A Fatal Case of Acute Myeloid Leukaemia—Methotrexate Related or Primary Autoimmune Disease Related: A Rare Case Report
Saurabh Agarwal1, Nidhi Kaeley2, Priyanka Gupta3, Vibha Gupta4, Rohan Bhatia5
1 Assistant Professor, Department of Medicine, Himalayan Institute of Medical Sciences, SRHU, Jolly Grant, Dehradun, Uttarakhand, India.
2 Assistant Professor, Department of Medicine, Himalayan Institute of Medical Sciences, SRHU, Jolly Grant, Dehradun, Uttarakhand, India.
3 Senior Resident, Department of Microbiology, Himalayan Institute of Medical Sciences, SRHU, Jolly Grant, Dehradun, Uttarakhand, India.
4 Assistant Professor, Department of Pathology, Himalayan Institute of Medical Sciences, SRHU, Jolly Grant, Dehradun, Uttarakhand, India.
5 Assistant Professor, Department of Anaesthesia, Himalayan Institute of Medical Sciences, SRHU, Jolly Grant, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priyanka Gupta, Senior Resident, Department of Microbiology, HIMS, SRHU, Jolly Grant, Dehradun, India.
E-mail: dr.priyankagupta60@yahoo.com
Methotrexate is being used for many years in the treatment of chronic medical disorders e.g. rheumatoid arthritis since 1951. It has been associated with various systemic toxicities and complications including bone marrow suppression and lymphomas. The development of leukaemia in a patient of chronic rheumatoid arthritis is either related with the primary disease or due to the drugs which are used in the treatment like cyclophosphamide. In our present case, a 70-year-old female who was a known case of Rheumatoid Arthritis (RA) and was on methotrexate once a week orally for the past 20 years presented with complaints of loss of appetite, loss of weight and anaemia since 2 months. After thorough examination and investigation, she was diagnosed with acute myeloid leukaemia (AML-M4) with bilateral chest consolidation.
Bone marrow suppression, Chest consolidation, Rheumatoid arthritis, Systemic toxicities
Case Report
A 70-year-old female presented to the Department of Medicine with complaints of loss of appetite and loss of weight and anaemia since 2 months. She was also seeking medication from some private practitioner for a long time for her condition. She was a known case of Rheumatoid Arthritis for which she was on Methotrexate 10 mg, once a week orally for the past 20 years.
On general examination patient was conscious, oriented and afebrile. Her blood pressure was 140/70 mm Hg and pulse rate was 82 beats/minutes. Her random blood sugar was 198mg/dl.
She had pallor with no icterus, cyanosis and clubbing. On further examination, she had bilateral axillary lymphadenopathy. Lymph nodes were firm and mobile, measuring around 2x2cm which was also confirmed on chest X-ray. Bilateral pedal oedema was present. Central nervous examination and central venous examination was normal. On respiratory examination, basal crepitations were heard on the right side of chest. During per abdominal examination hepatosplenomegaly was found which was soft and non-tender.
On investigation her haemoglobin was 8.31g/dl. Total leukocyte count was raised i.e. 59.51 thousand/cubic mm. Differential leukocyte count showed neutrophil -19%, lymphocyte -13%, Promyelocyte-3%, Myelocyte-12%, Metamyelocyte-4%, Blast cells-42%, Eosinophil-6%. Her platelet count was 97.6 thousand/cubic mm. Her Mean corpuscular haemoglobin was 34.8 pg, Mean corpuscular volume was 104.4 fl, Mean corpuscular haemoglobin concentration was 33.43%. Her packed cell volume was 97.6%. Liver function tests, Serum electrolytes, kidney function tests, Thyroid function tests and creatinine phosphokinase-MB were in normal range. Rheumatoid factor was positive i.e. 75 IU/ml and anti CCP antibody was 200 and antinuclear antibodies was negative.
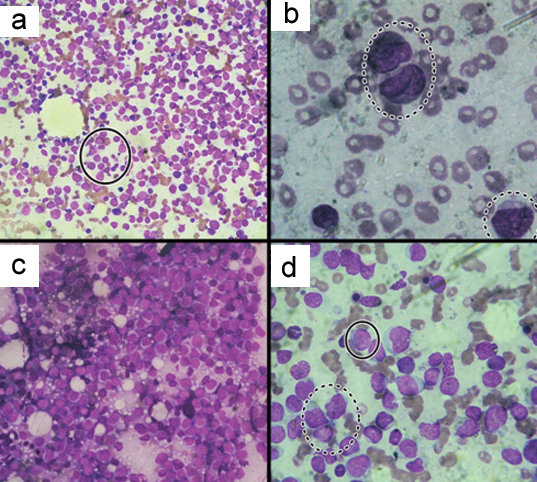
On further investigations: Chest X-ray (PA view) showed cardiomegaly with bilateral lung consolidation [Table/Fig-1]. On ultrasound abdomen hepatomegaly with periportal lymphadenopathy was seen. Her Bone marrow examination revealed hypercellular, infiltration with blasts having morphology suggesting of AML-M4 (Myelomonocytic type) which on Peripheral blood smear showed Acute leukaemia [Table/Fig-2]. Patient was managed conservatively with intravenous fluids and antibiotics but 4 days later she died.
Chest x-ray (PA view) showing bilateral consolidation and cardiomegaly.

a) Bone marrow aspirate Myeloblast and monoblast (inside circle) (magnification 100X). b) Bone marrow aspirate: Promyelocytes (inside larger circle) and myeloblast (inside smaller circle) (magnification1000X). c) Bone marrow imprint (magnification 400X). d) Bone marrow aspirate show myeloblast (inside continous circle) and collection of monocytes (inside broken circle) (magnification 400X).
Discussion
Methotrexate (MTX) is an anti-metabolite agent which acts through inhibition of dihydrofolate reductase, causing disruption of the folic acid cycle and interference of DNA synthesis and repair and used as a first-line treatment for rheumatoid arthritis (RA) [1,2]. There are various systemic and local adverse effects of methotrexate among which gastrointestinal side effects are the commonest. Haematological side effects like lymphoma or Acute Myeloid Leukaemia (AML) have also been reported secondary to MTX, ranging 4.5 % to 25 % [3–5]. Till date, 15 cases of AML following methotrexate have been reported [6]. The present case is in addition to that. The age of these patients ranged from 35 to 83-year-old with a median age of 65-year-old and the sex ratio F/M was 2:1. All reported cases were treated by low dose MTX for RA (15 cases) or psoriasis (1case); with a weekly dose ranging from 5mg to 12.5mg/ week. Cumulative dose ranges were from 80mg to 9600 mg. The primary disease lasted for 0.25 year to 33 years. Our patient, a 70-year-old female who had RA for 20 years and was treated with 10 mg weekly dose of methotrexate with a cumulative dose of 9600 mg.
Various studies by Anoun S, Dubin K and Kolte B et al., suggested that methotrexate has a causal relationship with leukaemia [6–8]. Similarly, Goldin et al., in their study reported that there is significantly increased risk of AML and MDS associated with a prior history of autoimmune disease and the risk for AML is increased by 70% in patients who had any autoimmune disease [9].
Therapy related-Acute myeloid leukaemia is nearly 10% of total AML and it is a well known complication in patients with chronic malignancies and on various anticancer drugs [10]. According to Godley et al., the duration of development of therapy-related leukaemia and its features depends upon the exposure to specific agents and the total dose of the drug therapy after a primary diagnosis [11]. Also, Seedhouse et al., in their study suggested that heriditary predisposition to the development of t-AML, such as altered drug metabolism or DNA repair may also play a role [12]. Various animal experiments have also shown the oncogenic potential of Methotrexate especially in combination with cyclophosphamide on haematopoetic system [13].
But in contrast, numerous studies have shown that inflammatory cells which are increased in rheumatoid arthritis and other autoimmune diseases, produces tumour-associated antigens which could be the cause of leukaemia [14]. Another Study by Kristinsson et al., reported that history of any autoimmune disease increases risk for AML by 1.7 times and MDS by 2.1 times [15]. Thus, we need various in vitro experimental studies and good evidences to prove the causal relationship between the two.
Conclusion
In the present case it is difficult to conclude that AML is therapy related (methotrexate induced) or just an association with the primary autoimmune disease i.e rheumatoid arthritis. But looking at the fact that leukaemia is derived from rapidly proliferating hematopoietic cells which are particularly sensitive to changes in the intracellular folate levels which have the greatest requirements for DNA synthesis, they are likely to be affected by the metabolic rate of folic acid. Along with that out of total 16 cases, four cases had myelodysplasia which further transformed to AML, we could hypothesize that MTX use might be accompanied by an increased relative risk of developing MDS, which can be transformed into AML. Also, there has been a general agreement that patients with t-AML have shorter survivals than patients with de novo AML, thus frequent complete haemogram should be done while patient is on anti-metabolites such as methotrexate and physicians should be aware of this fatal complication.
[1]. Al-Anazi KA, Eltayeb KI, Bakr M, Al-Mohareb FI, Methotrexate-Induced Acute Leukaemia: Report of Three Cases and Review of the LiteratureClinical Medicine: Case Reports 2009 2:43-49. [Google Scholar]
[2]. Cronstein BN, Low-dose methotrexate: a mainstay in the treatment of rheumatoid arthritisPharmacol Rev 2005 57(2):163-72. [Google Scholar]
[3]. Choi BR, Ahn MJ, Lee WS, Kim TH, Bae SC, Jun JB, Acute erythroleukaemia in a rheumatoid arthritis patient during low-dose methotrexate therapyRheumatol Int 2005 25(4):311-13. [Google Scholar]
[4]. Mariette X, Cazals HD, Warszawki J, Liote F, Balandraud N, Sibilia J, Lymphomas in rheumatoid arthritis patients treated with methotrexate: A 3-year prospective study in FranceBlood 2002 99:3909-15. [Google Scholar]
[5]. Buhroo AM, Baba AN, Adverse Effects of Low-Dose Methotrexate in Patients with Rheumatoid ArthritisIJPMR 2006 17(2):21-25. [Google Scholar]
[6]. Anoun S, Lamchahab M, Qachouh M, Benchekroun S, Quessar A, A Case of Acute Myeloid Leukaemia Caused by Low Dose Methotrexate Used to Treat a Rheumatoid Arthritis PatientIJBC 2013 1:25-28. [Google Scholar]
[7]. Kolte B, Baer AN, Sait SN, O’Loughlin KL, Stewart CC, Barcos M, Acute myeloid leukaemia in the setting of low dose weekly methotrexate therapy for rheumatoid arthritisLeuk Lymphoma 2001 42(3):371-78. [Google Scholar]
[8]. Dubin KL, Troy K, Isola L, Temporal association between the use of methotrexate and development of leukaemia in 2 patients with rheumatoid arthritisJ Rheumatol 1995 22(12):2356-58. [Google Scholar]
[9]. Goldin LR, Kristinsson SY, Liang XS, Derolf ÅR, Landgren O, Björkholm M, Familial Aggregation of Acute Myeloid Leukaemia and Myelodysplastic SyndromesJournal of Clinical Oncology 2012 30(2):179-83. [Google Scholar]
[10]. Ramadan SM, Fouad TM, Summa V, Hasan SK, Lo-Coco F, Acute myeloid leukaemia developing in patients with autoimmune diseasesHaematologica 2012 97(6):805-17. [Google Scholar]
[11]. Godley LA, Larson RA, Therapy-related Myeloid LeukaemiaSeminars in oncology 2008 35(4):418-29. [Google Scholar]
[12]. Seedhouse C, Russell N, Advances in the understanding of susceptibility to treatment-related acute myeloid leukaemiaBr J Haematol 2007 137:513-29. [Google Scholar]
[13]. Zimecki M, Artym J, Effect of methotrexate on the immune response in selected expeimental modelsPostepy Hig Med Dosw 2004 58:226-35. [Google Scholar]
[14]. Szekanecz E, Andras C, Sandor Z, Malignancies and soluble tumour antigens in rheumatoid arthritisAutoimmun Rev 2006 6:42-47. [Google Scholar]
[15]. Kristinsson SY, Björkholm M, Hultcrantz M, Derolf AR, Landgren O, Goldin LR, Chronic immune stimulation might act as a trigger for the development of acute myeloid leukaemia or myelodysplastic syndromesJ Clin Onco 2011 29:2897-903. [Google Scholar]