Antisynthetase Syndrome: A Rare Cause for ILD
HJ Gayathri Devi1, MD Majeed Pasha2, Mantha Sathya Padmaja3, Sujith Halappa4
1 Associate Professor, Department of Respiratory Medicine, MS Ramaiah Medical College, Bangalore, India.
2 Resident, Department of Respiratory Medicine, MS Ramaiah Medical College, Bangalore, India.
3 Resident, Department of Respiratory Medicine, MS Ramaiah Medical College, Bangalore, India.
4 Resident, Department of Respiratory Medicine, MS Ramaiah Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. HJ Gayathri Devi, Associate Professor, Department of Respiratory Medicine, MS Ramaiah Medical College, Bangalore – 560 054, India.
E-mail: gayathrijoshy@gmail.com
Anti-Synthetase Syndrome (ASS) is a rare autoimmune disorder characterized by Interstitial Lung Disease (ILD), inflammatory myositis, fever, Raynaud’s phenomenon, mechanic’s hand, and inflammatory polyarthritis in the setting of antibodies against amino acyl-transfer RNA synthetases, with anti-Jo-1 antibody being the most common. It can sometimes present as interstitial lung disease without any other expression of the syndrome. Clinical and radiological features can be similar to atypical pneumonia and could be a challenge to diagnose at an early stage. Prognosis is generally poor, especially when there is associated ILD and delay in diagnosis can lead to increase in morbidity due to progression of pulmonary involvement. We report a patient of ASS presenting with ILD, diagnosed early and treated successfully with immunosupression.
Anti-jo-1, Cryptogenic, Organizing, Pneumonia
Case Report
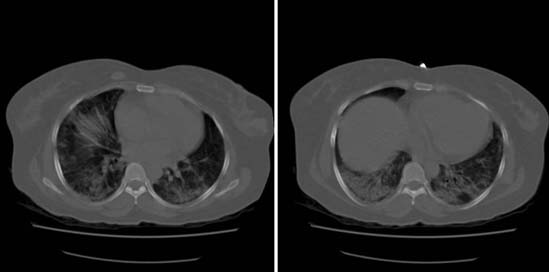
A 35-year-old female presented to the Pulmonology department with cough, progressive breathlessness and fever. She denied any previous respiratory illness, swelling of the joints, muscle weakness or skin rashes. Initial vital signs were 99°F, RR 22, BP 126/90 and room air oxygen saturation of 80%. Respiratory system examination showed occasional crepitations in the left infrascapular region. Other systemic examination were unremarkable. Laboratory evaluation showed total leucocyte count (TLC) 14,050 slightly elevated liver enzymes, renal function test and urine routine were normal. A 2D Echocardiogram was normal. Chest x-ray showed parenchymal haziness in both the lung fields [Table/Fig-1]. Patient was started on Injection Piperacillin+Tazobactum and Clarithromycin with the provisional diagnosis of bilateral bronchopneumonia. Patient continued to have persistent breathlessness and desaturation with no new findings on respiratory system examination. She also complained of polyarthralgia during the course of her hospital stay, which lead us to investigate further to look for other causes of radiological abnormality. Contrast enhanced computerised tomography (CECT) thorax revealed bilateral airspace opacities mainly basal region suggestive of cryptogenic organizing pneumonia [Table/Fig-2a,b]. Screening of the patient for systemic disorder was done because of non responsiveness to broadspectrum antibiotics. Spirometry showed restrictive pattern and Diffusion Capacity of Lungs for Carbon Monoxide (DLCO) was reduced. Upper gastrointestinal endoscopy was normal. Serum Creatine Phosphokinase (CPK) and complements were normal. Rheumatoid factor and anti neutrophil cytoplasmic antibodies were not detected. Muscle biopsy and skin biopsy were not done in view of the paucity of symptoms with normal CPK value. C-reactive protein (CRP) was elevated 6.24(<0.5 mg /dl). Antinuclear antibody profile showed anti-jo1 +++, and RO 52 +. The positive titre of anti-jo-1 antibodies supported the diagnosis of antisynthetase syndrome with an interstitial lung disease.
Chest X-ray showing bilateral non-homogeneous opacities.

CT Thorax showing bilateral alveolar opacities mainly in the basal region with air bronchogram.
The patient was started on high dose of intravenous methylprednisolone 500 mg twice a day for three days. On Day-2 of treatment patient showed dramatic improvement in her symptoms. The oxygen saturation also improved and we could move her out of the high dependency unit. She has received six cycles of 500 mg of cyclophosphamide. She is on oral methylprednisolone 4mg once daily and azathioprine 50mg once daily. Follow-up X-ray showed clearance of the opacities [Table/Fig-3].
Chest X-ray showing good clearance of the opacities.

Discussion
The Anti-Synthetase Syndrome (ASS) is a rare, systemic autoimmune disease involving multiple organs. The presence of anti-aminoacyl t-RNA antibodies (anti-ARS antibodies) especially anti-Jo-1 antibody is the hallmark of the disease [1].
Antisynthetase syndrome was first described by Marguerie and coworkers in 1990. It was described as a triad of polymyositis,diffuse interstitial lung disease and serum autoantibodies to aminoacyl transfer RNA synthetase (anti-ARS) [2]. The pathogenesis of antisynthetase syndrome involves autoantibodies to eight of the aminoacyl–transfer RNA synthetases. In ASS, 68-87% of the anti-ARS consists of anti-jo-1 antibody [3]. Seven other anti-ARS identified are rarely seen. Anti SSA autoantibodies and anti-Ro 52 are frequently seen in anti–ARS positive patients [4]. ASS is characterized by varying degrees of interstitial lung disease, myositis, arthropathy, fever, Raynaud’s phenomenon and mechanic’s hands [5]. Key features for the diagnosis of ASS include the presence of an Anti-ARS antibody, accompanied by myositis, ILD or both [1]. ASS is a rare disease seen mainly in the age group of 43 to 60 years. A female dominance has been reported in most series [1]. Lung involvement may occur in the absence of muscle involvement [6]. Our patient did not have any features suggestive of myositis. The major determinant of morbidity and mortality in ASS is ILD [7]. Lung involvement in the form of interstitial lung disease is found in more than 60% of the patients and is a major cause of morbidity [8]. Surgical lung biopsies in antisynthetase syndrome presenting as ILD may show different histologic features like non-specific interstitial pneumonia, diffuse alveolar damage, usual interstitial pneumonia or cryptogenic organizing pneumonia [9]. However, lung biopsy is not recommended as a routine procedure in the evaluation of antisynthetase syndrome [6].
Prednisone in the dose of 1mg/kg/day remains the drug of choice for the treatment of this disorder. High dose of steroid is used in the initial phase. Remission is achieved in 25-68% of cases when high dose of corticosteroids are given as part of initial therapy [10]. Studies have found a better response to steroid therapy in patients with Non-Specific Interstitial Pneumonia (NSIP) and Cryptogenic Organizing Pneumonia (COP) when compared to those with Usual interstitial pneumonia (UIP) [11]. Monthly IV pulse therapy with cyclophosphamide has shown to be effective when ILD is prominent. Steroid sparing agents azathioprine, methotrexate and cyclosporine have been used with low to moderate success [11]. Mycophenolate mofetil has been used in anti-jo-1 positive patients with refractory ILD with improvement of ILD. In some series Rituximab has been used with moderate success in patients with worsening of the ILD despite aggressive conventional treatment. However, prospective studies are needed to assess the safety issues of Rituximab [7]. The dermatologic manifestations are treated with hydroxychloroquine. ILD is the major determinant of morbidity and mortality in Antisynthetase syndrome. The course of the disease is usually chronic and associated with decreased survival. Progression of the ILD is the main prognostic factor. Possible predictors of poor outcome of ILD are older age, symptomatic ILD, UIP pattern in high resolution CT thorax, lower values of FVC and DLCO at the time of diagnosis and steroid refractory ILD [11]. The knowledge about the course is limited because of paucity of large scale studies of this rare disease.
Conclusion
This case shows the importance of considering an alternative diagnosis when there is no response to standard antibiotic regimens for suspected infectious pneumonia. Early diagnosis and prompt institution of appropriate therapy can prevent disease progression and improve patient outcome as in our patient.
[1]. Solomon J, Swigris JJ, Brown KK, Myositis-related interstitial lung disease and antisynthetase syndromeJornalbrasileiro de pneumologia :publicacaooficial da SociedadeBrasileira de Pneumologia e Tisilogia 2011 37(1):100-09. [Google Scholar]
[2]. Marguerie C, Bunn CC, Beynon HL, Bernstein RM, Hughes JM, So AK, Polymyositis, pulmonary fibrosis and autoantibodies to aminoacyl-tRNAsynthetase enzymesQ J Med 1990 77:1019-38. [Google Scholar]
[3]. Jan Tore Gran and ØyvindMolberg (2011). The Antisynthetase Syndrome, Idiopathic Inflammatory Myopathies - Recent Developments, Prof. Jan Tore Gran (Ed.), ISBN: 978-953-307-694-2, InTech, Available from: http://www.intechopen.com/books/idiopathic-inflammatory-myopathies-recent-developments/theantisynthetase-syndrome [Google Scholar]
[4]. Vancsa A, Csipo I, Nemeth J, Devenyi K, Gergely L, Danko K, Characteristics of interstitial lung disease in SS-A positive/Jo-1 positive inflammatory myopathy patientsRheumatol Int 2009 29(9):989-94. [Google Scholar]
[5]. Katzap E, Barilla-LaBarca ML, Marder G, Antisynthetase syndromeCurrRheumatol Rep 2011 13:175-181. [Google Scholar]
[6]. Tillie-Leblond I, Wislez M, Valeyre D, Interstitial lung disease and anti-Jo-1 antibodies: difference between acute and gradual onsetThorax 2008 63:53-9. [Google Scholar]
[7]. Sem M, Molberg O, Lund MB, Gran JT, Rituximab treatment of the anti-synthetase syndrome: a retrospective case seriesRheumatology. (Oxford) 2009 48(8):968-71. [Google Scholar]
[8]. Marie I, Hatron PY, Hachulla E, Wallaert B, Michon-Pasturel U, Devulder B, Pulmonary involvement in polymyositis and in dermatomyositisJ Rheumatol 1998 25(7):1336-43. [Google Scholar]
[9]. Yousem SA, Gibson K, Kaminski N, Oddis CV, Ascherman DP, The pulmonary histopathologic manifestations of the anti-Jo-1 tRNAsynthetase syndromeMod Pathol 2010 23(6):874-80. [Google Scholar]
[10]. Tzioufas AG, "Antisynthetase syndrome,"Orphanet Encyclopediahttp://www.orpha.net/data/patho/GB/uk-antisynthetase.pdf, Nov. 2001, pp. 1-5 [Google Scholar]
[11]. Marie I, Josse S, Hatron PY, Dominique S, Hachulla E, Janvresse A, Interstitial Lung Disease in Anti–Jo-1 Patients WithAntisynthetase SyndromeArthritis Care Res 2013 65:800-08. [Google Scholar]