Chronic pancreatitis (CP) is a progressive inflammatory disease of the pancreas characterized by debilitating pain and pancreatic exocrine and endocrine insufficiency [1]. Chronic alcohol abuse is the most common cause of chronic pancreatitis in western countries, accounting for about 60% CPs [2]. The incidence of CP is approximately 5-10 cases per 100,000 populations and has nearly quadrupled in the past 30 years, although this may be due to improvement in imaging technology rather than a true increase in occurrence [3,4]. India has the highest incidence of chronic pancreatitis in the world at approximately 114-200 cases per 100,000 persons [2]. But in India, tropical pancreatitis is the most frequently seen etiology of chronic pancreatitis. It is often classified as idiopathic but in fact it may have a mixed etiology, including metabolic, nutritional and genetic [3]. Approximately 90% of patients with CP complain of pain which requires multiple hospitalizations and that can lead to narcotic dependency [5]. The poor understanding of the disease pathology and unpredictable clinical course of the disease has made the management of patients suffering, difficult and challenging. Many studies have shown that CP has a substantial impact on quality of life because of chronic pain, and complications, including exocrine and endocrine insufficiency [6–8].
Previous studies have shown that 40% to 75% of patients with CP ultimately requires surgical intervention despite of medical and endoscopic intervention [9,10]. It is primarily used as the last step of the step up approach. But recent studies have showed benefits of early surgery on control of pain and preservation of exocrine and endocrine insufficiency before the disease progress into an irreversible stage. The main indication for surgery is intractable abdominal pain not relieved with medication, development of jaundice due to peri-choledochal inflammation and suspicion of malignancy [3,11]. Varied morphology of the gland, presence of inflammation in the pancreas and peri-pancreatic tissue, disease location, prior treatment and suspicion of malignancy has led to evolution of diverse resection and drainage procedures. 18-50% of patients with CP have disease limited to the head of the pancreas and resection is necessary for pain relief [12]. Pancreaticoduodenectomy may provide good pain relief, but there has been increasing enthusiasm for duodenum preserving pancreatic head resection along with ductal drainage procedures [13]. Two such procedures have gained importance; they are Beger’s procedure and Frey’s procedure [14]. Frey’s procedure is more popular among pancreatic surgeons as it avoids pancreatic neck resection and requires single anastomosis [15]. This novel technique was first described by Frey and Smith in 1987 which consist of local pancreatic head resection combined with longitudinal pancreatico-jejunostomy (LR-LPJ) [16].
CP is an incurable disease; the main purpose of any therapeutic intervention in CP is to make the patient pain free and improve the quality of life [17]. Several studies have shown that Frey’s procedure is an effective way for management of patients with intractable abdominal pain due to CP, which is associated with minimal morbidity and mortality and have a better quality of life after the procedure [18–23].
In this study, we have intended to further validate the above theory and see whether Frey’s procedure is effective in Indian patients. The primary aim of this study was to observe and analyze the outcomes of Frey’s procedure on quality of life in patients with chronic pancreatitis. This study also deals with the clinical presentation, duration of surgery, particularly in relation to the diameter of pancreatic duct and peri-operative morbidity and mortality.
Materials and Methods
This was a prospective observational study done in Institute of Post Graduate Medical Education and Research, Kolkata, India, between 2010 and 2014. Ethical clearance was taken from the institutional review board for this study. Informed and written consent were taken from all patients. All proven cases of CP with age above 12 years having a main pancreatic duct diameter of ≥6.5mm with or without duct calculi and complaining of pain not controlled on medications were included in the study. Those patients with gross cardiovascular morbidity, splenomegaly and pancreatic malignancy in the postoperative histopathology were excluded from the study.
Demographic data were collected from all patients at the time of admission, including age sex, and BMI, history of alcohol intake, clinical presentation and main pancreatic duct diameter (MPD). Visual analogue scale (0-100) was used to assess the preoperative and postoperative pain [24]. Preoperative physical quality of life was assessed using European Organization for Research and Treatment of cancer (EORTC) QLQ-C30 (version 3) questionnaire (Appendix 1). This questionnaire was developed by the EORTC study group to use this as an instrument for quality of life assessment in cancer patients. It consists of 30 questions related to health related quality of life. In our study we have classified all the 30 questions into five domain i.e. Physical Function Domain (PFD), Physical Domain (PD), Emotional Domain (ED), Social Domain (SD) and Global Health (GH) to make the analysis and interpretation easy and simple (Appendix 2).
Total score of VAS and each domain was calculated in the preoperative period before surgery. Frey’s procedure was performed (coring of pancreatic head and longitudinal pancreaticojejunostomy) in all patients and tissues from the pancreatic head were sent for histopathological examination. Patients with evidence of malignancy on histopathology were excluded from the study. Postsurgery, patients were followed up after three months, then every six monthly for a period of three years. During each follow up patients were interviewed and physical quality of life was assessed using the same EORTC QLQ-C30(3) questionnaire [25] and VAS score. As we were using the raw scores for the comparison, a high score in the PFD, ED, SD and PD represents a low level of functioning or low level of symptomatology, while a low score in these domains represents a high level of functioning or high level of symptomatology. But a high score in global health domain (GH) represents a high quality of life (Qol) and a low score represents a low Qol.
Statistical Analysis
Statistical Analysis was performed with help of Epi Info (TM) 3.5.3. EPI INFO is a trademark of the Centers for Disease Control and Prevention (CDC). Descriptive statistical analysis was performed to calculate the means with corresponding standard errors (s.e) and the medians. Pearson correlation coefficient was used to assess the correlation between main pancreatic duct diameter and operative time. Analysis of variance (ANOVA) followed by Tukey’s Test was performed with the help of Critical Difference (CD) or Least Significant Difference (LSD) at 5% and 1% level of significance to compare the mean values. The p-value <0.05 was taken to be statistically significant.
Results
A total of 35 patients with features of CP underwent Frey’s procedure during the study period. Two patients with features of malignancy in the postoperative histopathology were excluded from the study. A total of 33 patients with features of CP in the postoperative histopathology were included in the study. Mean age of presentation was 38.48±5.55 years (29-49 years) and the median age was 38 years. Most of the patients were in the age group of 35-44 years (51.5%) compared to other age groups. Incidence among males (81.8%) was significantly higher than females. In our study non alcoholic patients (69.7%) were more commonly affected than alcoholic patients. Most of the patients were thin build with a BMI of < 19 kg/m2 (60.6%). The clinical and socio-demographic characteristics of the patients are shown in [Table/Fig-1].
Patients characteristics.
| Number | Percentage (%) |
|---|
| Age (In years) |
| 25-34 | 10 | 30.3 |
| 35-44 | 17 | 51.5 |
| 45 and above | 6 | 18.2 |
| Gender | | |
| Male | 27 | 81.8 |
| Female | 6 | 18.2 |
| Cause |
| Alcoholic | 10 | 30.3 |
| Non Alcoholic | 23 | 69.7 |
| Preoperative BMI (kg/m2) |
| 16.1-19 | 20 | 60.6 |
| 19.1-22 | 9 | 27.3 |
| 22.1-25 | 4 | 12.1 |
| >25 | 0 | 0 |
| Complains at Presentation |
| Pain | 33 | 100 |
| Diabetes | 5 | 15.1 |
| Diarrhea (Steatorrhea) | 8 | 24.2 |
| Postoperative complications |
| Wound infections | 2 | 6.0 |
| Abdominal abscess | 1 | 3.0 |
| Pancreatic leak | 1 | 3.0 |
| Total | 4 | 12.1 |
BMI: Body Mass Index
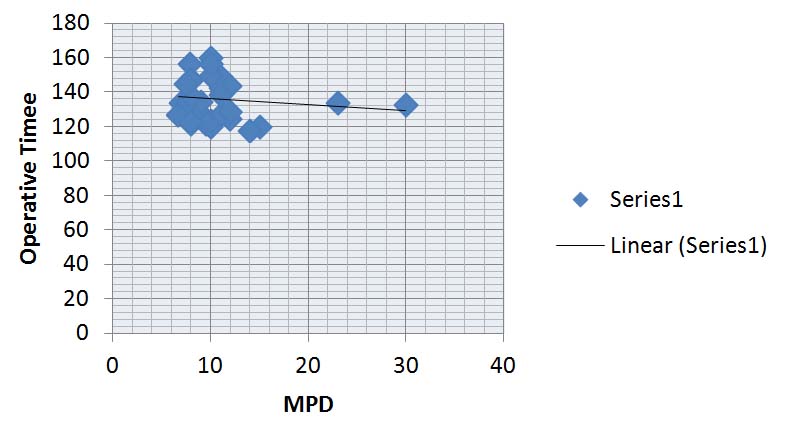
The mean MPD of the patients were 10.73±4.60mm with the range of 6.7-30mm and the median MPD diameter was 10mm. Mean operative time was 136±12 minutes (118-160) where as the median operative time was 133.5 minutes. The pearson correlation coefficient between Operative time and MPD was 0.043 (p<0.05) which suggest that the patients with thinner MPD had longer operative time [Table/Fig-2].
Illustrating the relation of MPD with Operative time.
Out of the 33 patients 48.5% of patient needed intraoperative blood transfusion (median 1 unit). All the patients were kept in intensive care unit in the early postoperative period. 4 out of 33 patients (12.1%) had surgical complications mainly wound infection (2), pancreatic leak (1) and abdominal abscess (1). No patient had undergone reoperation for the complications. In our study, thirty day mortality rate was zero.
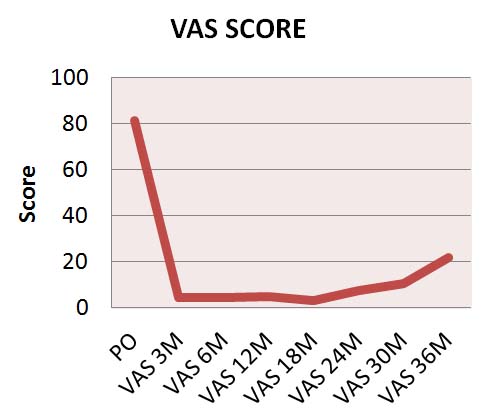
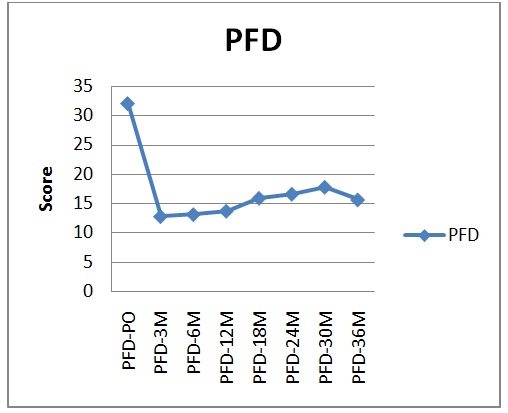
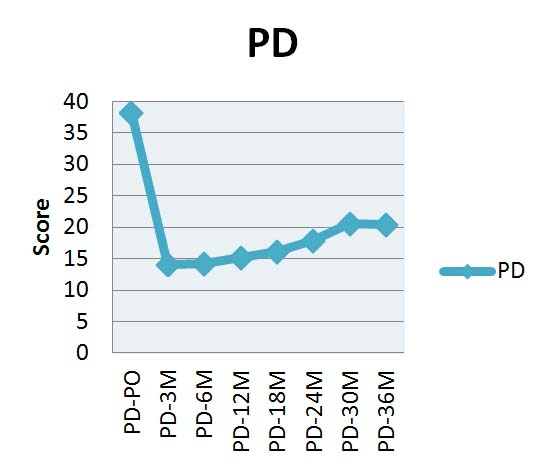
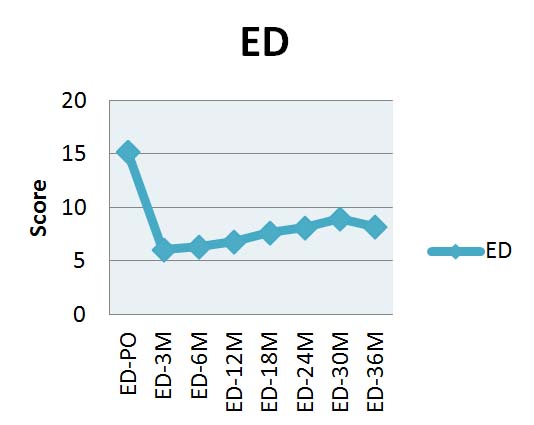
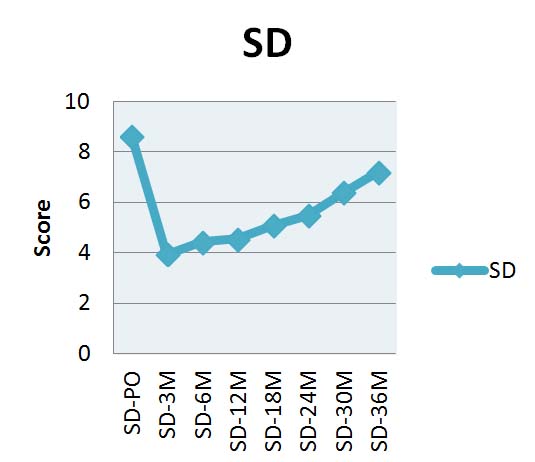
The mean scores (with standard error) of VAS and different domains in the preoperative period and during postoperative follow up at 3, 6, 12, 18, 24, 30 and 36 months as calculated by EORTC QLQ-C30(3) questionnaire is given in the [Table/Fig-3]. Mean VAS scores at different time periods were 81.5, 4.54, 4.54 5.15, 3.21, 7.81, 10.76, and 22.0 [Table/Fig-4]. For PFD the mean values were 32.06, 12.76, 13.09, 15.87,16.57, 17.76, and 15.60. For PD the mean values were 37.85, 14.09, 14.21, 15.15, 16.09, 17.95, 20.54, and 20.40. For ED the mean values were 15.18, 6.06, 6.36, 6.81, 7.65, 8.15, 9.00, and 8.20. For SD the mean values were 8.63, 3.93, 4.42, 4.54, 5.09, 5.47, 6.38, and 7.20. For GH the mean values were 4.48, 12.54, 12.57, 12.03, 11.65, 10.78, 10.00, and 10.20 [Table/Fig-5a,b,c,d and e].
Tabulation of the mean preoperative and postoperative follow up VAS score, Physical functional domain (PFD) score, Physical domain (PD) score, Emotional domain (ED) score, Social domain (SD) score and Global health (GH) score of the patients.
| Time | VAS (mean ±s.e.) | PFD (mean ±s.e.) | PD (mean ±s.e) | ED (mean ±s.e) | SD (mean ±s.e) | GH (mean ±s.e) |
|---|
| Preoperative | 81.51±10.0 | 32.06±0.40 | 37.85±0.36 | 15.18±0.32 | 8.63±0.31 | 4.48±0.26 |
| 3 months(n=33) | 4.54±6.6 | 12.76±0.49 | 14.09±0.36 | 6.06±0.24 | 3.93±0.18 | 12.54±0.32 |
| 6 months(n=33) | 4.54±6.5 | 13.09±0.52 | 14.21±0.52 | 6.36±0.27 | 4.42±0.25 | 12.57±0.30 |
| 12 months(n=33) | 5.15±6.5 | 13.67±0.63 | 15.15±0.59 | 6.81±0.42 | 4.54±0.27 | 12.03±0.33 |
| 18 months(n=32) | 3.21±5.8 | 15.87±0.75 | 16.09±0.81 | 7.65±0.50 | 5.09±0.30 | 11.65±0.35 |
| 24 months (n=19) | 7.81±10.8 | 16.57±1.08 | 17.95±1.15 | 8.15±0.69 | 5.47±0.41 | 10.78±0.54 |
| 30 months(n=13) | 10.76±10.3 | 17.76±1.56 | 20.54±1.49 | 9.00±0.91 | 6.38 ±0.52 | 10.00±0.63 |
| 36 months (n=5) | 22.0 ±14.8 | 15.60±2.78 | 20.40±3.65 | 8.20±1.49 | 7.20±1.35 | 10.20±0.80 |
[n= number of patients, s.e.= standard error] VAS: visual analogue scale
Illustrating the mean visual analogue scale scores (VAS) both during the preoperative period and the follow up period. [M: Month].
Illustrating the mean physical functional domain (PFD) scores according to QLQ-C30 (3) both during the preoperative period and the follow up period. [M: Month].
Illustrating the mean physical domain (PD) scores of the patients according to QLQ-C30 (3) both during the preoperative period and the follow up period. [M: Month].
Illustrating the mean emotional domain (ED) scores of the patients according to QLQ-C30 (3) both during the preoperative period and the follow up period. [M: Month].
Illustrating the mean social domain (SD) scores of the patients according to QLQ-C30 (3) both during the preoperative period and the follow up period. [M: Month].
Illustrating the mean global health (GH) scores of the patients according to QLQ- C30 (3) both during the preoperative period and the follow up period. [M: Month].
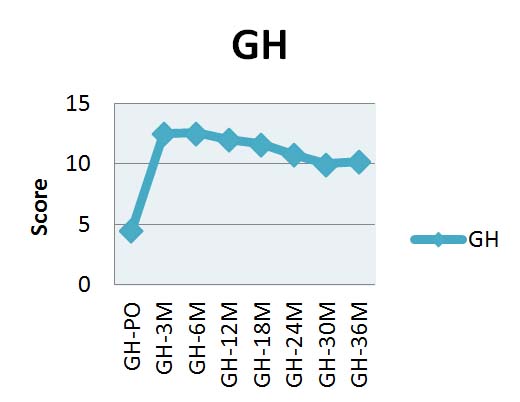
ANOVA showed that there was significant difference in the mean VAS scores (p<0.001), PFD score (p<0.0001), PD score (p<0.001), ED score (p<0.0001), SD score (p<0.001) and GH score (p<0.0001) during different time period as compared to preoperative mean score. As per the Critical Difference the mean scores of PFD, PD, SD and ED decreased significantly in different months compared to preoperative value except for SD during 30th and 36th month at which no significant difference was observed [Table/Fig-5a-d,6]. This is probably due to loss to follow up of the patients during this period (n=13, n=5). However, as per the critical difference the mean score of GH increased significantly in different months compared to preoperative mean score [Table/Fig- 5e,6].
Comparison between preoperative (PO) mean values of different domains of QLQ-C30(3) with their follow up values.
| Comparison between preoperative(PO) mean value of PFD score with the follow-up values | Difference of mean | Significance |
|---|
| PO Vs 3rd Month | 19.3 | p<0.0001 S |
| PO Vs 6th Month | 18.97 | p<0.0001 S |
| PO Vs 12th Month | 18.39 | p<0.0001 S |
| PO Vs 18th Month | 16.19 | p<0.001 S |
| PO Vs 24th Month | 15.49 | p<0.001 S |
| PO Vs 30th Month | 14.3 | p<0.001 S |
| PO Vs 36th Month | 16.46 | p<0.001 S |
| Comparison between preoperative(PO) mean value of PD score with the follow-up values | Difference of mean | Significance |
|---|
| PO Vs 3rd Month | 23.76 | p<0.0001 S |
| PO Vs 6th Month | 23.64 | p<0.0001 S |
| PO Vs 12th Month | 22.7 | p<0.0001 S |
| PO Vs 18th Month | 21.76 | p<0.001 S |
| PO Vs 24th Month | 19.9 | p<0.001 S |
| PO Vs 30th Month | 17.31 | p<0.001 S |
| PO Vs 36th Month | 17.45 | p<0.001 S |
| Comparison between preoperative(PO) mean value of ED score with the follow-up values | Difference of mean | Significance |
|---|
| PO Vs 3rd Month | 9.12 | p<0.001 S |
| PO Vs 6th Month | 8.82 | p<0.001 S |
| PO Vs 12th Month | 8.37 | p<0.001 S |
| PO Vs 18th Month | 7.53 | p<0.001 S |
| PO Vs 24th Month | 7.03 | p<0.01 S |
| PO Vs 30th Month | 6.18 | p<0.01 S |
| PO Vs 36th Month | 6.98 | p<0.01 S |
| Comparison between preoperative(PO) mean value of SD score with the follow-up values | Difference of mean | Significance |
|---|
| PO Vs 3rd Month | 4.7 | p<0.0001 S |
| PO Vs 6th Month | 4.21 | p<0.0001 S |
| PO Vs 12th Month | 4.09 | p<0.0001 S |
| PO Vs 18th Month | 3.54 | p<0.001 S |
| PO Vs 24th Month | 3.16 | p<0.05 S |
| PO Vs 30th Month | 2.25 | p>0.05 NS |
| PO Vs 36th Month | 1.43 | p>0.05 NS |
| Comparison between preoperative(PO) mean value of GH score with the follow-up values | Difference of mean | Significance |
|---|
| PO Vs 3rd Month | 8.06 | p<0.0001 S |
| PO Vs 6th Month | 8.09 | p<0.0001 S |
| PO Vs 12th Month | 7.55 | p<0.0001 S |
| PO Vs 18th Month | 7.17 | p<0.001 S |
| PO Vs 24th Month | 6.30 | p<0.001 S |
| PO Vs 30th Month | 5.52 | p<0.01 S |
| PO Vs 36th Month | 5.72 | p<0.01 S |
[S: Significant, NS: Not significant, PO: Preoperative, PFD: Physical function domain, PD: Physical domain, ED: Emotional domain, SD: Social domain, GH: General health]
Discussion
Chronic pancreatitis (CP) is a disease that is mostly seen in chronic alcoholics; however tropical pancreatitis a form of CP is frequently seen in tropical counties like India. We found a different variety of CP (tropical pancreatitis) mostly affecting malnourished younger individuals [5]. Debilitating pain and pancreatic insufficiency (exocrine and endocrine insufficiency) are characteristics of CP [26]. Efforts to relieve this debilitating pain should be individualized based on the size of the duct and the location of the disease. In our study we have seen that the operative time taken for operating patients with larger main pancreatic duct is significantly less when compared with thinner duct patients.
Pancreaticoduodenectomy is the standard procedure for addressing patients of CP with disease limited to the head region. Farkas and colleagues have shown better outcomes of organ preserving pancreatic head resection compared to pancreaticoduodenectomy interms of increased postoperative morbidity, longer hospital stay, longer operative time and lower quality of life [27]. Organ preserving procedures proposed by Beger and Frey are now a day’s more popular among the pancreatic surgeons than the respective procedures, because it combines the feature of resection as well as drainage. Izbicki and Bloeche have shown in their study that Frey procedure is a “patient friendly” procedure and has zero mortality and a low morbidity rate [28]. Our mortality and morbidity (12.1%) rates associated with the procedure are well within the acceptable range. Major postoperative complications in the current series include pancreatic leakage which was managed conservatively. In a recent meta-analysis done by Zhou Y et al., involving 23 studies comprising of 800 patients found that Frey procedure had favorable outcomes in terms of operation time, blood transfusion, overall morbidity, length of hospital and intensive care unit stay, pancreatic function and quality of life as compared to pancreaticoduodenectomy and Beger procedure [18].
CP is an incurable progressive inflammatory disease of pancreas. Therefore the aim of any surgical intervention in patients with CP is to improve the quality of life, of the patient along with relief from abdominal pain. Studies have shown that 70-80% of the patient, who underwent Frey procedure, had good pain relief [29–32] and improved quality of life [18,29]. In our series all the patients have significant improvement in pain and in all domains excepting for the last two follow up values in social domain, which may be due to patients lost to follow up. This observation further confirmed that the Freys’ procedure does improve the quality of life as shown by other studies.
Preservation of already limited functionality of the pancreas, occupational rehabilitation and increase in quality of life following surgery should be used in the evaluation of therapeutic success of any surgical procedure done for CP [18,33,34]. Collection of data on quality of life should be done with the help of standardized questionnaires so that effective comparison of different surgical procedures for CP is possible.
Limitation
Small sample size and short duration of follow up are the limitations of this study. We used EORTC QLQ-C30 (version 3) Questionnaire as an instrument for quality of life assessment in our study which is a general health questionnaire used for cancer patient and is not specific for CP. We have categorized all the 30 questions of the questionnaire into five domain i.e. physical function domain, physical domain, emotional domain, social domain and global health score to make the analysis simple and easy to interpret.
Conclusion
Quality of life has always been the most important decisive factor for patients with CP. The patients usually have debilitating abdominal pain and depend on chronic opioid analgesics. Freys’ procedure helps in ductal decompression along with resection of the “pacemaker of pain”, that is the head of the pancreas, with excellent outcome when compared with other surgical techniques. It improves quality of life and gives the patient long term relief from pain and suffering. We recommend Frey procedure as a standard method of therapy for chronic pancreatitis. This method is easier, organ-preserving and associated with minimal mortality and morbidity.
Disclosure: We don’t have any financial support for publication of this study.
Appendix 1: EORTC QLQ-C30 (Version 3)
We are interested in some things about you and your health. Please answer all of the questions yourself by circling the number that best applies to you. There is no "right" or "wrong" answers. The information that you provide will remain strictly confidential.
Please fill in your initials:
Your birth date (Day, Month, and Year):
Today’s date (Day, Month, Year):
| Not at All | A Little | Quite a Bit | Very Much |
| 1. Do you have any trouble doing strenuous activities, like carrying a heavy shopping bag or a suitcase? | 1 | 2 | 3 | 4 |
| 2. Do you have any trouble taking a long walk? | 1 | 2 | 3 | 4 |
| 3. Do you have any trouble taking a short walk outside of the house? | 1 | 2 | 3 | 4 |
| 4. Do you need to stay in bed or a chair during the day? | 1 | 2 | 3 | 4 |
| 5. Do you need help with eating, dressing, washing yourself or using the toilet? | 1 | 2 | 3 | 4 |
| During the past week: | Not at All | A Little | Quite a Bit | Very Much |
| 6. Were you limited in doing either your work or other daily activities? | 1 | 2 | 3 | 4 |
| 7. Were you limited in pursuing your hobbies or other leisure time activities? | 1 | 2 | 3 | 4 |
| 8. Were you short of breath? | 1 | 2 | 3 | 4 |
| 9. Have you had pain? | 1 | 2 | 3 | 4 |
| 10. Did you need to rest? | 1 | 2 | 3 | 4 |
| 11. Have you had trouble sleeping? | 1 | 2 | 3 | 4 |
| 12. Have you felt weak? | 1 | 2 | 3 | 4 |
| 13. Have you lacked appetite? | 1 | 2 | 3 | 4 |
| 14. Have you felt nauseated? | 1 | 2 | 3 | 4 |
| 15. Have you vomited? | 1 | 2 | 3 | 4 |
| 16. Have you been constipated? | 1 | 2 | 3 | 4 |
| During the past week: | Not at All | A Little | Quite a Bit | Very Much |
| 17. Have you had diarrhea? | 1 | 2 | 3 | 4 |
| 18. Were you tired? | 1 | 2 | 3 | 4 |
| 19. Did pain interfere with your daily activities? | 1 | 2 | 3 | 4 |
| 20. Have you had difficulty in concentrating on things, like reading a newspaper or watching television? | 1 | 2 | 3 | 4 |
| 21. Did you feel tense? | 1 | 2 | 3 | 4 |
| 22. Did you worry? | 1 | 2 | 3 | 4 |
| 23. Did you feel irritable? | 1 | 2 | 3 | 4 |
| 24. Did you feel depressed? | 1 | 2 | 3 | 4 |
| 25. Have you had difficulty remembering things? | 1 | 2 | 3 | 4 |
| 26. Has your physical condition or medical treatment interfered with your family life? | 1 | 2 | 3 | 4 |
| 27. Has your physical condition or medical treatment interfered with your social activities? | 1 | 2 | 3 | 4 |
| 28. Has your physical condition or medical treatment caused you financial difficulties? | 1 | 2 | 3 | 4 |
For the following questions please circle the number between 1 and 7 that best applies to you
29. How would you rate your overall health during the past week?
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Very poor | | | | | | Excellent |
30. How would you rate your overall quality of life during the past week?
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Very poor | | | | | | Excellent |
Appendix 2 Classification of the 30 questions of EORTC QLQ-C30 (3) questionnaire into five domains
| Domain | Item(Question) numbers | Scores(min-max) |
|---|
| Physical functional domain(PFD) | 1-7, 11 and 13 | 9-22 |
| Physical domain(PD) | 8-10, 12, 14-19 | 10-40 |
| Emotional domain(ED) | 20-25 | 6-24 |
| Social domain(SD) | 26-28 | 3-12 |
| Global health (GH) | 29-30 | 2-14 |
BMI: Body Mass Index
[n= number of patients, s.e.= standard error] VAS: visual analogue scale
[S: Significant, NS: Not significant, PO: Preoperative, PFD: Physical function domain, PD: Physical domain, ED: Emotional domain, SD: Social domain, GH: General health]