Candidal Infection of the Gingiva Mimicking Desquamative Gingivitis: A Case Report
Pallavi Samatha Yalamanchili1, Sushma Potluri2, Hemchand Surapaneni3, Md.Hafeez Basha4, Pavithra Davanapelly5
1 Reader, Department of Periodontics, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Gannavaram Mandal, Krishna, Andhra Pradesh, India.
2 Former Postgraduate, Department of Periodontics, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Gannavaram Mandal, Krishna, Andhra Pradesh, India.
3 Reader, Department of Prosthodontics, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Gannavaram Mandal, Krishna, Andhra Pradesh, India.
4 Post Graduate, Department of Periodontics, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Gannavaram Mandal, Krishna, Andhra Pradesh, India.
5 Former Post Graduate, Department of Periodontics, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Gannavaram Mandal, Krishna, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pallavi Samatha Yalamanchili, Lords Court, 501, D.No-59-3-1/1, Ashok Nagar, 2nd Lane, Vijayawada-520010, Andhra Pradesh, India. E-mail : pallavi_yalamanchili@yahoo.co.in
There has been an increase in the occurrence of fungal infections in humans in the recent years due to the discrete use of broad spectrum antibiotics and immunosuppressive therapies. The genus candida is the most frequently found fungi in humans. Candida albicans is a mucosal microbiota although it can cause infections which can be mucosal or life threatening infections in susceptible individuals. Candidiasis is the most common oral opportunistic fungal infection in humans. Candidiasis usually affects oral mucosa (buccal mucosa) and hard palate. Candidiasis affecting gingiva is not so common, but when it occurs, it is often misdiagnosed as desquamative gingivitis because of its clinical appearance. This paper discusses a case of Candidal infection of gingiva that mimics desquamative gingivitis.
Candida albicans, Clotrimazole, Diabetic, Fungal infection
Case Report
A 48-year-old female reported to Department of Periodontics and Implantology, Drs. Sudha & Nageswara Rao Siddhartha Institute of Dental Sciences, Chinaoutpalli, Andhra Pradesh with a chief complaint of swollen gums and burning sensation of gums on taking spicy food. Burning sensation was felt on the gingiva since one year. Medical history revealed that the patient was diabetic since two months and was under medication (insulin). On intraoral examination, the gingiva was erythematous and was peeling off [Table/Fig-1]. There was reduced salivary flow (xerostomia) and desquamation of the pseudomembrane was quite evident in maxillary arch and mandibular molar regions. Incisional biopsy was performed under local anesthesia (LIGNOX 2%- with adrenaline 1:80,000) in relation to 13, 14 (marginal gingiva and attached gingiva) [Table/Fig-2,3]. A provisional diagnosis of desquamative gingivitis was made. Patient was advised to use kenacort 0.1% twice daily, for a week. Routine lab investigations were done and all the tests were within the normal limits. HIV test had a negative result. Histopathological findings revealed the presence of Candidal hyphae and chronic inflammatory cells [Table/Fig-4]. A final diagnosis of Candidal infection (acute erythematous candidiasis) affecting the gingiva was made. Patient was advised to use candid mouth paint (clotrimazole) thrice daily along with antioxidants (Oxitard capsule once daily) and Limcee capsules (Vitamin C supplements). The patient was reviewed every three months until a year. Within the review period, the clinical features of gingiva were normal and the burning sensation had completely subsided [Table/Fig-5].
Peeling of gingival epithelium.



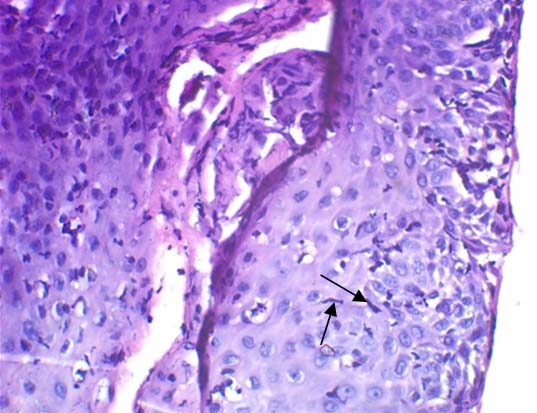
Connective tissue with dense collagen bundles, moderate amount of inflammatory cell infiltrate and dilated capillaries appearing as Candidal hypae. The arrows indicate thin filamentous structures appearing as Candidal hypae.

Discussion
In recent years, there has been a significant increase in fungal infections. Most of the fungal infections are superficial, affecting the skin, hair, nails and mucosa but can also be systemic, involving major body organs. Members of the genus Candida are amongst the most frequently recovered from disease. Candidiasis is the most common oral fungal infection in humans [1]. Candida albicans (C.albicans) is a commensal found to cause oral candidiasis with an incidence rate of about 20% in normal population [2]. The other non-albicans species such as C. glabrata, C. tropicalis, C. guellermondii, C. krusei are also pathogenic. C. albicans is a fungus that can grow in a number of morphological forms ranging from yeast to hyphae [3]. Pseudohyphal forms are also seen [4]. Odds stated that hyphal form is invasive and pathogenic, while the yeast form is the commensal non-pathogenic form [5]. Candidal hyphae are highly adherent and are resistant to phagocytosis [6]. Innate defense mechanisms play an important role in preventing yeast colonization of the oral cavity [7]. The first line of defense mechanisms are the epithelial barrier, antimicrobial peptide, defensin with an antimicroial activity [8], secretory IgA (assists in clearance), salivary flow rate and specific salivary enzymes like lysozyme [9], histatins [10] and lactoferrin [11] having candididal properties. Candidiasis is an opportunistic infection which occurs in immunocompromised individuals. The predisposing factors allow the Candida albicans to selectively express virulent factors to cause manifestations clinically. The patient was diabetic which was an important factor that altered the patient’s host immune response and allowed multiplication of candida. Several virulence factors of C.albicans such as adherence to host cells via mannoprotein of its cell wall have immunosuppressive properties and co-aggregation with Streptococcus mutans plays an important role in its colonization. Interference of host immune system begins with epithelial penetration of sIgA by hyphae and supported by aspartate proteinase and phospholipase resulting in reduced salivary flow [12]. Oral candidiasis has many distinct primary forms. Most common clinical entity is pseudomembranous candidiasis (oral thrush). Other forms include chronic erythematous candidiasis and chronic hyperplastic candidiasis. Candidiasis is not commonly seen in the gingiva of healthy individuals but when affected it is usually manifested as erythematous gingiva with a granular surface. It is often misdiagnosed as Desquamative gingivitis. The histopathologic changes include inflammatory cell infiltration of epithelium and connective tissue, intraepithelial microabscesses, epithelial intracellular oedema and epithelial atrophy, hyperplasia and dysplasia [13]. The reduced salivary flow and desquamated epithelium is the cause for burning sensation of mouth. Antifungal agents are used to treat oral candidiasis. Patient was advised to apply candid mouth paint topically over the lesion thrice daily, which contains clotrimazole as chief content. Clotrimazole acts by killing candida by altering the permeability of the cell wall and it inhibits the biosynthesis of ergosterol and other sterols required for cell membrane production by binding to the phospholipids in the cell membrane. This leads to the cell’s death via loss of intracellular substances. To our knowledge, this was the first case where candidiasis of gingiva was reported.
Conclusion
Candidal infection of gingiva is rare, but when affected, mimicks desquamative gingivitis. Local and systemic predisposing factors favor the colonization of the hyphae resulting in manifestations of candidiasis. The host’s defense mechanism also plays an important role in the occurrence of Candidal infection.
[1]. Ellepola ANB, Oral candidosis: a brief overviewBulletin of the Kuwait Institute for medical specialization 2005 4:17-24. [Google Scholar]
[2]. Abu-Elteen KH, Hamad MA, Salah SA, Prevalence of Oral Candida. Infections in Diabetic PatientsBahrain Medical Bulletin 2006 28:1-8. [Google Scholar]
[3]. Nasution AI, Virulence factor and pathogenicity of candida albicans in oral candidiasisWorld journal of dentistry 2013 4:267-71. [Google Scholar]
[4]. Odds FC, Candida and candidosis 1988 2nd editionLondonbailliere tindall [Google Scholar]
[5]. Odds FC, Candida species and virulenceASM News 1994 60:313-18. [Google Scholar]
[6]. Williams DW, Kuriyama T, Silva S, Malic S, Lewis MA, Candida biofilms and oral candidosis: treatment and preventionPeriodontol 2000 2011 55:250-65. [Google Scholar]
[7]. Cannon RD, Holmes AR, Mason AB, Monk BC, Oral Candida: clearance, colonization, or candidiasis?J Dent Res 1995 74:1152-61. [Google Scholar]
[8]. Schonwetter BS, Stolenberg ED, Zasloff MA, Epithelial antibiotics induced at sites of inflammationScience 1995 267:1645-48. [Google Scholar]
[9]. Togbi RS, Samaranayake LP, MacFarlane TW, Invitro susceptibility of candida species to lysozymeOral Microbial Immunol 1988 3:35-9. [Google Scholar]
[10]. Lal K, Santarpia RP, Xu L, Manssuri F, Pollock JJ, One step purification of histidine-rich polypeptides from human parotid saliva and determination of anti-Candidal activityOral Microbial Immunol 1992 7:44-50. [Google Scholar]
[11]. Nikawa H, Samaranayake LP, Tenovuo J, The fungicidal effect of human lactoferrin on candida albicans and candida kruseiArch Oral Biol 1993 38:1057-63. [Google Scholar]
[12]. Ashman RB, Papadimitriou JM, Production and function of cytokines in natural and acquired immunity to candida albicans infectionMicrobiol Rev 1995 59:646-72. [Google Scholar]
[13]. Odden K, Schenck K, Koppang H, Hurlen B, Candida infection of the gingival in HIV-infected personsJ Oral Pathol Med 1994 23:178-83. [Google Scholar]