Neutrophil–Lymphocyte Ratio in Patients with Adenoidectomy
Serhan Derin1, Selvet Erdogan2, Murat Sahan3, Hatice Topal4, Hamdi Sozen5
1 Faculty, Department of Otorhinolaryngology, Mugla Sitki Kocman University, School of Medicine, Mugla/Turkey.
2 ENT Clinic, Kocaeli University, Medical Faculty, Kocaeli, Turkey.
3 Faculty, Department of Otorhinolaryngology, Mugla Sitki Kocman University, School of Medicine, Mugla/Turkey.
4 Faculty, Department of Peadiatrics, Mugla Sitki Kocman University, School of Medicine, Mugla, Turkey.
5 Faculty, Department of Infectious Disease, Mugla Sitki Kocman University, School of Medicine, Mugla/Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Selvet Erdogan, Kocaeli Üniversitesi, Tıp Fakültesi, Kulak Burun Bogaz ABD, Kocaeli, Türkiye.
E-mail: sel-erdogan@hotmail.com
Introduction
Obstructive Sleep Apnea syndrome (OSA) is the most serious consequence of adenoid hypertrophy (AH) and it is one of the most common reasons of nocturnal hypoxia in children. There is some information about the relationship between childhood OSA and atherosclerosis or cardiac diseases. In this study, we evaluated the relationship between, neutrophil-lymphocyte ratio (NLR) and AH which is the most frequent cause leading OSA in children.
Aim
Thus we aimed to contribute about subject of preoperative and postoperative NLR values in patients undergoing adenoidectomy that there is limited information.
Materials and Methods
The study group comprised 76 children undergoing adenoidectomy. A preoperative and 3rd-month postoperative complete blood cell count was performed to calculate the NLR values in all patients. The NLR values were calculated as the ratio of neutrophils to lymphocytes in peripheral blood. Data analysis was performed using SPSS 15.
Results
The mean NLR (min - max) was 1.0 (0.16-3.57) preoperatively and 1.06 (0.35-4.95) 3 months postoperatively (p = 0.052> 0.05). Haemoglobin 12.9 ± 0.95 (preop) 12.94 ± 0.91 (postop) (p= 0.522), WBC (min-max) 7.75 (3.90-14.99) 7.8 (4-15.64) (p= 0.297 <0.005), platelet 344.5 ± 98.7 328.4 ± 68.9 (p<0,005).
Conclusion
There is limited information in the English literature. This study has investigated the association between the NLR and adenoidectomy. The results of the present study demonstrate that the NLR is not a statistically significant inflammatory factor. So, NLR values do not appear related to stage of upper airway obstruction.
Adenoid hypertrophy, Inflammatory markers, Obstructive sleep apnea syndrome
Introduction
Adenoid Hypertrophy (AH) leads to upper airway obstruction and this situation cause alveolar hypoventilation, which may result in chronic hypoxia and hypercarbia. Chronic hypoxia may lead to pulmonary arterial hypertension, cor pulmonale and finally decompensated heart failure. These destructive outcomes were found to be reversible with adenoidectomy, which increased the importance of the treatment [1]. Systemic inflammatory markers and pro-inflammatory cytokines are increased in these children and promote lymphoid tissue proliferation [2]. Low-level systemic inflammation and oxidative stress are related to OSA [3]. Systemic inflammatory changes that are associated with sleep disorders can be demonstrated by evaluating the levels of inflammatory markers in the blood. A high white blood cell count is positively associated with inflammation, particularly in patients with cardiovascular disease [4]. The neutrophil–lymphocyte ratio (NLR), which involves measurement of a subgroup of white blood cells, has been identified as a new marker of inflammation [5]. Many studies have shown that the NLR is an important predictor of vascular diseases such as coronary artery disease, acute coronary syndromes, heart failure, and diabetic nephropathy [4,6–9]. But there is limited information in patient who has AH.
Aim
In this study, we evaluated the relationship between preoperative and postoperative inflammation using the serum NLR values in patients undergoing adenoidectomy and estimated whether the NLR values can be used as an inflammation marker supporting operation for patients with adenoid hypertrophy.
Materials and Methods
The research protocol was submitted and approved by the Mugla Sitki Kocman University Ethics Committee and was conducted in accordance with the ethical regulations of the Declaration of Helsinki. Informed consent was provided by the parents of all of the patients.
Study Population
Seventy six children (38 girls and 38 boys, mean age 6.4 ±2.41) who underwent adenoidectomy in our hospital from August 2011 to December 2014 were included in this study. In addition to routine ear, nose, and throat (ENT) physical examination, transnasal nasopharyngeal endoscopy was performed on all of the patients to determine the size of the adenoids. Patients who could not tolerate the endoscopic examination underwent plain lateral X-rays of the nasopharynx. Patients who met the following criteria were included:
1. Children without chronic diseases such as diabetes mellitus, hepatic or renal disease, chronic heart disease, haematological disease, thrombocytopaenia, hypothyroidism or hyperthyroidism, bronchial asthma, obesity (those with a body mass index greater than the 95th percentile by age and sex), use of antithrombotic medication, an intraoperative bleeding volume > 50 mL, and postoperative bleeding
2. Children who exhibited open-mouth breathing, snoring, sleep apnea, difficulty swallowing, and lack of appetite
3. Children with adenoid hypertrophy characterized by > 50% nasopharyngeal obstruction without other causes of nasal obstruction such as turbinate hypertrophy, allergic rhinitis, septal deviation, or anatomic deformities.
Adenoidectomy was performed on all patients using the same surgical technique and by the same surgeon. Preoperative and 3rd-month postoperative haemograms were obtained, and the preoperative and postoperative NLRs were compared.
Laboratory Analysis
Blood samples were drawn from the antecubital vein, and collected in ethylene diamine tetra acetic acid (EDTA) containing tubes. Blood samples were drawn from 08:30 a.m to 10:00 a.m in fasting patients and laboratory analyses were conducted on the same day until 14:00. Haemogram analysis was performed on a Beckman Coulter LH 780 Haematology Analyser (Beckman Coulter Inc., Miami, FL, USA).
Statistical Analysis
Data analysis was performed using SPSS for Windows, version 15.0 (SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was used to test the normality of distribution of the continuous variables and preoperative- postoperative changes and then, homogeneity test was performed. Numerical variables with normal distribution are expressed as sample size and mean values with standard deviation and if not normal distribution, median (minimum-maximum). The comparison of mean of quantitative variables with normal distribution was compared to a paired-samples t-test. If they are not normal distribution, Wilcoxon test used. The p-value < 0.05 was considered statistically significant.
Results
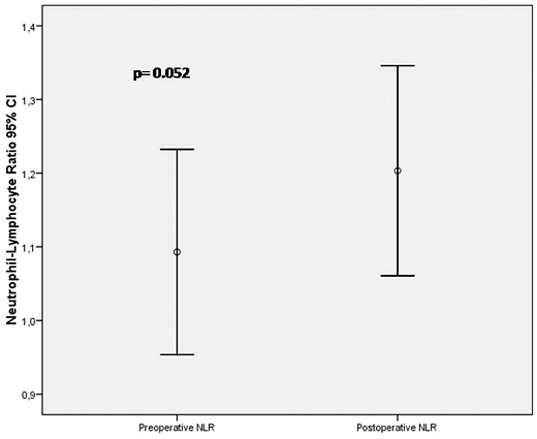
This study included 76 paediatric patients (38 boys, 38 girls). Their mean age was 6.4 ± 2.41 years (range, 2–12 year). The preoperative and 3-month postoperative NLRs were 1.0 (0.16-3.57) and 1.06 (0.35-4.95) respectively, with no statistically significant difference (Wilcoxon test, p = 0.052 > 0.05) [Table/Fig-1]. Haemoglobin 12.9 ± 0.95 (preop) 12.94 ± 0.91 (postop) (p=0.522), WBC 7.75 (3.90-14.99) 7.8 (4-15.64) (p=0.297), platelet (x103) 344.5 ± 98.7, 328.4 ± 68.9 (p=0.15) [Table/Fig-2].
The pre- and postoperative neutrophil-lymphocyte ratios for the patients.
Pre- and postoperative calculated parameters.
| Preop | Postop | p |
|---|
| Hb | 12.9 ± 0.95 | 12.94 ± 0.91 | 0.522 |
| Haematocrit | 38.25 ± 2.68 | 38.93 ± 2.50 | 0.012 |
| *WBC | 7.75 (3.90-14.99) | 7.8 (4-15.64) | 0.297 |
| Platelet (x103) | 344.5 ± 98.7 | 328.4 ± 68.9 | 0.15 |
| *MPV | 7.80 (6.40-11.40) | 8.10 (6.40-10.70) | <0.001 |
| *NLR | 1.0 (0.16-3.57) | 1.06 (0.35-4.95) | 0.052 |
* Numerical values areexpressed as median (min-max), because distribution is not normal.
Discussion
Adenoidectomy is one of the most common procedure performed by otolaryngologists worldwide. The operation increases patient’s quality of life if performed for the appropriate indications. Adenoid hypertrophy can cause snoring, sleeping with open-mouth breathing and sleep apnea episodes. If not treated, in the long run, adenoid hypertrophy causes nocturnal hypoxia and is the most frequent cause of obstructive sleep apnea in children [10,11].
Thus, control of excess adenoid tissue, especially if its presence causes snoring and sleep apnea will minimize secondary inflammatory processes and inflammatory factors will decline. In time, this could play an important role in modulating the risk for illnesses associated with the development of atherosclerosis such as coronary artery disease and ischemia.
Important arguments originated in adults openly contain sleep-disordered breathing as a contributing risk factor for cardiovascular diseases such as hypertension, ischemic heart disease, and cerebrovascular accidents [12–14]. Intermittent hypoxia and sleep fragmentation have been demonstrated that cause inflammatory and oxidative responses. Thus, in time, inflammatory biomarkers increase and lead to secondary cardiovascular disease. Although the exact mechanism underlying these health problems remain unclear, chronic inflammation has been implicated in their pathogenesis [3]. Identification of inflammatory factors that in patients with OSAS can help us to estimate the risk of accompanying disease and violence in the future.
A number of studies have examined the relationship between prognosis and NLR as a marker of inflammation. The clinical value of NLR has been studied in patients with cardiovascular disease, chronic renal disease, malignancies, osteoporosis, and Alzheimer’s disease [7,15–21]. The clinical value of NLR, however are limited to the field of ENT medicine. The basic area of study in the ENT field is the relationship between the NLR and the prognosis of Bell’s Palsy, sudden hearing loss, and vertigo [22–24].
There is only one study about association of NLR values and adenoidectomy [25]. Our main finding (like the other paper) is the absence of a correlation between the preoperative and postoperative NLR. With this study, we compared pre and postoperative NLR values, and we observed that adenoidectomy do not cause a significant changes in NLR levels.
Limitation
The main limitation of our study is the small number of patients investigated. Another limitation is that we did not perform polysomnographic studies in our patients. Polysomnography (PSG) is standard diagnostic test to determine the presence and severity of OSA. Because of lack of a formal sleep laboratory, PSG studies were not performed for any of the patients before or after the operation. However, this is the first report on the pre- and post-adenoidectomy NLR in the English language. Future studies with larger groups and performed PSG will be beneficial.
Conclusion
Only one study has investigated the association between the pre- and post-adenoidectomy NLR. Our results demonstrated that the NLR is not significantly different before and after adenoidectomy. NLR cannot be considered as useful diagnostic and prognostic parameters in clinical practice in patients with adenoid hypertrophy with OSAS. However, these findings should be confirmed by additional studies involving larger numbers of patients.
* Numerical values areexpressed as median (min-max), because distribution is not normal.
[1]. Abdel-Aziz M, Asymptomatic cardiopulmonary changes caused by adenoid hypertrophyJ Craniofac Surg 2011 22:1401-03. [Google Scholar]
[2]. Kim J, Bhattacharjee R, Dayyat E, Snow AB, Kheirandish-Gozal L, Goldman JL, Increased cellular proliferation and inflammatory cytokines in tonsils derived from children with obstructive sleep apneaPaediatr Res 2009 66:423-28. [Google Scholar]
[3]. Korkmaz M, Korkmaz H, Küçüker F, Ayyıldız SN, Çankaya S, Evaluation of the association of sleep apnea-related systemic inflammation with CRP, ESR, and neutrophil-to-lymphocyte ratioMed Sci Monit 2015 21:477-81. [Google Scholar]
[4]. Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, Intermountain Heart Collaborative Study Group. Which white blood cell subtypes predict increased cardiovascular risk?J Am Coll Cardiol 2005 10:1638-43. [Google Scholar]
[5]. Zahorec R, Ratio of neutrophil to lymphocyte counts - rapid and simple parameter of systemic inflammation and stress in critically illBratisl Lek Listy 2001 102:5-14. [Google Scholar]
[6]. Gibson PH, Croal BL, Cuthbertson BH, Small GR, Ifezulike AI, Gibson G, Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass graftingAm Heart J 2007 154:995-1002. [Google Scholar]
[7]. Núñez J, Núñez E, Bodí V, Sanchis J, Miñana G, Mainar L, Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarctionAm J Cardiol 2008 101:747-52. [Google Scholar]
[8]. Rudiger A, Burckhardt OA, Harpes P, Muller SA, Follath F, The relative lymphocyte count on hospital admission is a risk factor for long-term mortality in patients with acute heart failureAm J Emerg Med 2006 24:451-54. [Google Scholar]
[9]. Huang W, Huang J, Liu Q, Lin F, He Z, Zeng Z, Neutrophil-lymphocyte ratio is a reliable predictive marker for early-stage diabetic nephropathyClin Endocrinol (Oxf) 2015 82:229-33. [Google Scholar]
[10]. Izu SC, Itamoto CH, Pradella-Hallinan M, Pizarro GU, Tufik S, Pignatari S, Obstructive sleep apnea syndrome (OSAS) in mouth breathing childrenBraz J Otorhinolaryngol 2010 76:552-56. [Google Scholar]
[11]. Muzumdar HV, Sin S, Nikova M, Gates G, Kim D, Arens R, Changes in heart rate variability after adenotonsillectomy in children with obstructive sleep apneaChest 2011 139:1050-59. [Google Scholar]
[12]. Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart HealthJAMA 2000 283:1829-36. [Google Scholar]
[13]. Peppard PE, Young T, Palta M, Skatrud J, Prospective study of the association between sleep- disordered breathing and hypertensionN Engl J Med 2000 342:1378-84. [Google Scholar]
[14]. Mooe T, Franklin KA, Holmstrom K, Rabben T, Wiklund U, Sleep-disordered breathing and coronary artery disease: long-term prognosisAm J Respir Crit Care Med 2001 164:1910-13. [Google Scholar]
[15]. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E, Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancerJ Thorac Cardiovasc Surg 2009 137:425-28. [Google Scholar]
[16]. Cedrés S, Torrejon D, Martínez A, Martinez P, Navarro A, Zamora E, Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancerClin Transl Oncol 2012 14:864-69. [Google Scholar]
[17]. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ, Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancerJ Surg Oncol 2005 91:181-84. [Google Scholar]
[18]. Halazun KJ, Aldoori A, Malik HZ, Al-Mukhtar A, Prasad KR, Toogood GJ, Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastasesEur J Surg Oncol 2008 34:55-60. [Google Scholar]
[19]. Duffy BK, Gurm HS, Rajagopal V, Gupta R, Ellis SG, Bhatt DL, Usefulness of an elevated neutrophil to lymphocyte ratio in predicting long-term mortality after percutaneous coronary interventionAm J Cardiol 2006 97:993-96. [Google Scholar]
[20]. Ahsen A, Ulu MS, Yuksel S, Demir K, Uysal M, Erdogan M, As a new inflammatory marker for familial Mediterranean fever: Neutrophil-to-lymphocyte ratioInflammation 2013 36:1357-62. [Google Scholar]
[21]. Turkmen K, Erdur FM, Ozcicek F, Ozcicek A, Akbas EM, Ozbicer A, Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patientsHaemodial Int 2013 17:391-96. [Google Scholar]
[22]. Özler GS, Increased neutrophil-lymphocyte ratio in patients with idiopathic sudden sensorineural hearing lossJ Craniofac Surg 2014 25:260-63. [Google Scholar]
[23]. Ozbay I, Kahraman C, Balikci HH, Kucur C, Kahraman NK, Ozkaya DP, Neutrophil-to-lymphocyte ratio in patients with peripheral vertigo: A prospective controlled clinical studyAm J Otolaryngol 2014 6:699-702. [Google Scholar]
[24]. Bucak A, Ulu S, Oruc S, Yucedag F, Tekin MS, Karakaya F, Neutrophil-to-lymphocyte ratio as a novel-potential marker for predicting prognosis of Bell palsyLaryngoscope 2014 124:1678-81. [Google Scholar]
[25]. Yenigun A, The efficacy of tonsillectomy in chronic tonsillitis patients as demonstrated by the neutrophil-to-lymphocyte ratioJ Laryngol Otol 2015 20:1-6. [Google Scholar]