Trigeminal Neuralgia (TN) is considered as one of the most painful neurologic disorders affecting oro-facial region. TN is often diagnosed clinically based on the patients complete history of pain (severity, duration, episodes etc), relief of pain on test dose of Carbamazepine, regional block of long acting anaesthetic. However, Magnetic Resonance Imaging (MRI) plays an important and confirmatory role in showing Neuro Vascular Conflict (NVC) which is the commonest causative factor for TN. This article reviews the effectiveness of three-dimensional constructive interference in steady-state (3D-CISS) MRI in diagnosing the exact location, degree of neurovascular conflict responsible for classical as well as atypical TN and possible pre-treatment evaluation and treatment outcome.
Introduction
Trigeminal neuralgia (TN) is the most common facial neuralgia, with a reported prevalence of 3–6 per 1,00,000 [1,2]. It is commonly seen in elderly adults in 5th to 7th decades of life with definite female predilection [2]. The classical and characteristic feature of TN is a paroxysm of pain, which is short, severe in episodes and exclusively unilateral along the course of trigeminal nerve, with more predilections towards the right side. The pain is typically located in the maxillary and mandibular divisions and rarely involves ophthalmic division. In about 3% of the cases, pain is bilateral [2,3] which suggests a secondary origin.
History
The first adequate description of TN was given in 1671, followed by a fuller description by physician John Locke in 1677. Andre described the convulsive-like condition and named it as Tic douloureux, John Hunter more clearly described the entity as a form of "nervous disorder" rather than pain of odontogenic origin [4,5].
Generally, neuralgia is a symptom of another disease, especially a space-occupying lesion compressing the trigeminal nerve on its way from the pons to the Gasserian ganglion (5 to 8% of patients) or vascular compression at the root entry zone at the cerebello pontine angle. According to Dandy, vascular compression was found in patients with paroxysomal facial pain at the root of the 5th nerve at cerebello pontine angle in 45% of 215 patients [6]. In case of a space-occupying lesion, diagnosis with the help of CT and MRI is more validated. Gardner and Miklos in 1959 developed neurovascular decompression of the nerve in the cerebellopontine angle as a non-destructive surgical treatment for TN [7]. There were controversies for the confirmation of neuro vascular compression as a causative factor for facial pain at operative times. The published figures show neuro vascular compression ranges from 10% to nearly 100%. The need of the hour is a proper diagnostic method to rule out aetiology underlying this suicidal pain.
Discussion
Clinical features
TN is characterized by episodes of paroxysmal sharp and shooting electric shock like pain along the trigeminal nerve distribution. Usually pain is unilateral in 97% of cases affecting right side of the face more commonly than the left side. It is more commonly seen to occur in elderly people in 5th to 7th decades of life with definite female predilection. The pain is more commonly located in the maxillary or mandibular divisions and ophthalmic division accounting for only 5% [8,9]. Trigger factors such as brushing teeth, eating, shaving or washing the face and even exposure to mild air breeze may precipitate the attack [8]. According to Fardy and Patton, the diagnosis of TN is important to perform the analgesic block, rapidly stopping the pain and triggering due to the occurrence of these in the area of the affected nerve [10]. The diagnosis of TN is mainly based on clinical signs and symptoms mentioned by the patient, as typical paroxysms, refractory periods and trigger zones. Olesen proposed few criteria for diagnosis of TN such as the paroxysmal attacks that last for few seconds to less than two minutes, pain presenting over one or more branches of the trigeminal nerve, sudden, intense, sharp, superficial, stabbing pain of great intensity, pain is precipitated from trigger areas or by certain activities like eating, talking, washing face or brushing teeth and the patient is completely asymptomatic between paroxysmal attacks [10].
Krafft concluded that the diagnosis of trigeminal neuralgia is essentially clinical and in patients who have unusual characteristics such as bilateral symptoms, dizziness or vertigo, age less than 40 years, hearing loss or disorder, episodes of pain with longer than two minutes, evaluations of image or specialized tests is required [10]. First reports of successful use of MRI in detecting vascular compressions were given by Tash et al., in 1989 [11]. Meaney and colleagues developed a specific technique to optimally image the relationship of the nerve and the blood vessels in its vicinity (magnetic resonance tomographic angiography) [12]. Recent advances in MRI such as 3D CISS (3D Constructive Interference in Steady State) led us to know the detailed visualization of underlying nerve compression in trigeminal neuralgia.
3D CISS
CISS which stands for Constructive Interference in Steady State, is a part of fast gradient echo sequences and considered to be superior to the conventional plain MRI [13] CISS is used in the assessment of the anatomical variations and various pathologies involving the cranial nerves and central nervous system [14]. CISS has been shown to be useful in spinal imaging, especially in cases of arterio-venous malformation. The main roots of trigeminal nerve and the gasserian ganglion can be finely depicted by CISS in the pre-pontine cistern and in Meckel’s cave, respectively [15]. In cases of TN, CISS plays an important role in searching for vascular compressions [16].
In a comparative study between 3D CISS MR imaging and Magnetic Resonance (MR) angiography conducted by Norio Yoshino et al., they concluded that 3D CISS MR imaging with Multi Planar Reconstruction (MPR) is useful in the detection of NVC in patients with TN, compared with MR angiography [17]. A 3D CISS imaging offers high spatial resolution and excellent contrast resolution and depicts both the artery and the vein responsible for the NVC. Furthermore, a close relationship was found between the region of neuralgic manifestation, distribution of the corresponding trigeminal branch fibres and the site of the vascular compression in the trigeminal nerve [17].
MR angiography showed greater contrast between different anatomical structures such as artery and nerve. However, 3D CISS is superior in depicting the venous architecture more clearly than the MR angiography. A 3D CISS also provides high spatial resolution with clear and enhanced contrast resolution between the nerve root and cerebrospinal fluid [17]. The underlying rationale for selection of 3D CISS over the conventional MRI is the high gradient amplitude & slow rates. These three dimensional images with MPR provides us source images with superior contrast and spatial resolution. High strength magnets are employed to reach the maximum intensity within short period of time [14].
Mechanism of Action
CISS is considered as green sequence i.e., the decaying signal from transverse magnetic plan is not wasted in radio frequency pulse. This decaying signal is responsible for the T2 images of a tissue. The decaying signal from transverse magnetization field is recycled by applying 1800 phase shift during every repetition time period, simultaneously the tipping of residual transverse magnetization field occurs along Z axis and longitudinal into X axis. After many cycles of repetition period the feeding of longitudinal and transverse planes & vice versa, equilibrium state is achieved in both transverse and longitudinal planes [14].
Repetition time period is always kept shorter than the T2 relaxation time so that there is insufficient time for the decay of transverse magnetization before the next radiofrequency pulse excitation. CISS is a kind of a fully refocused fast gradient echo sequences, which has both pre and post excitation signals which results in getting high signal to noise ratio and high spatial resolution [18].
Rationale of 3D CISS in Diagnosing Trigeminal Neuralgia
MRI is unique as it produces images of the entire course of the trigeminal nerve and even the cisternal segment. As mentioned earlier about the advantages of its ability to differentiate between artery and nerve is mainly helpful in locating the NVC which stands as a main causative factor for TN. So, 3D CISS helps in mainly determining the aetiology associated with the TN and also the extent of NVC [19,20]. NVC in the cranial location shows pain along the distribution of ophthalmic branch and involvement in the caudal region shows symptoms along mandibular division. A 3D CISS MRI not only helps in identification of such neurovascular relationships and atypical distributions of TN but also helps in pre-surgical planning and possible outcome after surgery. Possible aetiology for the TN can be assessed with the preoperative MRI [13]. Neurovascular compression is graded on MRI based on the extent of the compression of the nerve and vessel [20].
Grade I Mild contact with nerve & vessel.
Grade II Mild distortion /displacement of the nerve root by artery.
Grade III Marked indentation of the nerve root by the vessel.
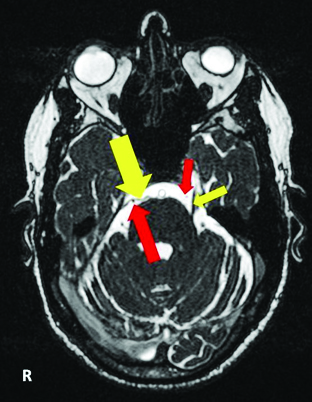
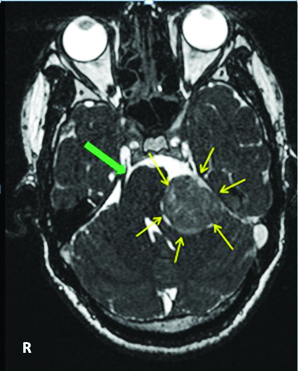
MRI plays an important role in diagnosing Grade I, II and III neurovascular conflict. The use of 3D CISS MR imaging which has advantages such as high spatial resolution and contrast between the structures allows for the in depth study of the anatomy of trigeminal nerve. A 3D MRI with CISS which has the advantages of high spatial resolution and excellent contrast between the structures allows us to know the anatomy of trigeminal nerve, cerebello pontine angle & inner ear and root entry zones of trigeminal nerve [Table/Fig-1&2].
MRI 3D CISS image on axial sections showing normal trigeminal nerve course marked in short yellow arrows and position of normal superior cerebellar artery marked in short red arrows on the left side. Whereas on the opposite side neurovascular compression of the trigeminal nerve (showed in large yellow arrows) by superior cerebellar artery marked in red.
MRI 3D CISS image on axial sections showing normal trigeminal nerve course marked in green arrow and on opposite side showed a well defined hyper intense, enhancing lesion in the left cerebello pontine angle marked in yellow arrows, causing compression of the trigeminal nerve, which was later diagnosed as Vestibular Schwannoma histopathologically.
Conventional MR Angiography shows artery as high signal, nerve as intermediate and cerebrospinal fluid as low signal but 3D CISS imaging show blood vessel & nerve appears as low signal, Cerebrospinal Fluid (CSF) as high signal intensity which shows that 3D CISS imaging has high contrast resolution between these anatomic structures [16]. Neurovascular conflict is common intracranial causative factor for TN, of which superior cerebellar artery is the commonly found artery which compresses the trigeminal nerve in quarter of cases reported followed by anterior inferior cerebellar artery, basilar artery in decreasing order [20]. Rarely the veins are also responsible for the nerve compression at root entry zone. The conventional MR angiography could not localize or detect neurovascular compression by the vein providing the inadequate information. However, the 3D CISS MRI provided the information regarding the location and degree of compression by the vein.
Advantages
Reasonably long T2 relaxation times will demonstrate additional signal due to various refocused echo paths [12].
Highest possible signal-to-noise ratio per unit time among all known sequences [13].
Increased signals and improved speed of acquisition.
Steady-state sequences have the advantage of speed that reduces motion artefacts from respiration and peristalsis [14].
Disadvantages
1. Expensive when compared to conventional MRI scan.
Availability
It is readily available in all MRI machines as CISS is a modification of conventional MRI machine [15]. Any high strength MRI machine above ≥ 1.3 Tesla can produce CISS images. CISS has different names according to different brands and manufacturers, a few are mentioned below:
Fast imaging employing steady-state acquisition (FIESTA) by GE,
True fast imaging with steady-state precession (FISP) by Siemens,
Balanced fast field echo (FFE) by Philips,
True steady-state free precession (SSFP) by Toshiba.
Economic factor
MRI is cost effective, either conventional or CISS when compared to other diagnostic imaging modalities. Conventional MRI of brain costs around 400$ with another 100$ for the radiologist. In India, 3D CISS MRI is readily available around all the major educational and corporate centres with cost ranging from 6500-7500 INR, whereas plain MRI costs around 5000 INR. Though 3D CISS MRI is expensive when compared to plain MRI, but the diagnostic efficacy of 3D CISS MRI stands superior over conventional MRI in depicting the aetiology and site of NVC more clearly.
Other Clinical applications
It is used in the evaluation of cartilage and meniscal lesions, brain haemorrhages, cardiac imaging to assess the myocardial viability, pericardial diseases and congenital heart diseases, abdominal imaging, fetal and interventional imaging for needle path guidance [15].
Conclusion
Despite recent advances in diagnosis and management, Trigeminal neuralgia still remains a severe neurologic disorder manifested as severe unilateral oro-facial pain along the distribution of the nerve. Although there are no specific clinical tests for diagnosing trigeminal neuralgia, MRI still stands as lone imaging modality for diagnosing this disorder. A 3D CISS MRI acts as an adjuvant to conventional MR angiography and superior to it in contrast, visualising the location, degree of exact neurovascular conflict and veins which cause compression are also visualized in 3D MRI CISS than in plain MRI.
[1]. Yoshimasu F, Kurland LT, Elveback LR, Tic douloureux in Rochester, MinnesotaNeurology 1972 22:952-56. [Google Scholar]
[2]. Katusic S, Beard CM, Bergstralh E, Kurland LT, Incidence and clinical features of trigeminal neuralgia, Rochester, MinnesotaAnn Neurol 1990 27:89-95. [Google Scholar]
[3]. Fromm GH, Steven B, Graff-Radford Terrence CF, Sweet WH, Pre-trigeminal neuralgiaNeurology 1990 40:1493-95. [Google Scholar]
[4]. Pearce JMS, Historical note Trigeminal neuralgia (Fothergill’s disease) in the 17th and 18th centuriesJ Neurol Neurosurg Psychiatry 2003 74:1688 [Google Scholar]
[5]. Fothergill J, Of a painful affection of the faceMedical observations and inquiries by a society of physicians 1773 5:129-42. [Google Scholar]
[6]. Dandy WE, Concering the cause of trigeminal neuralgiaAm J Surg 1934 24:447-55. [Google Scholar]
[7]. James Gardner W, Miklos MV, Response of trigeminal neuralgia to "decompression" of sensory root discussion of cause of trigeminal neuralgiaJAMA 1959 170:1773-76. [Google Scholar]
[8]. Sjaastad O, Pareja JA, Zukerman E, Jansen J, Kruszewski P, Trigeminal neuralgia: clinical manifestations of first division involvementHeadache 1997 37:346-57. [Google Scholar]
[9]. Yu AC, Sweeney PJ, Cranial neuropathies. In: Katirji B, Kaminski HJ, Preston DC, Ruff RL, Shapiro B (eds)Neuromuscular disorders in clinical practice 2002 Boston–OxfordButterworth Heinemann:820-27. [Google Scholar]
[10]. Santos MM, Freire AR, Rossi AC, Prado FB, Caria PHF, Botacin PR, Trigeminal neuralgia: literature reviewJ Morphol Sci 2013 30:1-5. [Google Scholar]
[11]. Tash RR, Sze G, Leslie DR, Trigeminal neuralgia: MR imaging featuresRadiology 1989 172:767-70. [Google Scholar]
[12]. Meaney JF, Miles JB, Nixon TE, Whitehouse GH, Ballantyne ES, Eldridge PR, Vascular contact with the fifth cranial nerve at the pons in patients with trigeminal neuralgia: detection with 3D FISP imagingAJR Am J Roentgenol 1994 163:1447-52. [Google Scholar]
[13]. Gupta SK, Gupta A, Mahajan A, Gupta R, Tandon VR, Gupta N, Clinical Insights in Trigeminal NeuralgiaJK Science Clinical guide 2005 7:181-84. [Google Scholar]
[14]. Gonçalves FG, do Amaral LLF, Constructive interference in steady state imaging in the central nervous systemEuropean Neurological Review 2011 6:138-42. [Google Scholar]
[15]. Hingwala D, Chatterjee S, Kesavadas C, Thomas B, Kapilamoorthy TR, Applications of 3D CISS sequence for problem solving in neuroimagingIndian J Radiol Imaging 2011 21(2):90-97. [Google Scholar]
[16]. Yousry I, Moriggl B, Schmid UD, Trigeminal ganglion and its divisions: detailed anatomic MR imaging with contrast-enhanced 3D constructive interference in the steady state sequencesAJNR Am J Neuroradiol 2005 26:1128-35. [Google Scholar]
[17]. Yoshino N, Akimoto H, Yamada I, Trigeminal neuralgia: evaluation of neuralgic manifestation and site of neurovascular compression with 3D CISS MR imaging and MR angiographyRadiology 2003 228:539-45. [Google Scholar]
[18]. Chavhan GB, Babyn PS, Jankharia BG, Cheng HL, Shroff MM, Steady-state MR imaging sequences: physics, classification and clinical applicationsRadiographics 2008 28:1147-60. [Google Scholar]
[19]. Sindou M, Howeidy T, Acevedo G, Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict). Prospective study in a series of 579 patientsActa Neurochir 2002 144:1-12. [Google Scholar]
[20]. Harsha KJ, Kesavadas C, Chinchure S, Thomas B, Jagtap S, Imaging of vascular causes of trigeminal neuralgiaJ Neuroradiol 2012 39(5):281-89. [Google Scholar]