalin fixed tissue as the gold standard in such borderline cases.
Conclusion
Thus, to conclude it would not be an exaggeration to say that preoperative ultrasound guided cytology is a rapid, useful and a very effective diagnostic modality. The inconclusive and false negative cases are mainly due to poor cell yield and limited sampling.
The number of false positive cases can be reduced by conducting a large scale study to set up a standard cytological morphological data for proper categorization of lesions similar to that already used in histology, and reduce personal variations, more importantly, in the gray zone areas of borderline ovarian tumours. Such data can be generated if we can perform aspiration cytology peroperatively and secondarily in addition to the frozen section where it is used on a routine basis.