GIST Jinx – A Rare Case of Acute Massive Life Threatening Bleed from a Jejunal Gastro-Intestinal Stromal Tumour
Pranav Honnavara Srinivasan1, Joji I Maliekal2, Chaganty Saikiran Reddy3, Sriharsha Suda4
1 Senior Resident, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
2 Professor and Head, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
3 Post Graduate Student, Department of Pathology, Government Medical College, Kozhikode, Kerala, India.
4 Senior resident, Department of General Surgery, Government Medical College, Kozhikode, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pranav Honnavara Srinivasan, 816, 37th Cross, 18th main, 4th T block, Jayanagar, Bangalore – 560041, India.
E-mail: pranavhs8@gmail.com
Melena, Gastrointestinal haemorrhage, Jejunum
A 55-year-old lady presented to us in the emergency services with melaena. Haemoglobin was 3.4 g/dL. A massive blood transfusion was given. Upper Gastrointestinal (GI) endoscopy showed antral erosions without active bleed and colonoscopy was inconclusive. An Ultrasonogram (USG) of the abdomen showed multiple haemangiomas of the liver and no bowel pathology. A Contrast Enhancing Computed Tomogram (CECT) of the abdomen showed an intensely enhancing lesion in the jejunum. Laparotomy revealed a firm hypervascular mass 3x3cm in the proximal jejunum 6cm distal to the duodeno-jejunal junction. The mass was resected and on histopathological examination was found to be a low-risk GIST with adequate margins and c-KIT (CD 117) positivity.
Clinically, severe pallor was present. The abdominal examination was within normal limits. Digital rectal examination revealed melaena staining. On proctoscopy, the lower rectum could not be visualised due to the melaena.
Laboratory findings: Haemoglobin 3.4 g/dL, bleeding and coagulation parameters were within normal limits
On Endoscopy of Upper GI, Antral erosions were noted with no active bleeding. Colonoscopy was inconclusive as rectum was filled with melaena resulting in poor visibility.
Abdominal USG showed multiple haemangiomas in the liver with no abnormal bowel pathology visualised.
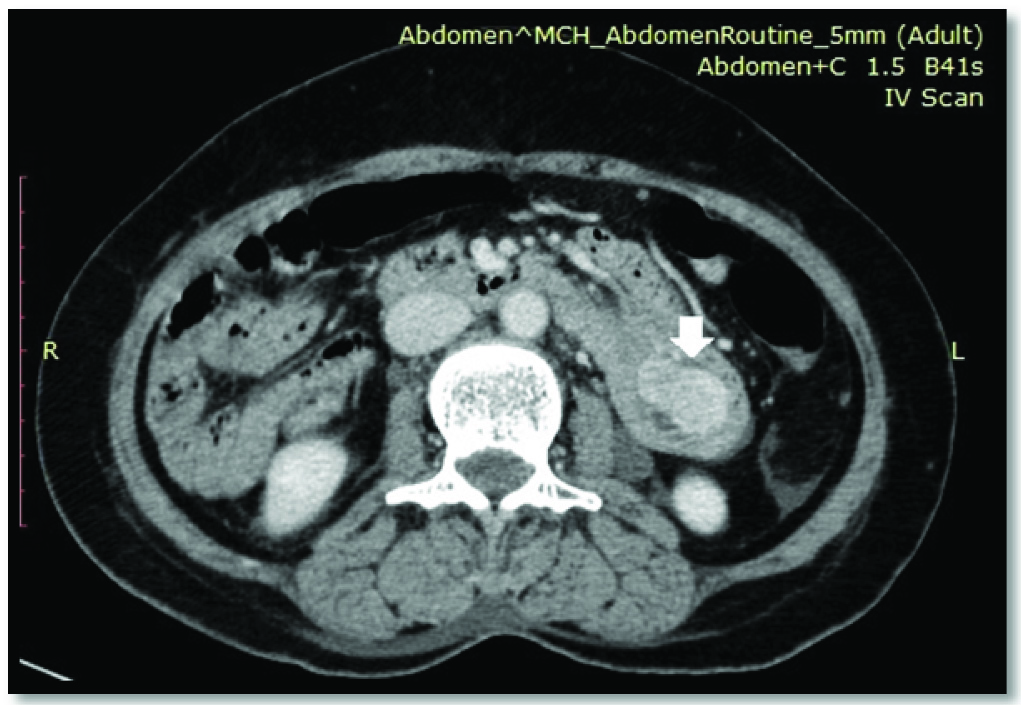
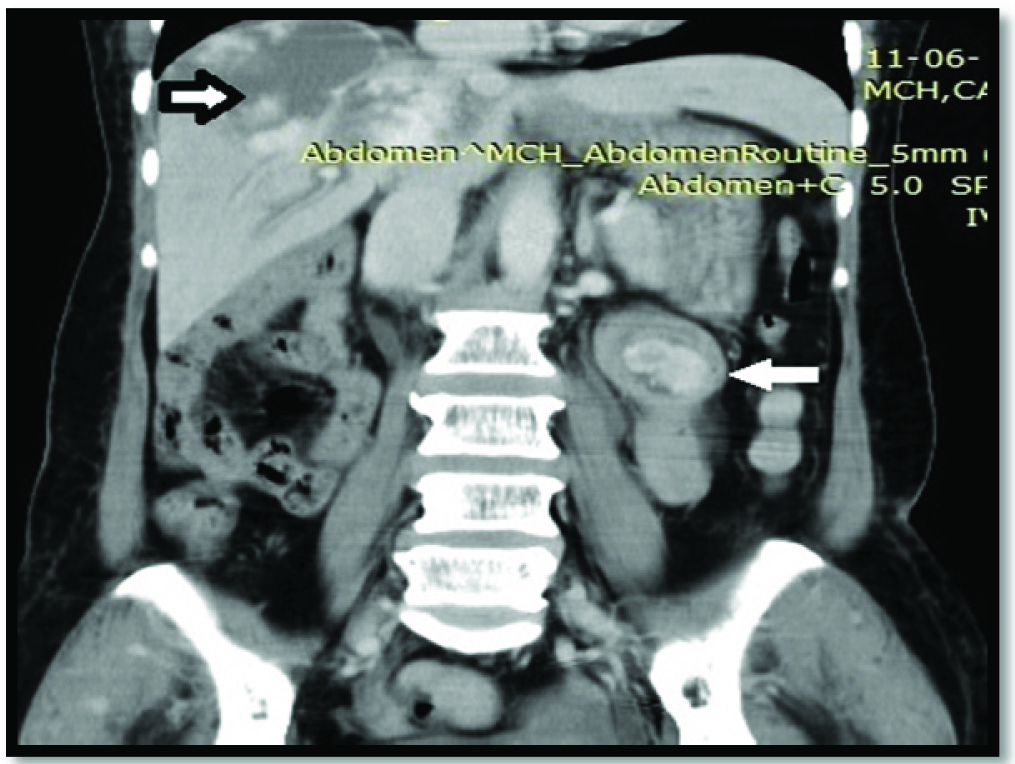
CECT abdomen showed Duodeno-Jejunal intussusception [Table/Fig-1] with intensely enhancing submucosal lesion with the same intensity as that of blood vessels with probable diagnosis being a growth of vascular origin. Multiple liver haemangiomas were also visualised [Table/Fig-2].
An abdominal CT transverse slice showing intensely enhancing lesion with duodeno-jejunal intussusception (white arrow).
An abdominal CT coronal slice showing liver haemangiomas (black arrow) and duodeno-jejunal intussusception with intensely enhancing submucosal lesion (white arrow).
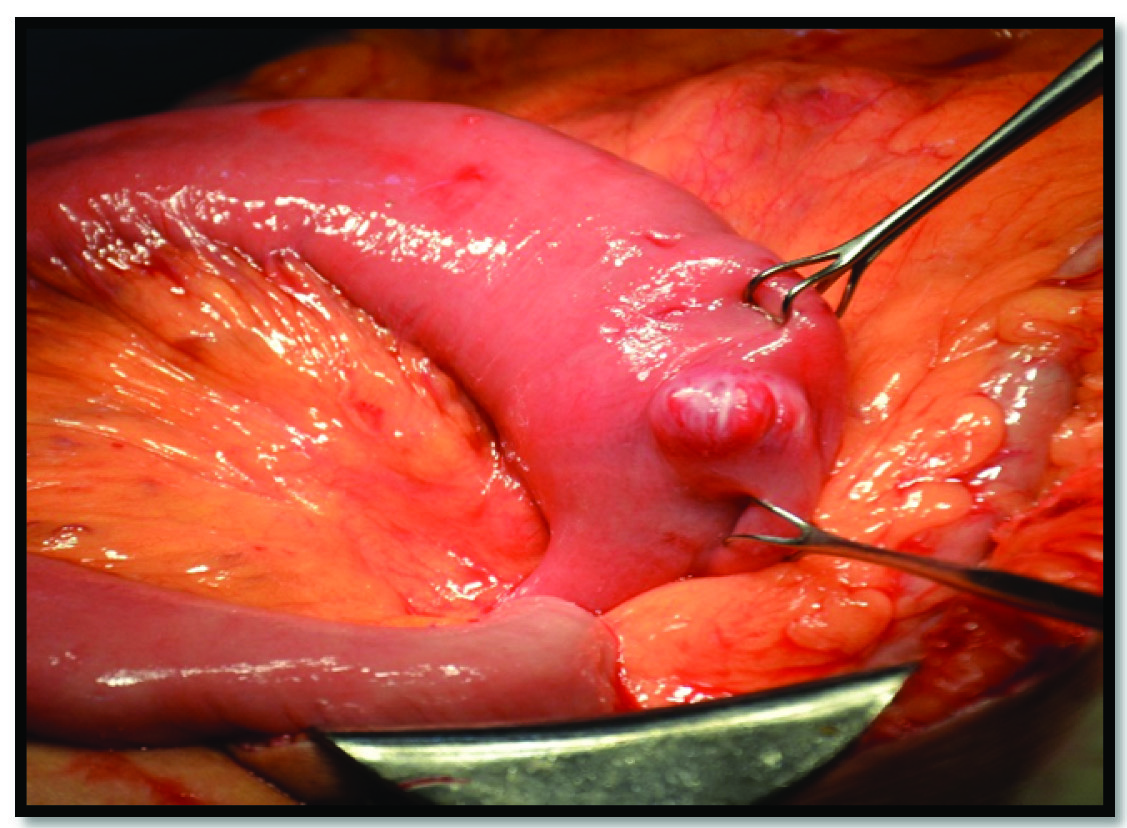
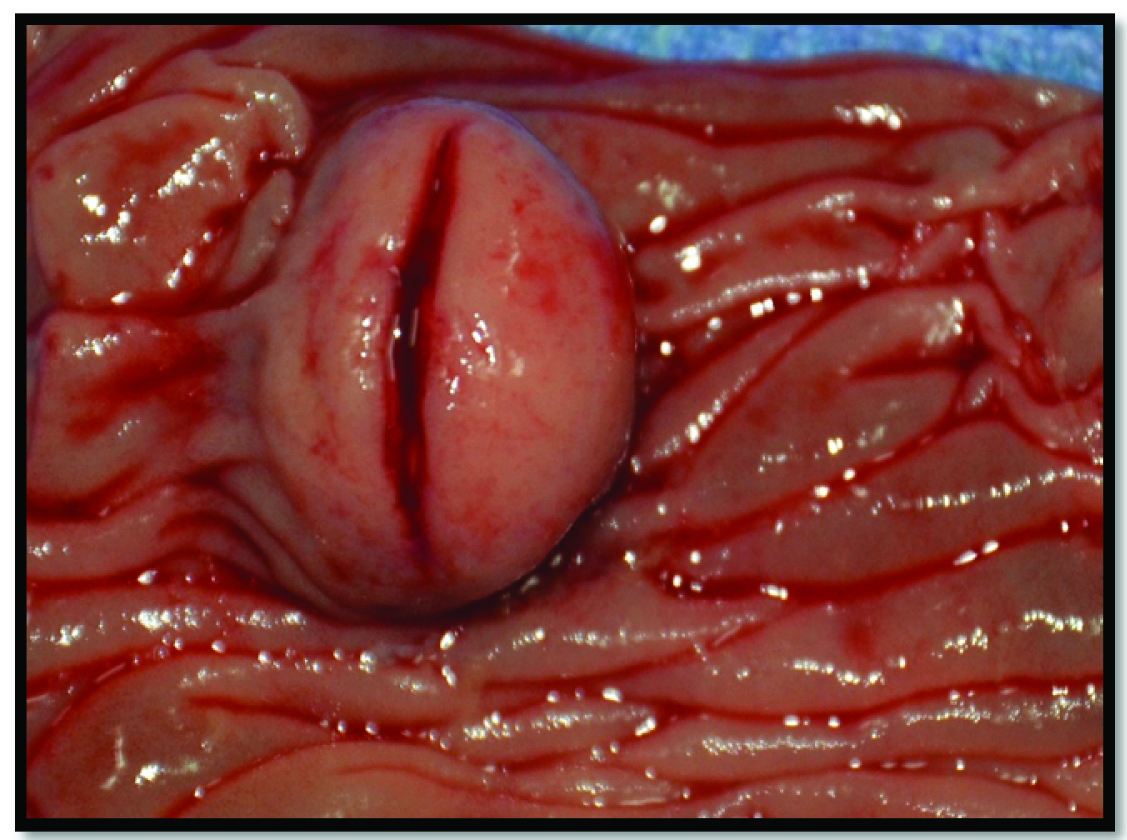
Gross findings: Laparotomy revealed a firm well circumscribed mass 3x3cm, arising from the anti-mesenteric border of the jejunum 6 cm distal to the duodeno-jejunal flexure with dilated peritumoural vessels. The intraluminal portion of the affected bowel showed a full diameter transverse slit across the tumour representing rupture which probably caused the massive bleed [Table/Fig-3,4].
Intraoperative photograph showing the lesion near the duodeno-jejunal junction
Intra-luminal photograph showing the lesion with intraluminal rupture.
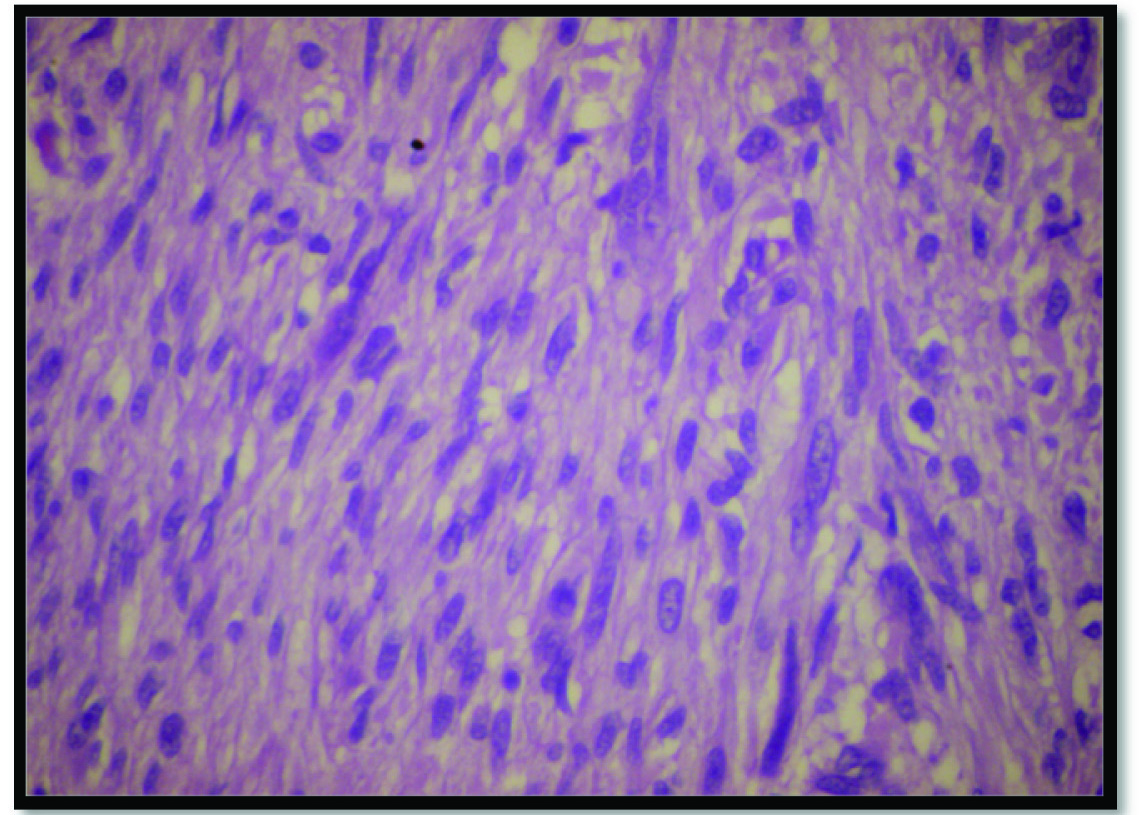
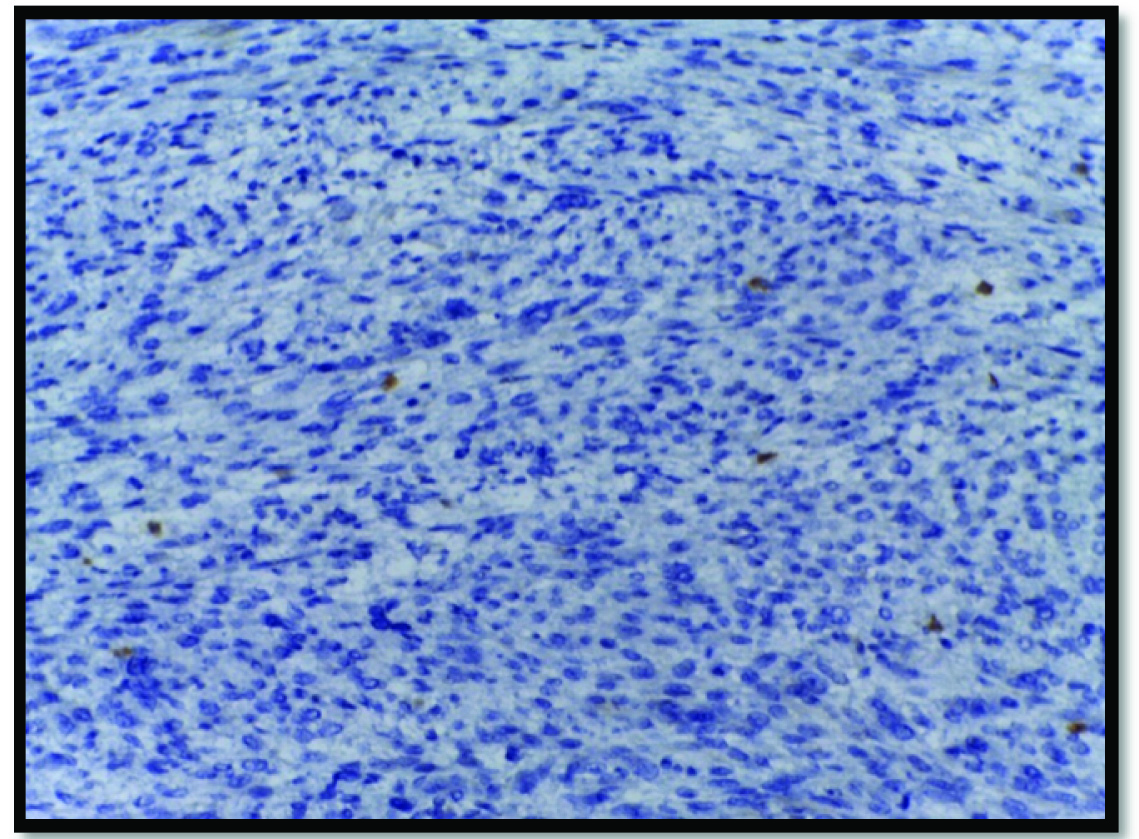
Microscopy: Microscopy with classical haematoxylin and eosin staining revealed clusters of spindle shaped cells with elongated nuclei with areas of mitosis. Immunohistochemistry demonstrated positivity for CD 117 [Table/Fig-5,6].
Photomicrograph showing spindle shaped cells with irregular large nuclei with intervening stroma (H & E, x 400).
Photomicrograph demonstrating spindle shaped cells with large nuclei with CD117 positivity in few cells (Immunohistochemistry staining, x 100).
GISTs are the most common sarcomatous tumours of the GIT, typically seen in patients more than 50 years with slight male preponderance. The most common sites in the GIT include stomach (50-60%), small intestine (25-30%), rectum (5%), oesophagus (2%). Jejunal GISTs are rare, contributing to only 10% of GISTs arising from the GIT [1,2]. Histologically, GISTs consist of a combination of spindle and epitheloid cells. Immunohistochemistry for GISTs typically shows positivity for the tyrosine kinase receptor protein – c-KIT (CD 117) [3].
Most patients with GISTs present symptomatically with variable clinical presentation. Small GISTs usually present as vague abdominal pain or with bleeding. Bleeding is most common into the lumen of the GIT which is usually chronic in presentation. Acute massive life threatening intraluminal bleed is very rare. CECT abdomen findings typically are of a well circumscribed submucosal mass or of an exophytic lesion. Endoscopy can also be used for pre-operative diagnosis in accessible locations. A pre-operative diagnosis is difficult especially in cases presenting as emergency and diagnosis is usually confirmed at surgery.
Complete surgical resection forms the mainstay of treatment.
Small bowel GIST is an unusual tumour of the GIT and can have varied clinical presentation. Its presentation as acute massive GI haemorrhage is rare. Aggressive resuscitation, a high index of suspicion and thorough clinical and radiological evaluation are necessary to provide the best possible treatment.
[1]. Zhao X, Yue C, Gastrointestinal stromal tumourJ Gastrointest Oncol 2012 3(3):189-208.doi: 10.3978/j.issn.2078-6891.2012.031 [Google Scholar]
[2]. Corless CL, Fletcher JA, Heinrich MC, Biology of gastrointestinal stromal tumoursJ Clin Oncol 2004 22(18):3813-25. [Google Scholar]
[3]. Miettinen M, Lasota J, Gastrointestinal stromal tumours: review on morphology, molecular pathology, prognosis, and differential diagnosisArch Pathol Lab Med 2006 130(10):1466-78. [Google Scholar]