Dirofilariasis is a zoonotic disease caused commonly by Dirofilaria repens and Dirofilaria immitus. The definitive hosts are domestic dogs and cats. Human beings are accidental dead end hosts, and acquire infestation through mosquito bites. So far, very few cases have been reported from western India.
We report a case of a 27-year-old male who presented with preseptal cellulitis right eye and a firm mass in the lower lid. Histopathological examination after surgical excision of the mass revealed a diagnosis of dirofilariasis. Although rare in Western India a diagnosis of dirofilariasis should be considered in cases of preseptal cellulitis associated with a periorbital mass.
Case Report
A 27-year-old male reported to the outpatient department with complaints of painful swelling of the right lower lid and cheek of 2 days duration. Ophthalmic examination of the right eye revealed inflammation involving the lower lid and cheek. Ocular movements were normal. There was no proptosis. Distant visual acuity was 6/6 in both eyes. Anterior and posterior segments and the intra ocular presssure were normal in both the eyes.
A diagnosis of preseptal orbital cellulitis right eye was made and treatment with Capsule Doxycycline 100mg twice daily, Tab Ibuprufen 400mg and Paracetamol 325mg twice daily was instituted for 5 days. Subsequent to the resolution of cellulitis, a firm, non tender, discrete oval swelling measuring 2x1cm could be palpated in the medial half of the right lower lid. The mass was mobile and not adherent to the overlying skin [Table/Fig-1].
Preoperative appearance of the patient, showing a swelling in the Right lower lid

General and Systemic examination was within normal limits. No other subcutaneous lesions were found. Routine haematological investigations, including complete haemogram, ESR and blood sugar levels were within normal limits.
In view of the firm, nontender, mobile mass in the lower lid a differential diagnosis of dermoid cyst and cysticercosis was entertained. MRI Brain and orbits was advised to exclude neurocysticercosis and to determine the dimensions of the lesion and its intra orbital extension prior to planning any surgical intervention.
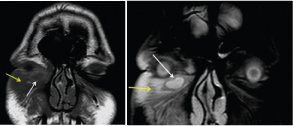
MRI Brain was reported as within normal limits. MRI Orbits (T1weighted images, T1 post contrast images and STIR images) showed a well defined, elliptical, hypointense lesion in the right lower eyelid measuring 14.6 x 6.5mm with a relatively hyperintense margin. The surrounding soft tissue showed evidence of subcutaneous oedema and cellulitis [Table/Fig-2a&b]. No calcification was seen in the cyst. There was no intraorbital extension and the globe was normal.
(a) T1 weighted coronal MRI image of orbits showing a well defined, elliptical, hypointense lesion with hyperintense margins in the Right lower lid (White Arrow). Surrounding soft tissue appears hypointense suggestive of subcutaneous oedema (Yellow Arrow) (b) STIR coronal image showing corresponding hyperintense signal within the lesion with a hypointense periphery (White arrow). No focal hypointensity within the lesion to suggest calcification. Subcutaneous oedema (yellow arrow)
Surgical exploration was performed, which revealed a well encapsulated, firm mass, measuring 2.5 x 1.5x 1 cm, lying beneath the orbicularis oculiand anterior to the orbital septum It was excised in toto and subjected to histopathological examination [Table/Fig-3,4].
Intraoperative appearance of cyst


Histopathology reported a single, elongated, grey white tissue bit measuring- 2.5 x 1.5 x 1cm. On cut section homogenous white necrotic areas were seen.
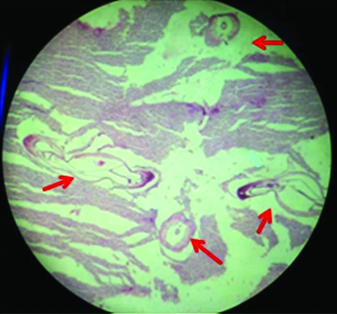
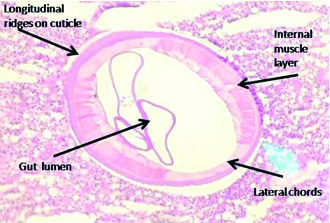
Microscopic examination of the sections studied from the swelling over the eyelid showed a thick walled cyst. The cyst showed a well circumscribed lesion composed of dense mixed inflammatory exudate with infiltration by histiocytes, mononuclear cells, and eosinophils. The lumen showed multiple cross sections of a parasite having outer thick multilayered cuticle with longitudinal ridges, internal muscle layer with lateral chords, and a gastrointestinal tract, suggestive of Dirofilaria repens [Table/Fig-5,6].
Histopathological image (H&E Stain, X 50 magnification) showing a well circumscribed lesion with infiltration by histiocytes, mononuclear cells and eosinophils. Multiple cross sections of the parasite seen
High power view (100X) showing thick, multilayered cuticle with longitudonal ridges, internal muscle layer with lateral chords and the gastrointestinal tract of the parasite
Postoperative recovery was uneventful [Table/Fig-7]. Monthly follow up over a period of 6 months showed no recurrence of the mass or any subcutaneous nodule.
Appearance on 4th Postoperative day

Discussion
Dirofilariasis is a zoonotic disease caused commonly by Dirofilaria repens and Dirofilaria immitus. The definitive hosts are domestic dogs and cats. Other hosts include wolves, coyotes, foxes, muskrats, and sea lions etc. The Aedes, Anopheles and Culex mosquitoes act as intermediate hosts and vectors [1]. Human beings are accidental dead end hosts, and acquire infestation through mosquito bites.
The prevalence of human dirofilariasis is very high in Italy and Srilanka [1]. Cases have also been reported from United States, Canada, Japan, and Australia [1]. Reports have also been published from the Indian states of Kerala [2], Karnataka [3] and Tamil Nadu [4]. So far, very few cases have been reported from western India.
The epidemiology of human Dirofilariasis directly correlates to the prevalence of canine infestation. In India, most cases have been reported from Kerala and Karnataka; few cases have also been noted in Assam [5] and Orissa [6]. A study done to assess the prevalence of canine infestation in Leh, Mumbai, Sikkim and Delhi revealed a prevalence of 8% to 16.7% in Mumbai [7]. However, reports of human dirofilariasis with ocular symptoms are relatively rare, with only four cases reported so far from Maharashtra [8–10]. This is the fifth case of ocular human dirofilaria from Maharashtra.
Canines are the definitive hosts in the life cycle of Dirofilaria and are infected with the 3rd stage filarial larva following a bite from an infected mosquito. The adult worm is present in the subcutaneous tissues of the dog and may live for 5 to 10 years. The microfilarae are found in the peripheral blood of canines. Humans are infected accidentally and are poor hosts. The worm generally dies before reaching sexual maturity and does not release viable microfilarae. Only one report of circulating microfilarea in a human exists in medical literature [1].
Human Dirofilariasis usually manifests as subcutaneous nodules or lung disease which may often be asymptomatic. D immitus is responsible for human pulmonary disease, where as D repens infestation usually presents as subcutaneous lumps, which maybe painful. The common sites of the lesions are face and eyelids, chestwall, upper arms, thighs, abdominal wall and male genitalia [1]. Ophthalmic involvement may be periorbital [2], subconjunctival [8], subtenons or intraocular [11]. Most frequent ocular involvement has been seen in the periocular tissues. Of the four cases reported from Maharashtra, three had a cystic mass in the lids and one patient had a subconjunctival nodule [8–10]. All cases were managed successfully with excision. The diagnosis in these cases was established after histopthological examination of the excised mass.
Our case presented as preseptal cellulitis involving the lower lid and cheek. A subcutaneous mass in the lower lid was detected on subsidence of inflammation. In reported cases of periorbital inflammation along with cystic lesions in the lids, differential diagnoses of orbital abscess, inflammatory pseudotumour, sebaceous cyst and metastases have also been considered [12]. These were excluded in our patient by MRI studies and furthermore there was complete resolution of inflammation with treatment.
Though orbital dirofilariasis is a known manifestation, the diagnosis is usually made after surgical excision. However, it is now being reported that high resolution ultrasonography of the lesion may detect a live worm [13]. CT-scan orbits may show the cyst as a well defined, peripherally enhancing lesion. MRI orbits reveal a hyper intense signal on Short-Tau Inversion Recovery image (STIR) and rim enhancement on post contrast T1 weighted images [2]. MRI findings in our case also showed a similar picture, however the presence of the worm was not reported. High resolution ultra sonography if performed might have suggested the diagnosis preoperatively. Eosinophilia may be detected in up to 20% of cases of Human Pulmonary Dirofilariasis (HPD), however eosinophilia and elevated serum immunoglobulin E levels are rarely observed and are of limited value in screening for dirofilariasis [1].
Treatment of subcutaneous dirofilarial nodule consists of complete excision. Ivermectin or Diethylcarbamazine may be advised for deeper multiple lesions [1]. Preoperative Ivermectinor Dec may be considered if the diagnosis is suspected prior to surgery. However, most cases are diagnosed after histopathological examination of the excised tissue. Our case showed complete recovery after excision of the cyst. No recurrences were detected during a six month follow up.
Conclusion
Human Dirofilariasis, a newer emerging zoonosis, is now being reported more often from various parts of the world as well as India. Though uncommon, this case highlights the importance of Dirofilaria being considered as a differential diagnosis in cases of periocular or orbital inflammation. A high index of suspicion should be maintained in cases of orbital cysts and high resolution ultrasonography may be useful in confirming the diagnosis prior to surgical excision.
[1]. Alena Klochko, MD; Chief Editor: Burke A Cunha, MD dirofiariasis Updated: Jul 22, 2013. Available at emedicine.medscape.com/article/236698 [Google Scholar]
[2]. Gopinath TN, Lakshmi K P, Shaji PC, Rajalakshmi PC, Periorbital dirofilariasis-Clinical and imaging findings: Live worm on ultrasoundIndian J Ophthalmol 2013 61:298-300. [Google Scholar]
[3]. Bhat KS, Kotigadde S, VishwanathaBhat KN, Pare P, Subconjunctival dirofilariasis: Case studies with review of literatureTrop Parasitol 2014 4:119-21. [Google Scholar]
[4]. Sathyan P, Manikandan P, Bhaskar M, Padma S, Singh G, Appalaraju B, Subtenon’s infection by Dirofilaria repensIndian J Med Microbiol 2006 24(1):61-62. [Google Scholar]
[5]. Nath R, Gogoi R, Bordoloi N, Gogoi T, Ocular dirofilariasisIndian J Pathol Microbiol 2010 53:157-59. [Google Scholar]
[6]. Singh R, Shwetha JV, Samantaray JC, Bando G, Dirofilariasis: A rare case reportIndian Journal of Medical Microbiology 2010 28(1):75-77. [Google Scholar]
[7]. Megat Abd, Rani PA, Irwin PJ, Gatne M, Coleman GT, McInnes LM, Traub RJ, A survey of canine filarial diseases of veterinary and public health significance in IndiaParasit Vectors 2010 3:30 [Google Scholar]
[8]. Sangit VA, Haldipurkar SS, Subconjunctival dirofilariasis mimicking scleritis: First report from Western IndiaIndian J Ophthalmol 2012 60:76-77. [Google Scholar]
[9]. Khurana S, Singh G, Bhatti H S, Malla N, Human subcutaneous dirofilariasis in India: A report of three cases with brief review of literatureIndian J Med Microbiol 2010 28:394-96. [Google Scholar]
[10]. Sahdev SI, Sureka SP, Sathe PA, Agashe R, Ocular dirofilariasis: Still in the dark in western India?J Postgrad Med 2012 58:227-28. [Google Scholar]
[11]. Das D, Das K, Islam S, Bhattacharjee K, Bhattacharjee H, Das SM, A rare case of anterior chamber dirofilariasisOman J Ophthalmol 2015 8(1):50-53. [Google Scholar]
[12]. Mannino G, Teresa Contestabile M, Medori EM, Dirofilaria repens in the eyelid: Case report of subcutaneous manifestationEur J Ophthalmol 2009 19:475-77. [Google Scholar]
[13]. Smitha M, Rajendran VR, Devarajan E, Anitha PM, Case report: Orbital dirofilariasisIndian J Radiol Imaging 2008 18(1):60-62. [Google Scholar]