Primary Paratesticular Lymphoma with Testicular Sparing: Account of an Unusual Scrotal Mass
Vidya Monappa1, Ranjini Kudva2, Satadru Ray3
1 Associate Professor, Department of Pathology, KMC, Manipal University, Manipal, India.
2 Professor, Department of Pathology, KMC, Manipal University, Manipal, India.
3 Professor, Department of Surgical Oncology, KMC, Manipal University, Manipal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vidya Monappa, Associate Professor, Department of Pathology, Basic Science Block, Kasturba Medical College, Manipal University, Manipal, Karnataka-576104, India.
E-mail: vidsdr@yahoo.co.in
Tumours of the testicular adnexa include a heterogeous group of mesothelial, mesenchymal and germ cell tumours. Adenomatoid tumour, pseudosarcomatous myofibroblastic proliferations and rhabdomyosarcoma are the more frequently encountered neoplasms. Lymphoma/leukemic infiltration secondary to testicular involvement or primary tumour elsewhere is not unusual. However, Primary Para-Testicular Lymphoma (PPTL) involving spermatic cord and/or epididymis with sparing of the testicular parenchyma is extremely rare. Accurate staging and typing is crucial for effective management.
We present a rare case of Diffuse Large B Cell Lymphoma (DLBCL) involving the left paratesticular tissue with testicular sparing in a young immunocompetant male patient.
DLBCL, NHL, Paratesticular tumours
Case Report
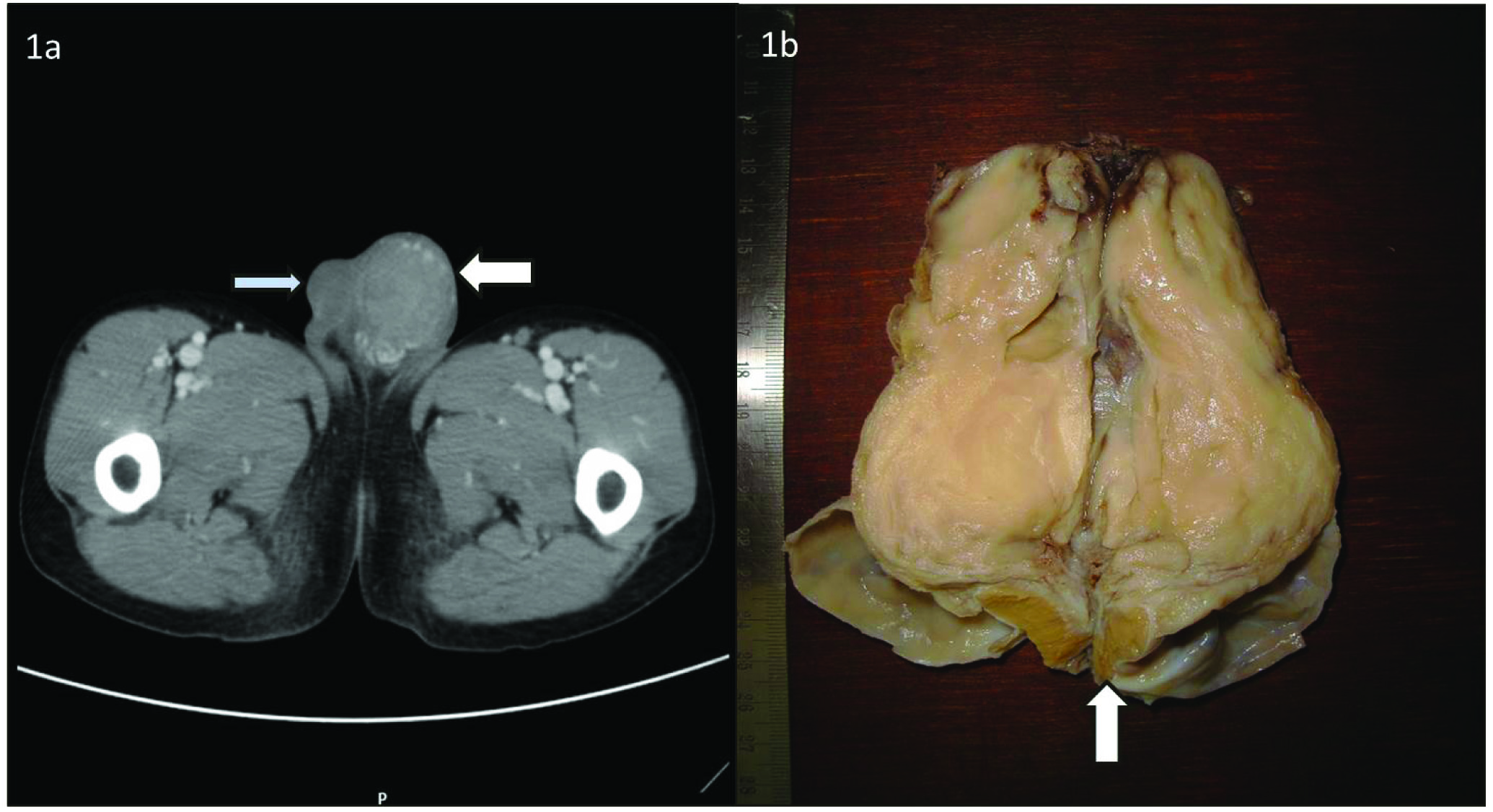
A 17-year-old boy presented with 6 weeks history of upper abdominal discomfort and 2 weeks history of painless left sided testicular swelling. Examination revealed 5x6cm non fluctuant, non tender left testicular swelling with vague mass in epigastric and right hypochondriac region. There were no palpable neck, axillary or groin nodes. Systemic examination was within normal limits. Routine laboratory investigations were normal, apart from elevated serum LDH levels (570 IU/L). Ultrasonography (USG) scrotum with colour Doppler revealed mass lesion in left epidydimis displacing the testis inferiorly. CT abdomen and pelvis region revealed a heterogeneously enhancing mass in the scrotum involving left spermatic cord, seminal vesicle and prostate with loss of fat planes [Table/Fig-1a]. Right testis was normal. Multiple para aortic and retroperitoneal lymph nodes suggestive of lymphoma / tumour was observed.
a) CT image showing a heterogeneously enhancing mass in scrotum (white arrow); right testis appears normal (blue arrow); b) Cut section of left high orchidectomy specimen showing paratesticular lymphoma with homogenous fish flesh appearance totally involving epidydimis and spermatic cord with compressed left testis at one end (arrow).
Review of Fine Needle Aspiration Cytology (FNAC) slides performed elsewhere, showed dispersed population of atypical lymphoid cells suggestive of Non Hodgkin Lymphoma.
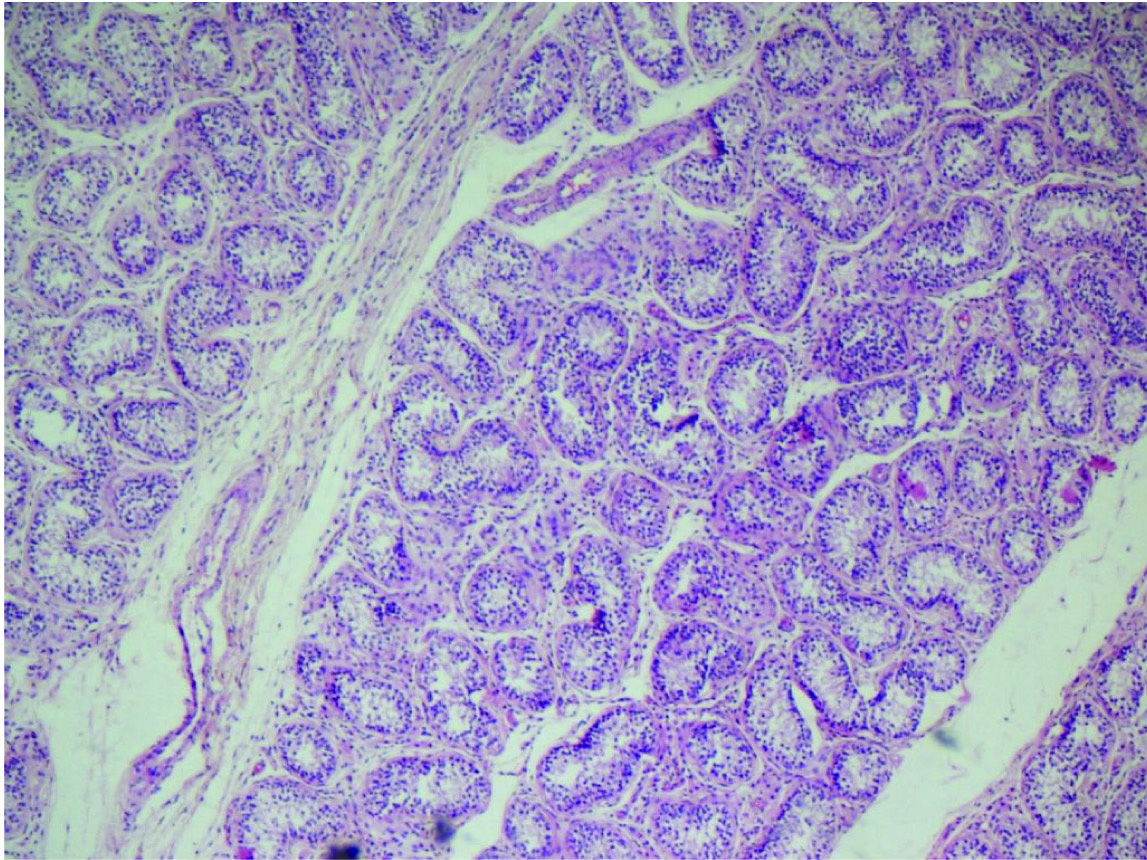
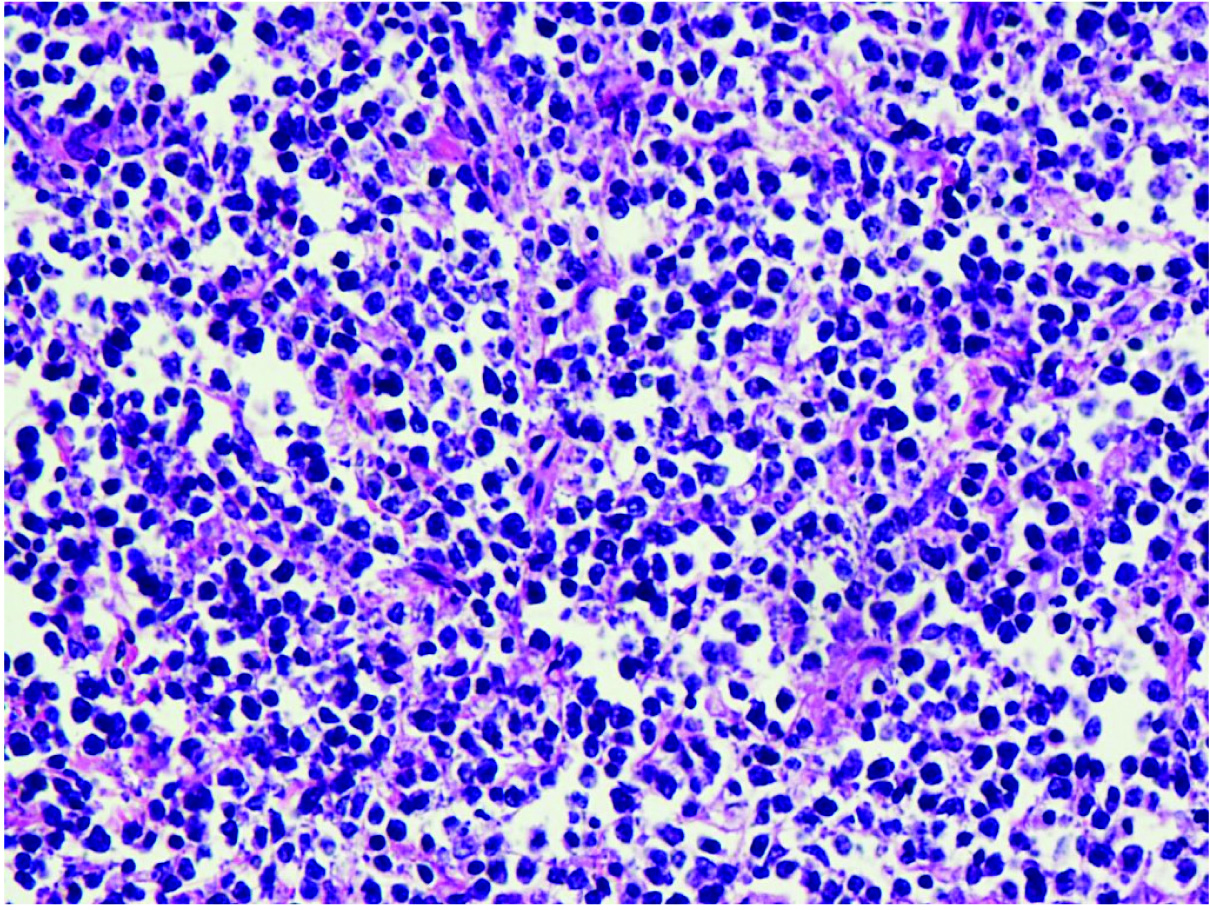
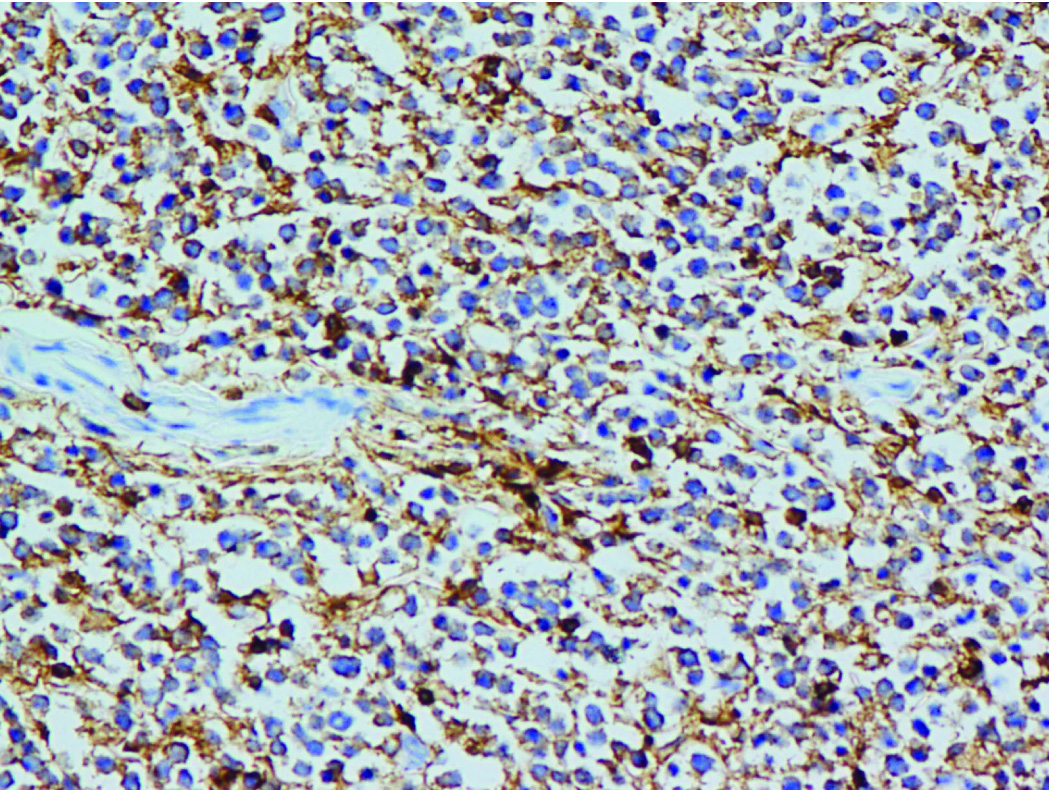
Patient underwent left high orchidectomy. Grossly, specimen weighed 119gm and measured 13x5x2cm with smooth external surface. Spermatic cord was markedly thickened. Cut section showed compressed testis at one end with paratesticular tissue showing a tumour with homogenous grey-white “fishflesh” appearance [Table/Fig-1b]. Microscopically testis showed atrophic changes with intact tunica albuginea [Table/Fig-2]. Paratesticular tumour showed diffuse infiltration by large atypical lymphoid cells with irregular nuclear membrane, coarse granular chromatin, one or more prominent nucleoli with scant cytoplasm (suggestive of centroblast) and increased mitosis; foci of necrosis and fibrous strands dividing the tumour cells into nests was seen [Table/Fig-3]. Immunohistochemically the tumour cells were CD45 +/, CD20+ve [Table/Fig-4] and CD3 -/. A final diagnosis of Paratesticular Diffuse Large B Cell Lymphoma (DLBL) was offered. Bone marrow biopsy performed to rule out disseminated lymphoma was negative. Clinical staging was IVB.
Section from testis showing atrophic seminiferous tubules. (H&E; X-200).
Section shows diffuse infiltration by large lymphoid cells with 1 or more nucleoli, areas of necrosis and delicate fibrous strands dividing tumour into nests. (H&E; X400).
CD20 Diffuse membrane positive in the neoplastic lymphoid cells. (CD20; X400).
Patient received 3 courses of R-CHOP chemotherapy with G-CSF support. At the time of last follow-up he was under complete remission.
Discussion
Primary lymphomas in extranodal sites have been documented in the skin, gonads, bone, brain, lung, salivary glands, tonsil, prostate, uterus, and thyroid [1]. Lymphoma arising in paratesticular region could be primary or secondary to primary testicular lymphomas or as part of systemic dissemination of lymphoma elsewhere. Careful clinico-pathological staging is therefore crucial [2].
DLBCL is the most common extranodal lymphoma encountered in the central nervous system, eyes, paranasal sinuses, Waldeyer ring, bone, heart, adrenals, and testis. This is commonly seen in older adults, around seventh decade, but younger adults and children can occasionally be affected. There is a slight male preponderance overall, but this varies among anatomic sites. Increased occurrence was also observed in HIV positive patients [1].
PPTLs are exceedingly rare. Review of the literature uncovered 49 cases, of which 38 cases involved the spermatic cord [3], 10 cases were confined to the epididymis [4,5] while one case involved both these sites [4]. The present case involved both the epididymis and spermatic cord.
Clinically PPTLs present with painless masses in inguinoscrotal region, usually without any history of weight loss, fever or night sweats [6,7]. The present case was unusual, as it occurred in a young patient with a HIV negative status. Because these tumours are rare, they are generally not considered in the differential diagnosis of neoplastic or non-neoplastic lesions of the paratestis. There have been instances of PPLT being falsely considered as hernias [8,9].
Vega et al., reviewed 6 cases of primary lymphoma of epidydimis and 12 cases of primary spermatic cord lymphomas in addition to 2 new cases of PPTL [2]. Of these, only 7 cases had undergone immunophenotyping, majority (6 cases) being B cell type. Diffuse Large B Cell Lymphoma (DLBCL) was the commonest morphologic type described.
Bertolotto et al., discussed the radiological findings of a case of spermatic cord lymphoma [3]. They opined that the tumour tissue appeared hypoechoic under Colour Doppler Ultrasound (US). The tissue surrounding the normal spermatic vessels appeared hypervascular under contrast enhanced US with homogenous enhancement. MRI showed diffuse tumour infiltration which was hypointense on T2-weighted and iso-intense to testis on T1-weighed images. They proposed that a specific diagnosis of this rare tumour was achievable through integration of different imaging modalities.
Tralongo V et al., reviewed 8 cases of primary epididymal lymphomas while reporting a new case of primary follicular lymphoma [4]. The histologic typing was mentioned in only two cases as Histiocytic lymphoma and Mucosa Associated Lymphoid Tissue (MALT) lymphoma. Rajaian et al., reported a case of marginal zone lymphoma of the epididymis [5].
In the present case systemic lymphoma was ruled out as there was no peripheral lymphadenopathy, hepatosplenomegaly or bone marrow involvement. Morphologically, the tumour showed CD20 positive large lymphoid cells, which was consistent with the diagnosis of DLBCL. Testicular sparing could possibly be explained owing to the shielding effect of the tunica media.
The primary lymphomas of the testis and spermatic cord have the worst prognosis among all extranodal lymphomas, with the 5-year overall survival ranging between 70 and 79%. They are known for aggressive behaviour with frequent involvement of nodal and extranodal sites at presentation and relapse. Favourable factors are lymphoma sclerosis, young age and early stage. Therapy of choice is surgical excision and chemotherapy (CHOP), followed by radiotherapy [10].
Conclusion
PPTLs are extremely rare tumours with an aggressive clinical course. DLBL is the commonest histologic type, however other variants have also been described. Proper clinical staging is crucial to exclude the systemic spread from lymphoma elsewhere. Radiologically, they have distinct features and a combination of different imaging modalities is effective in rendering the diagnosis. The present case involved both spermatic cord and epididymis while sparing the testis.
[1]. Ferry JA, Extranodal lymphomaArch Pathol Lab Med 2008 132:565-78. [Google Scholar]
[2]. Vega F, Medeiros LJ, Abruzzo LV, Primary paratesticular lymphoma – A report of 2 cases and review of the literatureArchives of Path and Lab Medicine 2001 125(3):428-32. [Google Scholar]
[3]. Bertolotto M, Borsato A, Derchi LE, Lymphoma of the spermatic cord: Sonographic appearanceJournal of clinical ultrasound 2014 42(8):509-12. [Google Scholar]
[4]. Tralongo V, Becchina G, Nagar C, Ottoveggio G, Mason S, Seno B, Primary follicular lymphoma of the epididymis positive for t(14;18)(q32;q21)/IGH-BCL2 and negative for BCL2 protein expression: a case reportJournal of Medical Case Reports 2012 6:24 [Google Scholar]
[5]. Rajaian S, Manipadam MT, Nair S, Kakre NS, Primary extranodal marginal zone lymphoma – EpididymisIndian Journal of Urology 2011 27(4):53-55. [Google Scholar]
[6]. Lagrange JL, Ramaioli A, Theodore CH, Terrier-Lacombe MJ, Beckendorf V, Biron P, Non-Hodgkin’s lymphoma of the testis A retrospective study of 84 patientsAnn Oncol 2001 12:1313-19. [Google Scholar]
[7]. D’Abrosca F, Lucev M, Turi V, Gerosa E, Villani L, Primary lymphoma of the spermatic cordMinerva Chir 1990 45:531-33. [Google Scholar]
[8]. Michael B, Moller Non Hodgkin’s lymphoma of the spermatic cordActa Haematol 1994 91:70-72. [Google Scholar]
[9]. D’Abrosca F, Lucev M, Turi V, Gerosa E, Villani L, Primary lymphoma of the spermatic cordMinerva Chir 1990 45:531-33. [Google Scholar]
[10]. Diakatou E, Haramis G, Kostopoulou A, Kakiopoulos G, Primary lymphoma of the spermatic cord: A case report and review of the literatureIndian J Pathol Microbiol 2011 54:588-90. [Google Scholar]