Over the last couple of decades there has been a rapid development in imaging technology that has transformed the diagnosis and management of the various spinal injuries including injuries to the spinal cord. Traumatic injuries of the spine and spinal cord are very common [1] and such injuries can cause potentially devastating lesions that may lead to significant neurological damage.
The clinical and prognostic implications of spinal injuries are vast as patients in whom neurological examinations fail to register any motor/sensory preservation due to severe spinal cord injuries tend to have a poor prognosis whereas patients who present with an incomplete injury may retain a large amount of useful function. In several instances, progression of injury may be halted by timely diagnosis and treatment and imaging studies play an extremely vital role in detecting any abnormality that compromises the integrity of the canal and the spinal cord.
The radiologist must design and choose a tailored multimodality protocol to image the spine in the best possible way keeping in mind various other factors [2]. Over the recent past, there has been a shift from plain radiography to Multi-Detector Computed Tomography (MDCT) which provides a faster and more accurate evaluation of the spine [3].
Advances in Magnetic Resonance Imaging (MRI) technology has made it an essential tool in imaging of acute spinal trauma and is the gold standard for detecting injuries to the spinal cord. While MDCT is done more routinely in all cases of spinal trauma seemingly without any specified protocols, MRI is generally restricted to either patients with negative radiographs and negative MDCT who have neurologic symptoms or for preoperative planning in patients with fracture or unstable injury noted on radiographic or MDCT work-up [4].
Studies by Benzel, Goldberg, Kihiczak and others have indirectly compared MR imaging with MDCT or radiography and determined its utility as compared to conventional imaging [5–8]. Some studies included neurologic outcome as the reference standard [9–11].
Few have attempted direct correlation between anatomic or surgical findings and imaging findings, either utilizing cadavers [12] or intraoperative verification for those patients who went on to surgery based on clinical or imaging findings [13–15].
To compare and correlate soft tissue injuries detected on MRI in cases of spinal trauma to the intraoperative evidence found by the surgeon.
Materials and Methods
This prospective observational study was conducted from October 2011 to September 2013 in a private medical college hospital in Mangalore to compare MR imaging of the spine with surgical observations following approval from the Instituional Ethical Committee. The study included a total of 63 consecutive patients who underwent MRI scan for spinal trauma. However, out of these, only 31 were included in this study as they presented within 72 hours of the trauma and underwent surgical fixation by either an anterior or posterior approach following imaging after obtaining an informed consent. Patients unfit/unwilling for the MRI/surgery were excluded from the study as were those who presented 72 hours after onset of injury.
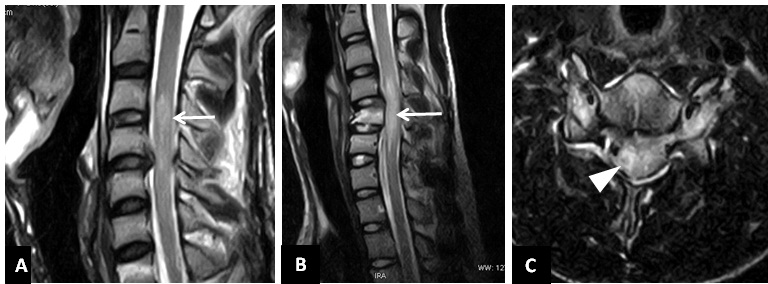
All MR imaging scans were obtained on a 0.4T Hitachi Aperto system (Hitachi Medical Corporation, Tokyo, Japan) using an imaging protocol as listed in [Table/Fig-1]. Evaluation of the preoperative MR imaging scans was performed by a consultant Radiologist on a GE AW Volume Share 2 workstation (General Electric Medical Syste, USA). We evaluated the following structures on MR imaging, from anterior to posterior: Anterior Longitudinal Ligament (ALL), intervertebral disc, Posterior Longitudinal Ligament (PLL), Spinal Cord, Ligamentum Flavum and Interspinous soft tissues. Presence and degree of injury were identified. The ALL, PLL and Ligamentum Flavum were considered abnormal if they demonstrated high T2 signal intensity or displacement or loss of continuity tear. Examples of such are depicted in [Table/Fig-2,3]. The Intervertebral disc and Interspinous ligament were considered abnormal if they demonstrated high T2 signal intensity or complete disruption as represented in [Table/Fig-4,5]. Similarly, the cord was best evaluated in the Sagittal T2 weighted images and was considered abnormal if they showed any focus of long T2 relaxation times as demonstrated in [Table/Fig-6].
Imaging protocol followed for MRI scans.
| Imaging plane | Sequence |
|---|
| Sagittal | T1 (TR 500–600, TE 10) |
| T2 (TR 2700–4000, TE 75) |
| STIR (TR 3500 – 4300, TE 30, TI 140 –180) |
| Gradient Echo (TR 610, TE 17, flip angle 10°) |
| Axial | T1 (TR 500–600, TE 10) |
| T2 (TR 2700–4000, TE 75) |
| STIR (TR 3500 – 4300, TE 30, TI 140 –180) |
| Gradient Echo (TR 610, TE 17, flip angle 10°) |
| Coronal | T2 (TR 2700–4000, TE 75) |
| STIR (TR 3500 – 4300, TE 30, TI 140 –180) |
| MRA (Cervical spine) | 2D Time-of-Flight |
TR: Time to Repetition, TE: Time to Echo expressed in milliseconds, STIR: Short TI inversion recovery.
Two cases of traumatic spondylolisthesis shows elevation of the anterior longitudinal ligament as seen in (a) whereas in (b) there is discontinuity of the ALL suggestive of disruption, along with associated anterior disc herniation (Solid arrows). There is also associated elevation of the posterior longitudinal ligament in both these cases (arrowheads). Injuries were confirmed at surgery.
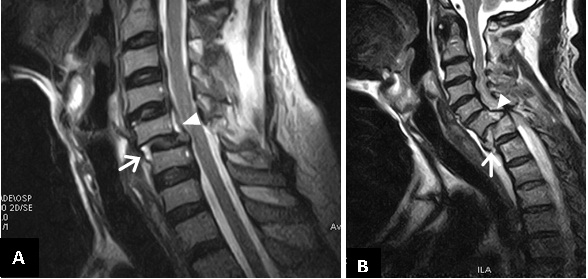
Two other cases of traumatic spondylolisthesis showing a disrupted Posterior longitudinal ligament (white arrowhead) along with disruption of the ligamentum flavum (black arrow) which were confirmed at surgery.

A case of true positive disc injury. The intervertebral disc at C5-C6 level shows high T2 signal intensity along with reduced disc height and posterior herniation into the spinal canal (black arrow) resulting in compression of the cervical cord.

Sagittal STIR image of the cervical spine shows high signal intensity in the posterior paraspinal region (white arrowhead) which was suggestive of injury to the Interspinous ligament. There is also elevation of the posterior longitudinal ligament and high signal intensity within the cervical cord suggestive of cord oedema (black arrowhead).

Sagittal T2 weighted image of a patient with acute cervical cord injury in (a) and T2 weighted sagittal and axial image of another patient (b) and (c), show high signal intensity within the cord on sagittal images (white arrow), whereas on the axial image the cord appears bulky with increased signal intensity (white arrowhead). These imaging features were suggestive of Cord Oedema.
Patients also underwent other individual investigations for surgical or anaesthetic clearance as per the treating surgeon’s orders.
Intraoperatively the extent of injury at the operated level was recorded for either anterior or posterior structures or both depending upon the operative approach. The operative approach determined which structures were adequately visualized by the surgeon and was modeled in a pattern similar to Goradia et al., according to which structures evaluated were; from the anterior approach, the anterior longitudinal ligament (ALL), disc annulus, vertebral body, and posterior longitudinal ligament (PLL) were generally visualized at the level of surgery [4]. There was limited-to-absent visualization of posterior structures. Similarly, for the posterior approach, the superficial dorsal soft tissues, interspinous soft tissues, ligamentum flavum, and posterior osseous elements were visualized at the level of surgery. From this approach the anterior structures were difficult to assess. Therefore, surgical information was dependent on the approach. The level that was operated on determined which structures were visualized depending on the anterior/posterior approach. Hence structures that were different from the operative level were not assessed intraoperatively.
For the ligaments, the operating surgeon recorded whether at surgery the structure was intact or partially or completely torn. The intervertebral discs were also evaluated for its integrity as was the spinal cord, seen intraoperatively.
Any of the above described soft tissue structure when found to be injured on the preoperative MRI and correlated with the intraoperative findings were deemed as ‘True-Positive (a)’. Similarly, a structure when found to be normal on the MRI and showed intraoperative correlation was classified as ‘True-Negative’. A structure preoperatively deemed as normal and later found to be injured on surgery was marked as ‘False-Negative (b)’ and vice versa, one as ‘False-Positive’ when diagnosed as injured on MRI and found to be normal on intraoperative correlation. Thus using these above parameters the statistical sensitivity of MRI in detecting injuries to the various soft tissue structures was calculated according to the following equation:
True Positive (a) / True Positive (a) + False Negative (b)
Results
The study comprised of 31 consecutive patients from October 2011 to September 2013 who met the inclusion criteria of being evaluated on MRI within 72 hours for spinal trauma and furthermore underwent operative fixation for the injuries sustained.
Of the 31 patients, there were 26 males and 5 females. Age of these patients ranged from 18 years to 65 years with a median age of 35 years and mean age of 37.6 years.
In 51.6% of patients the site of injury was cervical spine (n=16), thoracic spine was the next highest in occurrence of 39% (n=12) and lumbar spine accounted for 10% of all injuries (n=3).
The mechanism of injury in most cases was found to be due to fall from height (n=14) which in all of our cases involved fall from a tree. The next most common mechanism of injury was due to road traffic accidents (n=11), and lastly due to domestic and other occupational injuries (n=6) that involved direct mechanical trauma to the spine.
Injuries to the soft tissues of the spine were evaluated as described earlier from anterior to posterior is as follows; Anterior Longitudinal Ligament, Intervertebral Disc, Posterior Longitudinal Ligament, Spinal Cord including the conus medullaris, Ligamentum Flavum and Interspinous Ligament.
A total of 15 patients underwent an anterior surgical approach of which 14 were of the cervical spine and one thoracic spine. On the other hand, of the 16 patients who underwent a posterior surgical approach, 14 were of the thoracic spine and 2 of the cervical spine. The operative approach determined which structures were adequately visualized by the surgeon. The total number of structures evaluated using either an anteior/posterior approach is tabulated in [Table/Fig-7].
Number of structures evaluated by either an anterior/ posterior approach.
| Structure Evaluated | Surgical Approach | Total |
|---|
| Anterior | Posterior |
|---|
| Anterior Longitudinal Ligament | 15 | - | 15 |
| Posterior Longitudinal Ligament | 15 | 5 | 20 |
| Intervertebral Disc | 15 | 5 | 20 |
| Spinal Cord/ Conus Medullaris | 15 | 13 | 28 |
| Ligamentum Flavum | - | 16 | 16 |
| Interspinous Ligament | - | 16 | 16 |
The anterior longitudinal ligament was evaluated intraoperatively in 15 patients. Of these, in 9 patients the ALL was found to be injured on surgery of which 6 were detected on the preoperative MR images. The remaining three were reported as false negative, and another was reported as false positive. The sensitivity thus calculated was found to be 66.6%. In 5 patients in whom no abnormality was detected on the MRI, surgical evaluation also revealed a normal anterior longitudinal ligament.
On the other hand, there were a total of 18 injuries to the PLL on intraoperative evaluation. Of these, all but one were detected on the preoperative MRI. In addition to that, there was one which was normal on the MRI and on the subsequent intraoperative correlation and another which was falsely reported as injured on the MRI. However the resultant sensitivity of the MRI stood highly at 94.4%.
Coming to the intervertebral disc, of the total of 12 injuries to the Disc on intraoperative evaluation, 9 were preoperatively detected on the MRI with 3 being interpreted as uninjured (false negative). Hence the resultant sensitivity was calculated to be 75%. There was one patient in whom the disc was interpreted as injured on the MRI, but was found to be normal intraoperatively. In 7 patients the disc was found to be normal on the MRI which was confirmed on the surgical evaluation.
A total of 8 injuries to the Ligamentum Flavum were found on intraoperative evaluation, 5 of which were detected on the preoperative MRI and the remaining three interpreted falsely as uninjured. There were no cases reported as falsely injured and 8 patients in whom no injury was found on the MRI, the subsequent surgical evaluation were found to correlate. Therefore the resultant sensitivity of the MRI was calculated to be 62.5%.
There were a total of 11 injuries to the Interspinous ligament on intraoperative evaluation. Of these, 7 were injured that were detected on the preoperative MRI and a high number of false negatives at 4. Thereby reducing the sensitivity of the MRI to 63.6%. In 5 cases wherein Interspinous ligament was interpreted as normal the surgical findings were found to correlate.
In evaluating injuries to the spinal cord and conus medullaris the MRI was found to have a high sensitivity at 93%, with only one false negative reading out of 14 patients with injury to the spinal cord and the conus.
A summary of the findings described above is displayed in [Table/Fig-8].
Shows a comparative evaluation of the various soft tissue structures that were imaged on MRI and correlated with intraoperative findings.
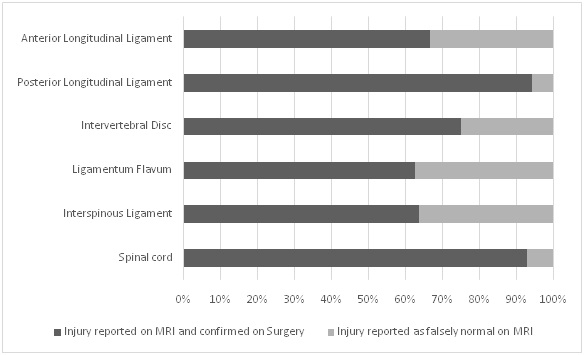
Thereby in evaluating the soft tissue structures of the spine, MRI was found to be highly sensitive in detecting injuries to the spinal cord and the PLL and moderately high for disc injuries. Regarding the anterior longitudinal ligament, ligamentum flavum and the interspinous ligament, there were a high number of false negative interpretations.
Discussion
Spinal fractures are commonly encountered in trauma patients with neurological injury to the spinal cord occuring in 19% to 50% of these patients and a delay in diagnosis of fractures resulting in up to an eightfold increase in neurologic deficits [16,17].
Historically, plain radiographs were part of the standard imaging protocol for evaluation of bony injuries; however, software reconstructed MDCT scans have replaced conventional radiography and has been established as the gold standard for evaluation of spinal fractures, especially involving the posterior neural elements. Magnetic Resonance Imaging (MRI) plays an important role in screening and evaluating patients for neurologic injury, ligamentous injury, and the need for operative intervention.
There have been several studies in this field, however most of the references we found either studied cervical or thoracolumbar injuries not the entire spine like we have performed. Furthermore, we found few studies that compared MRI findings in spinal trauma and correlated them to intraoperative assessment. Hence, we hope these factors provide scientific reasoning and novelty to our research.
In 51.6% of patients the site of injury was cervical spine (n=16), thoracic spine was the next highest in occurrence of 39% (n=12) and lumbar spine accounted for 10% of all injuries (n=3).
In earlier studies, the most common causes of spinal injury were found to be motor vehicle accidents (40.4%) and falls (27.9%) [18–21]. Majority of the patients in our study presented following a fall from height, followed by those who met with a motor vehicle accident.
In our study the non-osseous structures that were evaluated on MR imaging and subsequently compared to the intraoperative findings; from anterior to posterior are as follows (in a scheme similar to Goradia et al., [4]): Anterior Longitudinal Ligament (ALL), intervertebral disc, Posterior Longitudinal Ligament (PLL), Spinal Cord, Ligamentum Flavum and Interspinous soft tissues.
The ALL was evaluated intraoperatively in 15 patients of which 6 were found to be injured on the preoperative MR images out of the 9 that were injured on operative assessment. The remaining three were reported as false negative thus giving a sensitivity of 66.6%. Goradia et al., had reported a similar limited sensitivity (71%) for the anterior longitudinal ligament [4].
In contrast, of the 20 patients in whom the PLL was evaluated, 18 patients had an injury of which 17 were picked up by the initial MRI scan. There was one patient reported as false positive and false negative each. MRI was thus more sensitive in detecting injuries to the PLL at 94.4%. Other authors though have found that MRI was remarkable in regard to the anterior longitudinal ligament with 100% sensitivity and specificity and was just as highly specific but with a reduced sensitivity to 80% for the posterior longitudinal ligament [22].
The relatively lower sensitivity for the ALL in our study may be attributed to:
ALL, which is inherently difficult to accurately evaluate for integrity; and/or
Lowered bias when considering the ALL, as most patients were operated on basis of status of the disc rather than ALL injury alone [4].
The sensitivity of MRI in detecting injuries to the intervertebral disc was also on the higher side at 75%, with 9 out of 12 being detected on the MRI as it was in evaluating injuries to the spinal cord and conus medullaris with a high sensitivity at 93%.
However, when concerning the ligamentum flavum and the interspinous ligaments, the sensitivity of the MRI dropped to 62.5% and 63.6% respectively with a high number of false negatives in evaluating both these structures. The results of Zhuge et al., show 100% sensitivity for interspinous ligament, intervertebral disc, or paraspinal muscle injuries [22]. With regard to detecting ligamentum flavum injury, MRI showed moderate results for sensitivity (80%) and specificity (86.7%). Kliewer et al., correlated MR imaging findings with pathologic findings in 28 cadavers and found that MR imaging correctly identified 79% of ligament disruptions [12]. In this study, ALL and PLL injuries were detected in all 7 cases, but for the ligamentum flavum, facet capsules, and the interspinous tissues, there were 3 false-positives and 11 false-negatives. In a study by Emery et al., MR imaging detected ligament damage in 17 of 19 patients found to have injury at surgery and there were no false-positives [14].
Coming to imaging of the Spinal cord, MRI is considered as the modality of choice in evaluation of patients found to present with any neurological deficit. This is reiterated in a study that showed MRI to be very sensitive in detecting injuries to the cord [23]. Our study further strengthens this with a high sensitivity in detecting injuries to the cord (93%). Future research studies can utilize and assess the clinical applicability of advanced MR imaging in evaluation of spinal trauma [24].
Limitations
Our sample size was small owing to limited duration of study period and also due to exclusion of trauma patients due to various unavoidable reasons. We also had considerable verification bias as visualization of injuries depended on the operative approach. All the patients in whom a structure was deemed normal on imaging studies were not specifically evaluated surgically for confirmation of the same due to obvious ethical considerations. This important limitation prevented the calculation of MRI specificity. Since all the scans were performed using a low field strength magnet of 0.4T, a higher field strength MRI would have been more accurate in detecting injuries to both osseous and non-osseous structures. Conversely, even a low field strength MRI can be valuable tool, especially in areas where access to a high field strength MRI is limited.
Conclusion
MRI was found to be highly sensitive in detecting injuries to the spinal cord and the posterior longitudinal ligament and moderately sensitive for detection of disc injuries. On the other hand where the anterior longitudinal ligament, ligamentum flavum and the interspinous ligament are concerned, MRI performed ineffectively with higher number of false negative interpretations.
Hence to conclude, the utilization of MRI in assessing non-osseous injuries to the spine is well established and should be the modality of choice in evaluating spinal injuries, even when using low field strength magnets.
TR: Time to Repetition, TE: Time to Echo expressed in milliseconds, STIR: Short TI inversion recovery.